Ductal carcinoma in situ (DCIS) refers to a breast carcinoma limited to the ducts with no extension beyond the basement membrane, as a result of which the disease has not infiltrated the parenchyma of the breast and the lymphatics and cannot therefore metastasize.
On this page:
Epidemiology
The detection of ductal carcinoma in situ has increased markedly secondary to the widespread use of screening mammography, and it now accounts for 25-40% of mammographically detected breast cancers 1,3. It also accounts for approximately 15-20% of all detected breast cancers.
Associations
up to 11% of predetermined ductal carcinoma in situ on imaging may have an invasive component at the time a biopsy is done 2
20-25% of DCIS revealed on core biopsy may have invasive ductal carcinoma following surgical excision
Risk factors
Risk factors for ductal carcinoma in situ are similar to those for invasive carcinoma and include:
increasing age
family history of breast cancer
nulliparity
age of 30 years or older at the birth of the first child
Clinical presentation
Although most patients are asymptomatic, some present with nipple-related disease (nipple discharge or Paget disease of the breast) or have palpable abnormalities.
Pathology
Ductal carcinoma in situ (DCIS) is the non-obligate precursor of invasive breast carcinoma. In the context of "overdiagnosis" the low grade DCIS cases found on screening mammography are likely to cause the number of cases where the diagnosis of breast malignancy has been made but could conceivably not have been fatal to the patient. Remember that to try and guess the grade of DCIS on the mammogram images is not plausible or reproducible. Low grade DCIS is not a dangerous disease and there is actually some thought on following the disease with MRI after a histological diagnosis has been made.
Ductal carcinoma in situ is not a single entity, but rather a spectrum of disease 3. In essence, it refers to breast epithelial cells that have become "cancerous" but still reside in their normal place in the ducts and lobules 9.
Markers
In some situations, immunohistochemical staining for E-cadherin may help to differentiate from lobular carcinoma in situ.
Subtypes
The traditional classification broadly divided ductal carcinoma in situ lesions into two types mainly based on central necrosis, grade, and cell type:
comedo - large cell: more aggressive form; also referred to as comedocarcinoma
-
non-comedo - small cell: less aggressive; can be further divided into
cribriform
micropapillary
papillary
solid
A new pathological classification of DCIS is based on nuclear atypia and degree of necrosis.
Radiographic features
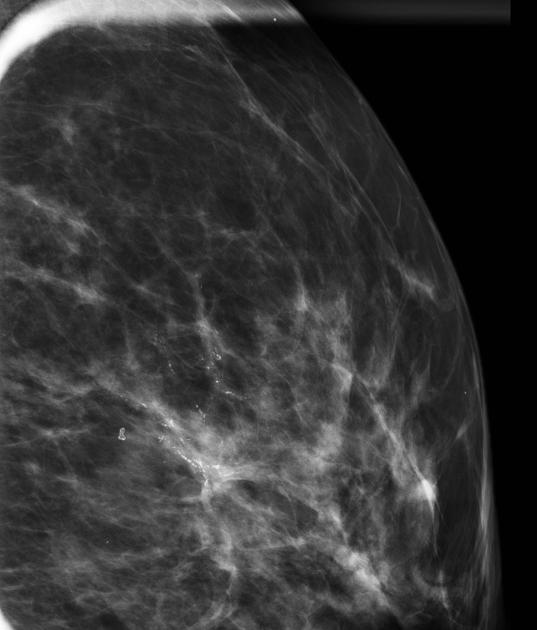
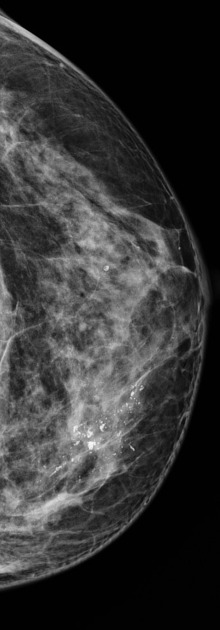
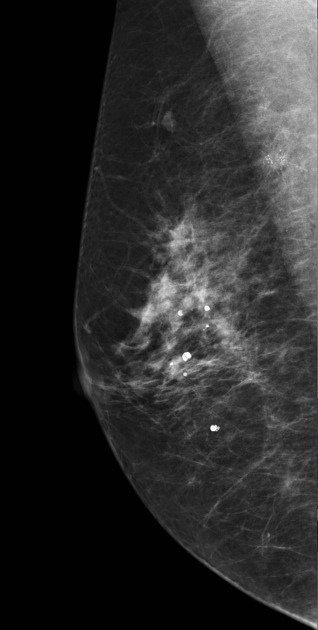
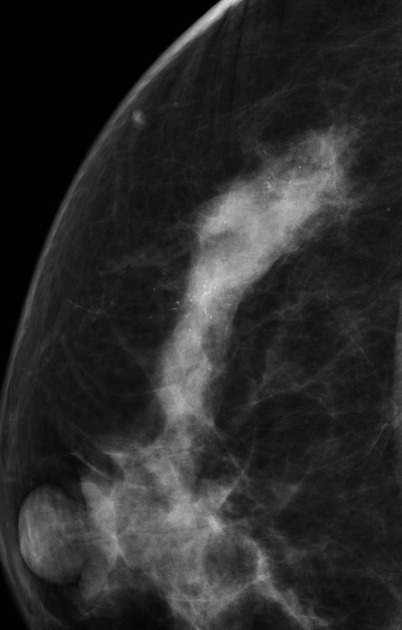
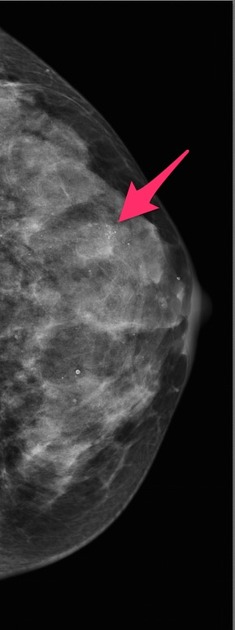
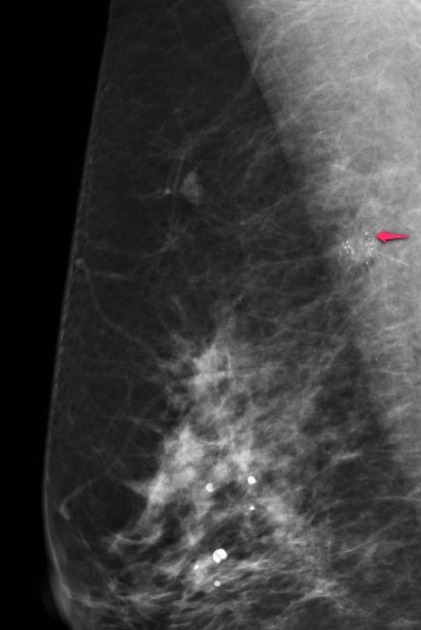
Mammography
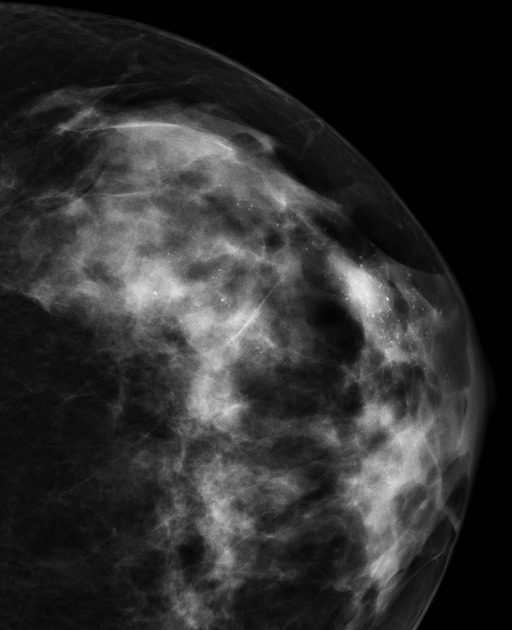
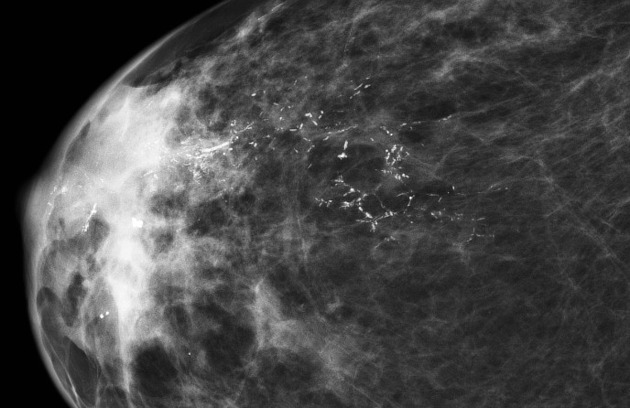
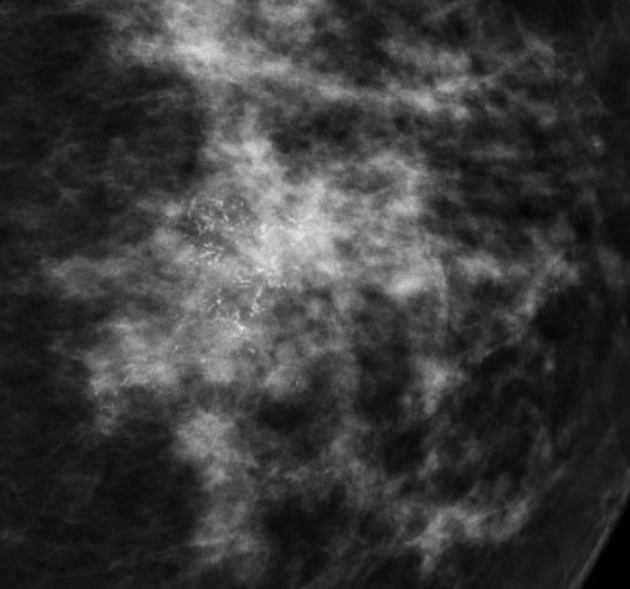
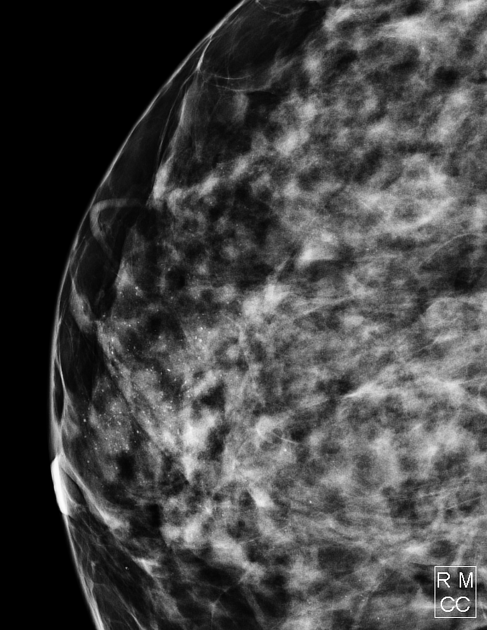
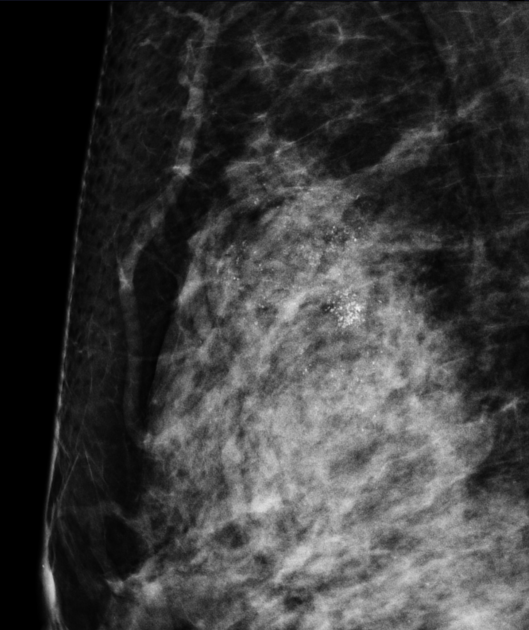
There are varied mammographic manifestations of ductal carcinoma in situ, with casting-type calcifications being the most common (present in 50-75% of cases 3). Other manifestations include a soft-tissue opacity either with or without associated calcifications.
Although DCIS calcifications may assume varied appearances, linear calcifications are more likely to be associated with comedo-type DCIS, while granular calcifications are more often correlated with non-comedo DCIS.
Occasionally DCIS appears as a simple mass or asymmetry without calcification (~8% of cases) 11.
There may be a significant discrepancy between the distribution of the disease as seen on the mammogram and the distribution of the disease on the pathology specimen of the breast as examined by the pathologist. In general, the calcification underestimates the distribution of DCIS in the breast, i.e. not all the DCIS calcifies.
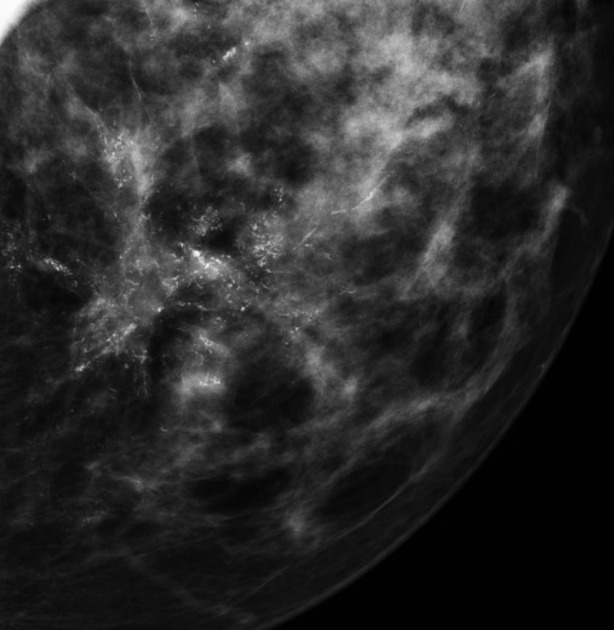
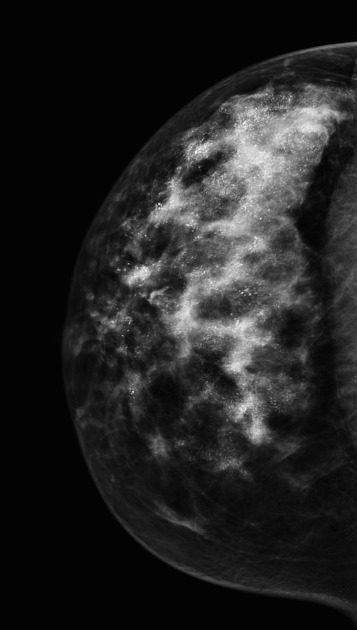
Breast ultrasound
One of the benefits of identifying a corresponding sonographic abnormality in women with mammographically detected DCIS is to use ultrasound to guide interventional (e.g. biopsy/hook wire) procedures. A microlobulated mild hypoechoic mass with ductal extension and normal acoustic transmission is considered the most common feature in sonographically detected DCIS.
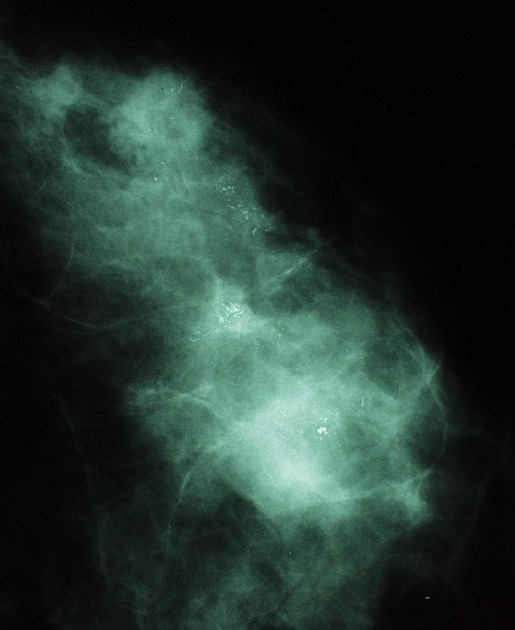
With good quality ultrasound and enough effort, it is possible in everyday practice to identify the DCIS process as it grows in the ductal system of the breast. It is quite possible to identify those minute wild and crazy calcifications of DCIS in the ducts itself and ultrasound-guided biopsy of DCIS is now an everyday procedure.
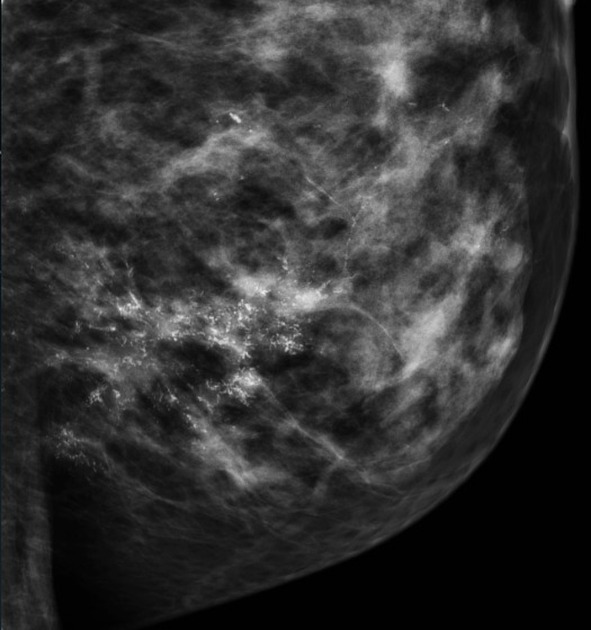
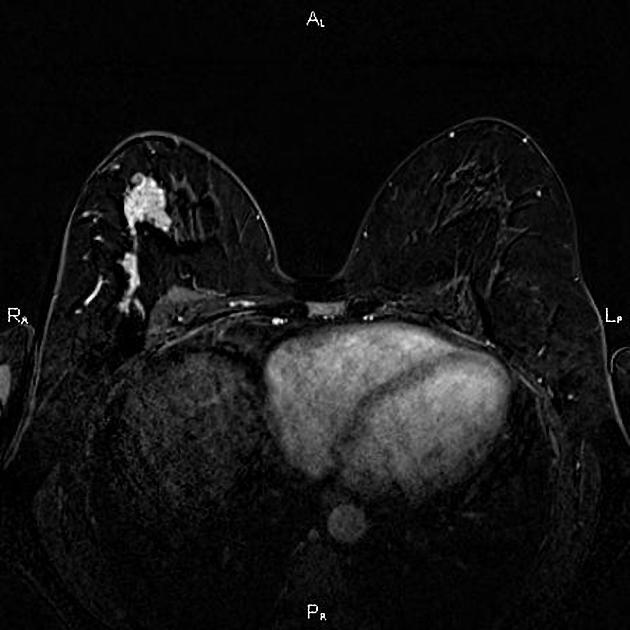
Breast MRI
DCIS most commonly appears as non-mass enhancement, most commonly with a segmental or linear distribution and clumped or heterogeneous internal enhancement pattern 13. Within non-mass enhancement, the clustered ring internal enhancement pattern is most specific for malignancy, usually DCIS 14.
Treatment and prognosis
Treatment options for ductal carcinoma in situ include mastectomy, lumpectomy with breast irradiation, or, for patients with small lesions (<1-2 cm) of low-grade DCIS, lumpectomy alone.
This disease is likely the precursor of invasive ductal carcinoma at a stage when the therapy is potentially curable. The advantage of diagnosis of DCIS is that the chances of encountering metastatic disease are in theory zero when compared to invasive ductal carcinoma. With the introduction of screening mammography, the decreased mortality of breast carcinoma is in some part due to the identification of DCIS and effective therapy. In large screening programmes, DCIS makes up to 30% of malignancies diagnosed.









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.