Gastric adenocarcinoma, commonly, although erroneously, referred to as gastric cancer, refers to a primary malignancy arising from the gastric epithelium. It is the most common gastric malignancy. It is the third most common GI malignancy following colon and pancreatic carcinoma.
On this page:
Epidemiology
Gastric cancer is rare before the age of 40, but its incidence steadily climbs after that (from 50 to 70 years) and peaks in the seventh decade of life, with males predominating at 2:1 2,10. The median age at diagnosis of gastric cancer in the United States is 70 years for males and 74 years for females.
Risk factors
-
Billroth II partial gastrectomy for benign disease (e.g. peptic ulcer disease)
reflux of bile and pancreatic juice as thought to be carcinogenic 8
type A blood group 9
smoking 10
Clinical presentation
It often produces no specific symptoms when it is superficial and potentially surgically curable, although up to 50% of patients may have nonspecific gastrointestinal complaints such as dyspepsia 2.
Patients may present with anorexia and weight loss (95%) as well as abdominal pain that is vague and insidious. Nausea, vomiting, and early satiety may occur with bulky tumours that obstruct the gastrointestinal lumen or infiltrative lesions that impair stomach distension 2.
Several nodal metastases with eponymous names associated with gastric cancer have been described:
Pathology
Adenocarcinoma is by far the most common gastric malignancy, representing over 95% of malignant tumours of the stomach 1. There are two types of gastric adenocarcinoma, intestinal or well-differentiated and diffuse or undifferentiated that have distinct morphologic, pathogenesis, and genetic traits 11.
Aetiology
Gastric cancer continues to be one of the leading causes of cancer-related death. A significant development in the epidemiology of gastric carcinoma has been the recognition of the association with Helicobacter pylori infection (~55% risk; range 46-63% 11). Most gastric cancers occur sporadically, whereas 8-10% have an inherited genetic component. A low vitamin A and C diet, large amounts of smoked foods consumption, and contaminated drinking water also increase the risk of gastric cancer. High body mass index (BMI), high-calorie foods, and gastro-oesophageal reflux are associated with an increased risk of the distal oesophageal segment, gastric proximal segment, and gastro-oesophageal junction adenocarcinoma 11.
Radiographic features
Endoscopy is regarded as the most sensitive and specific diagnostic method in patients suspected of harbouring gastric cancer. Endoscopy allows direct visualisation of tumour location, the extent of mucosal involvement, and biopsy (or cytologic brushings) for tissue diagnosis 3. But radiological methods are often the initial examination that raises suspicion for gastric carcinoma, besides being used in the staging of the disease.
Fluoroscopy
Early gastric cancer (elevated, superficial, shallow):
type I: elevated lesion, protrudes >5 mm into the lumen (polypoid)
type II: superficial lesion (plaque-like, mucosal nodularity, ulceration)
type III: shallow, irregular ulcer crater with adjacent nodular mucosa and clubbing/fusion/amputation of radiation folds 4
Advanced gastric cancer:
polypoid cancer can be lobulated or fungating
lesion on a dependent or posterior wall; filling defect in barium pool
lesion on non-dependent or anterior wall; etched in white by a thin layer of barium trapped between edge of mass and adjacent mucosa
ulcerated carcinoma (penetrating cancer): 70% of all gastric cancers 4
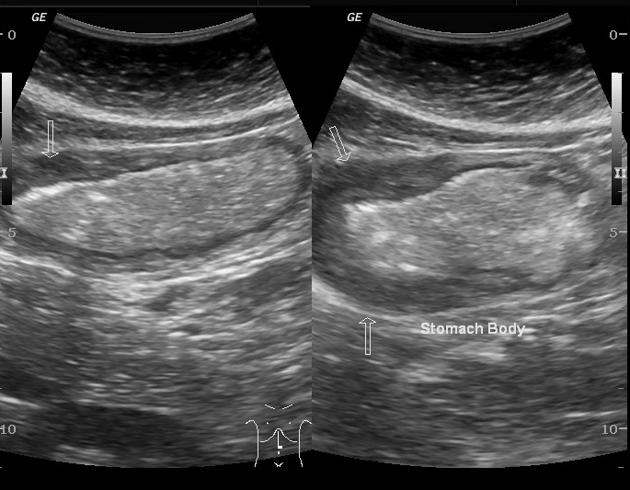
Ultrasound
Not useful, unless a large epigastric mass is present or in an endoscopic ultrasound study.
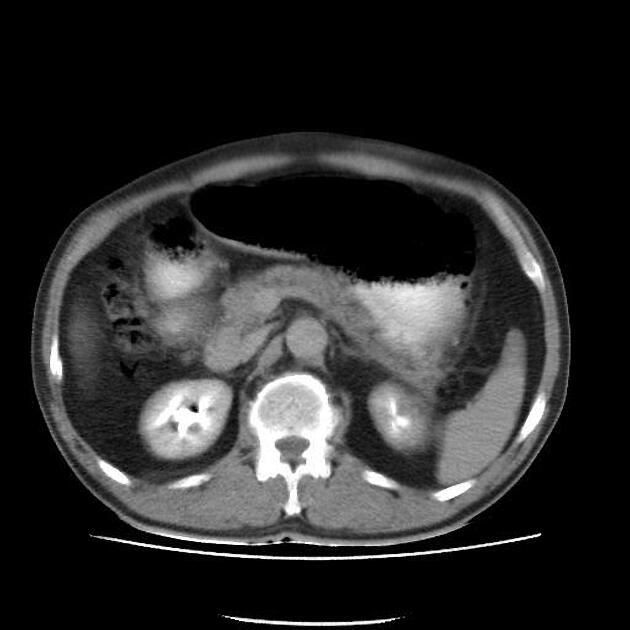
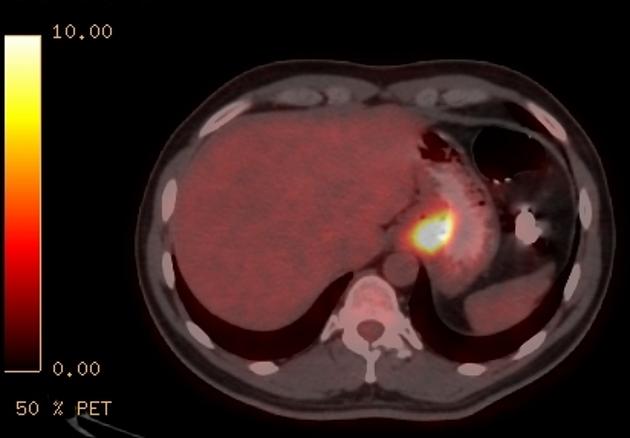
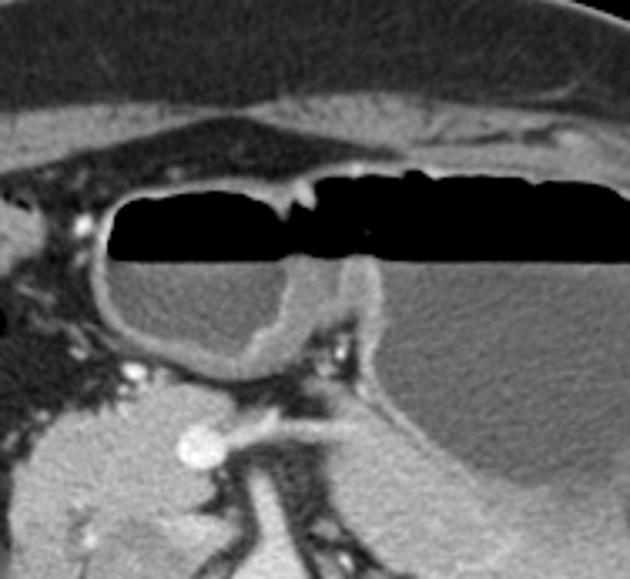
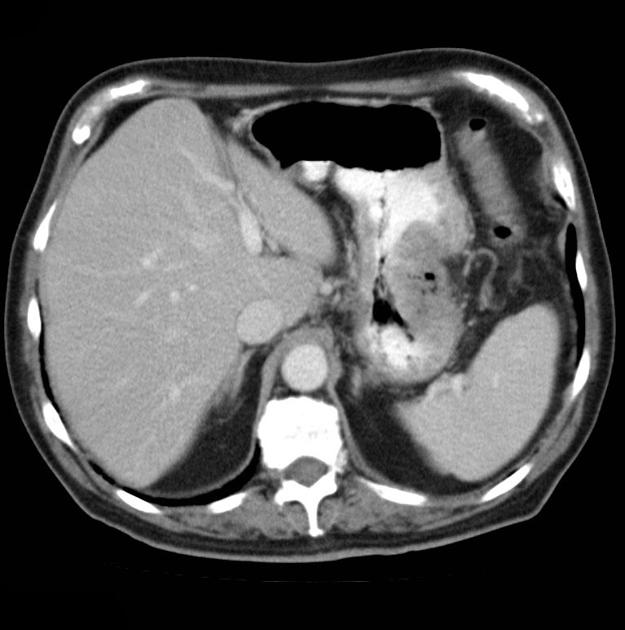
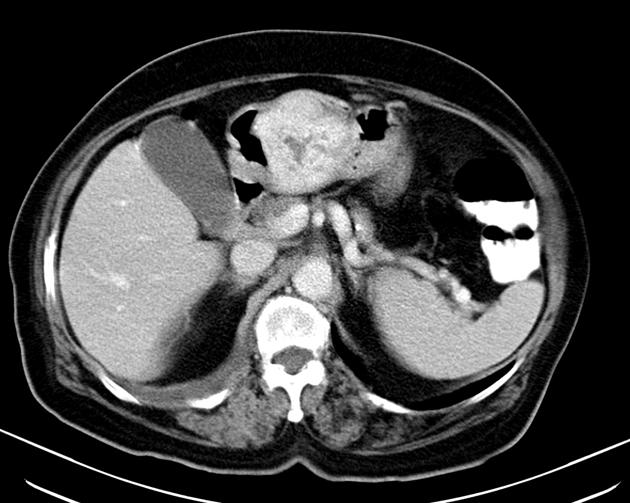
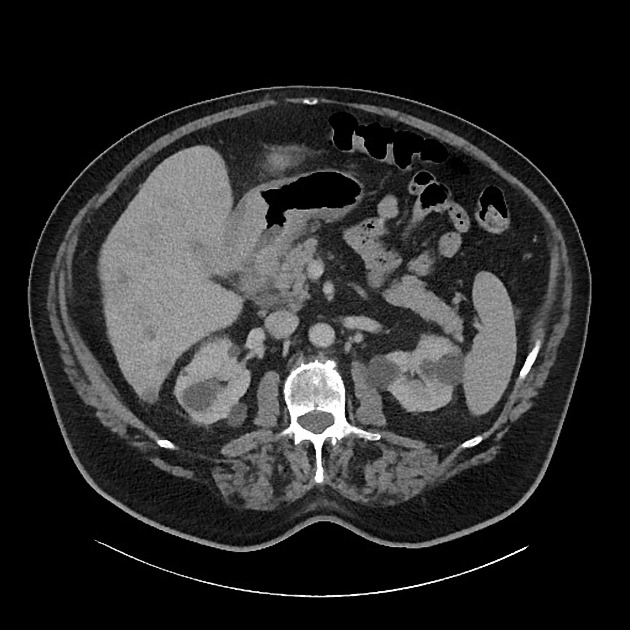
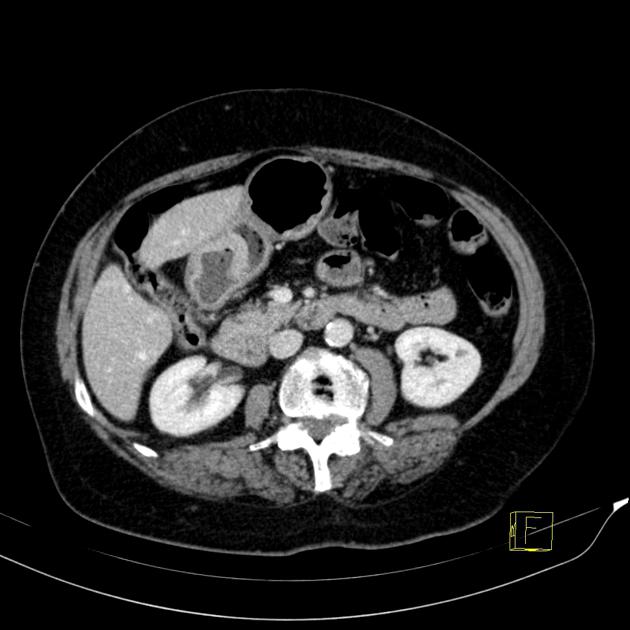
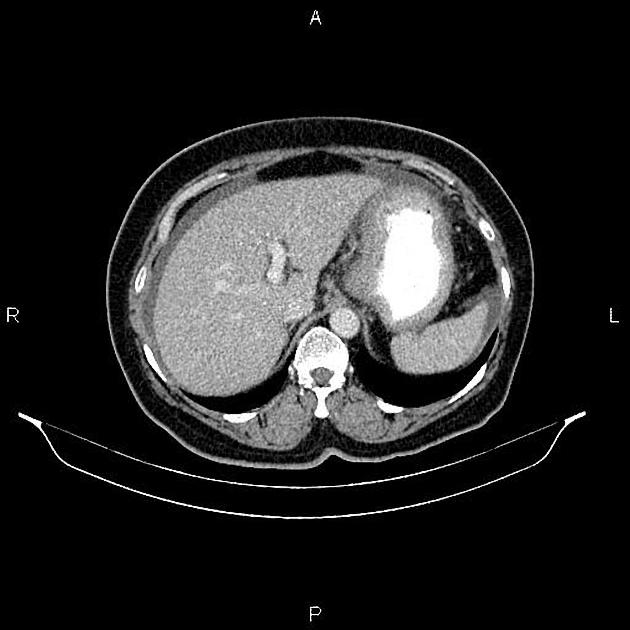
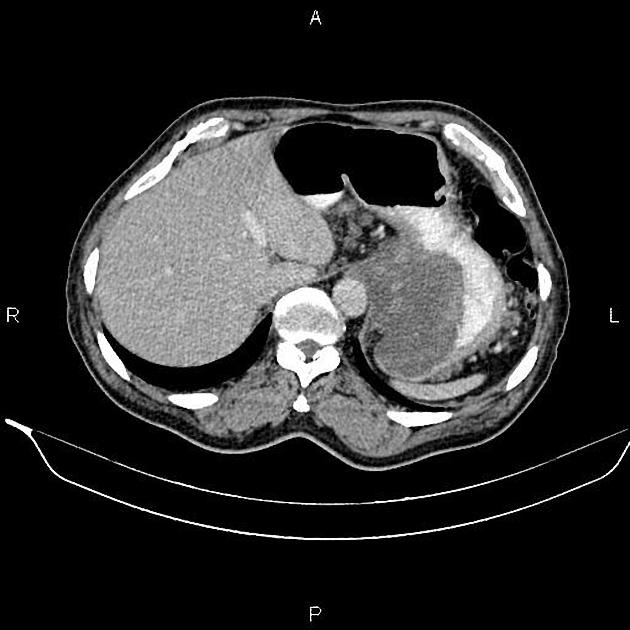
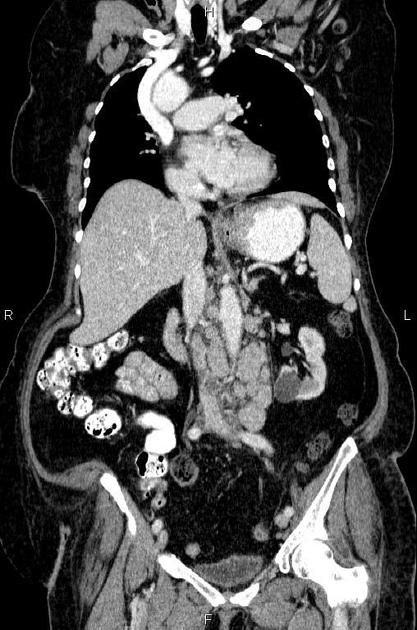
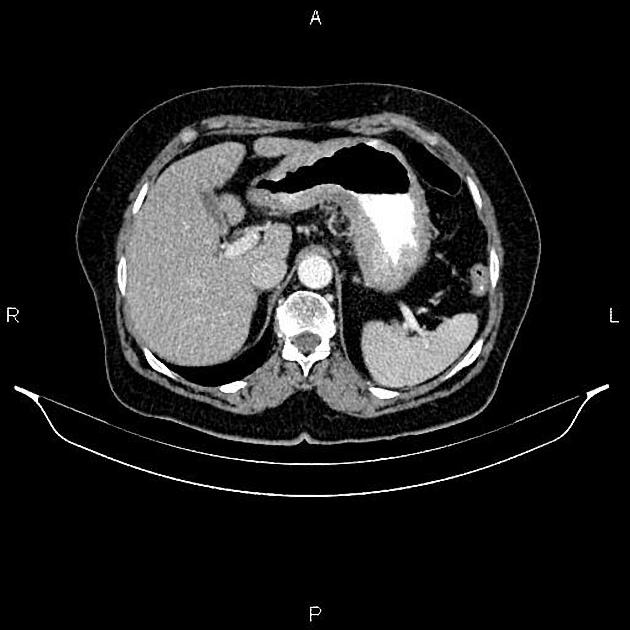
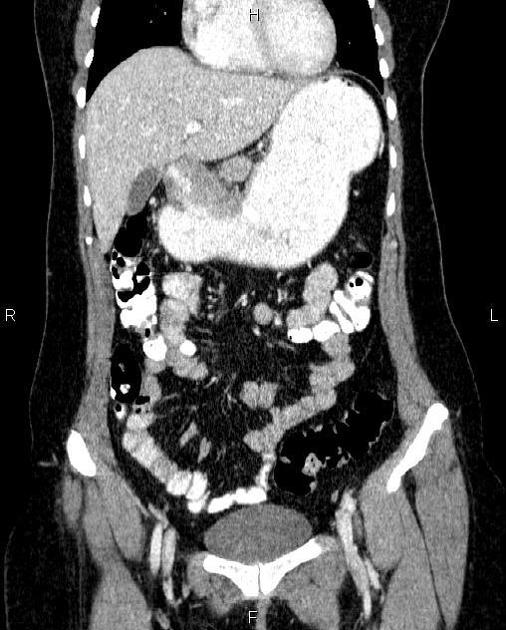
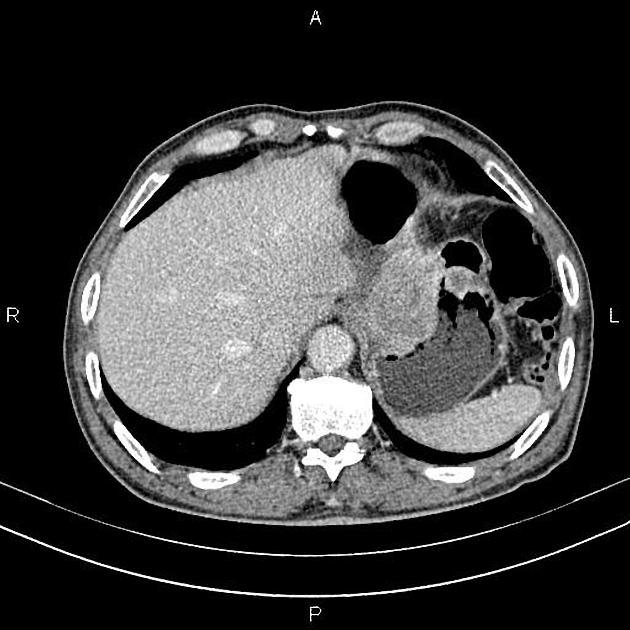
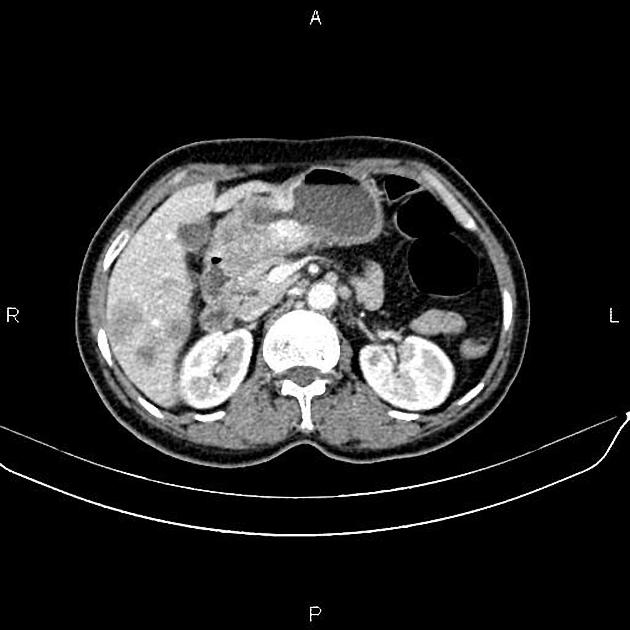
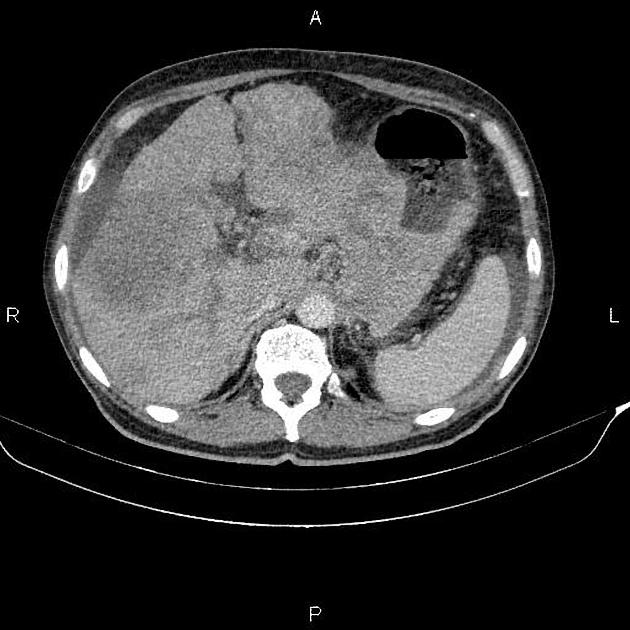
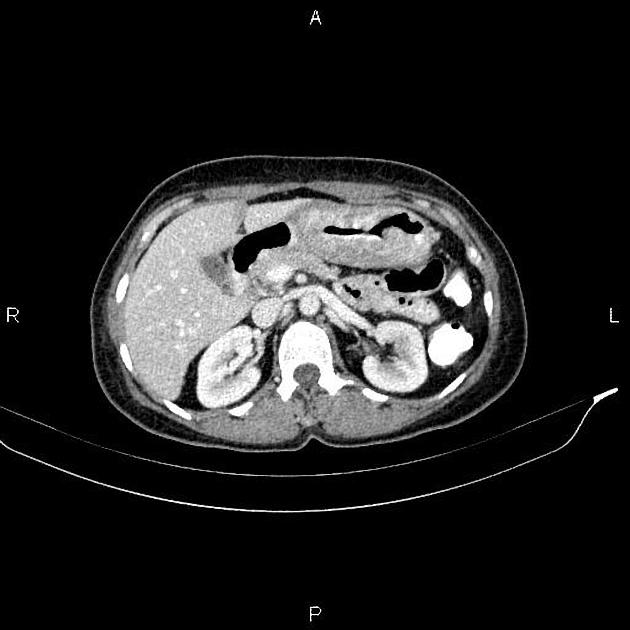
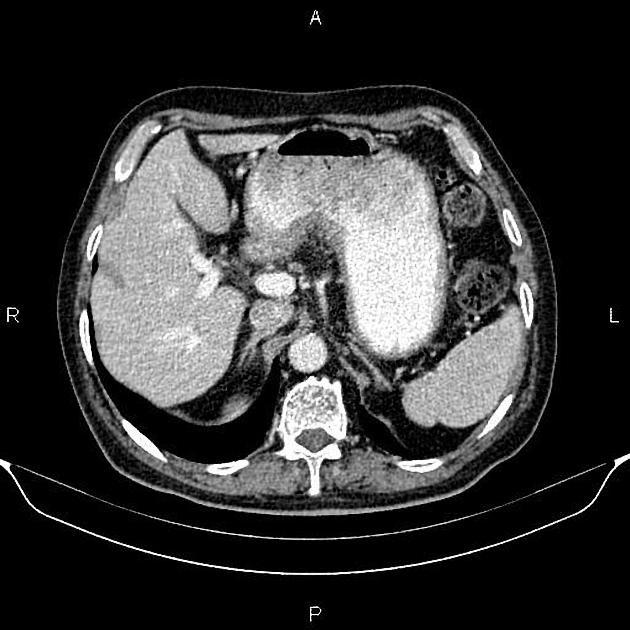
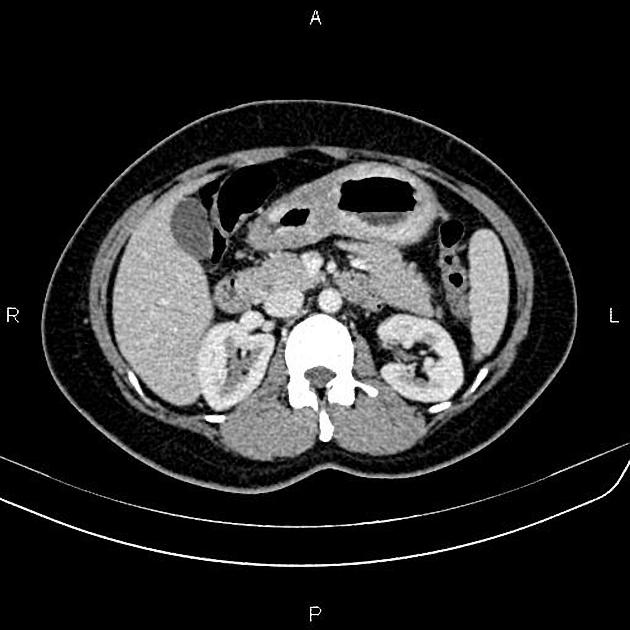
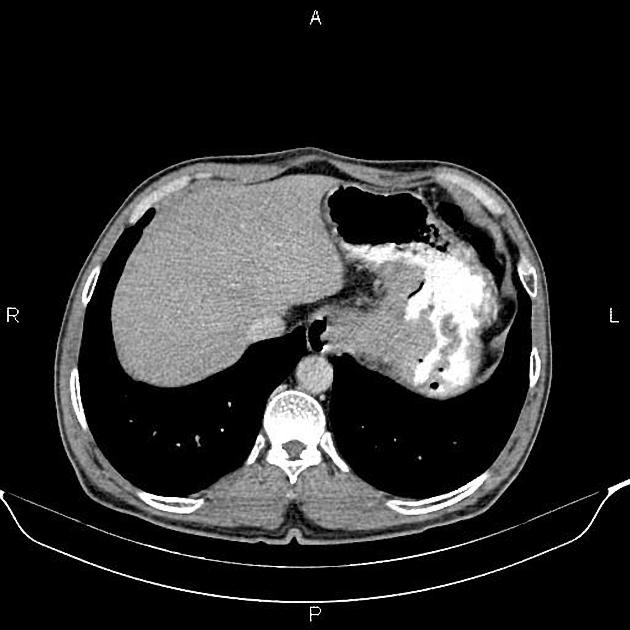
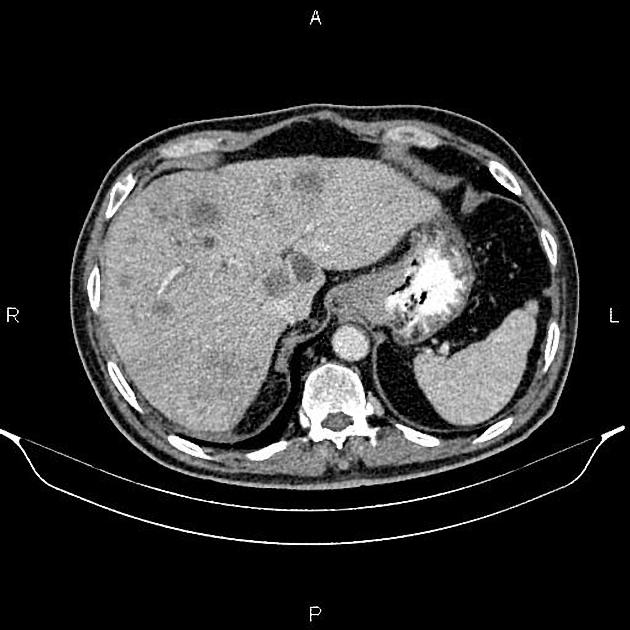
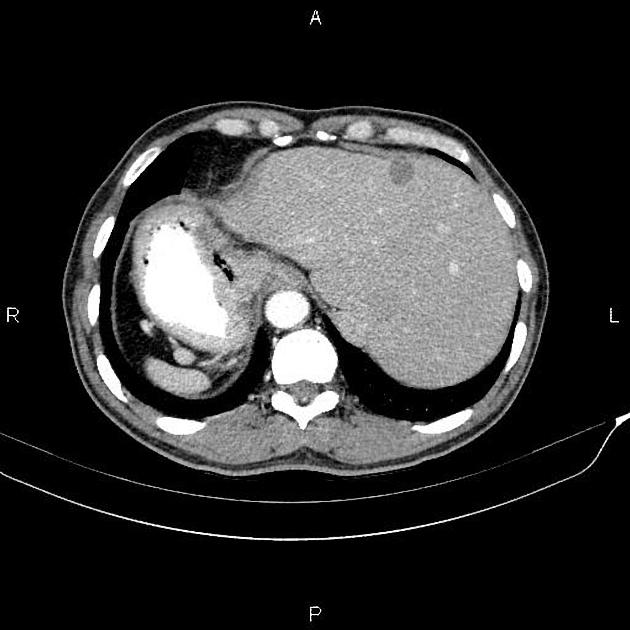
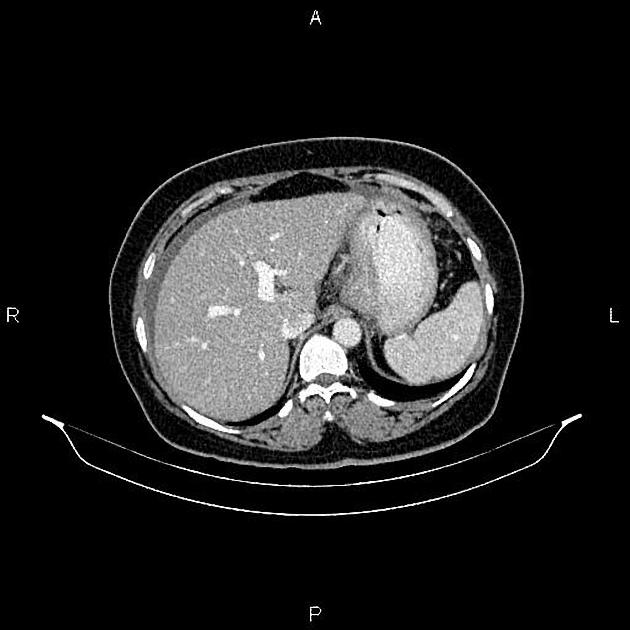
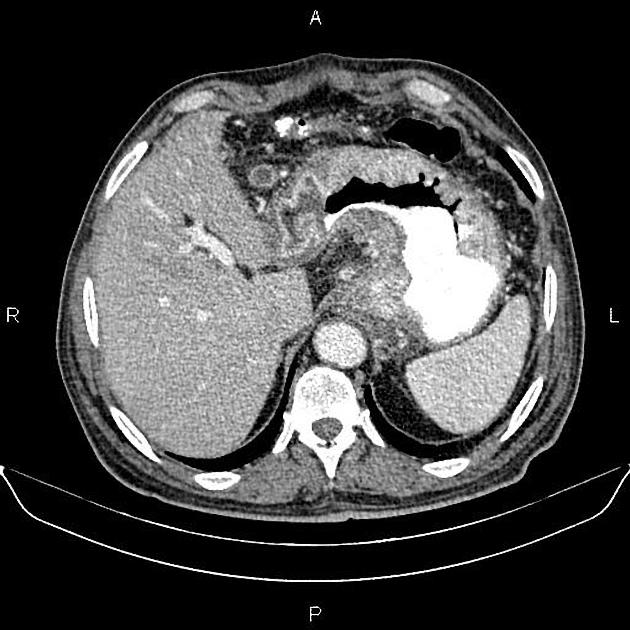
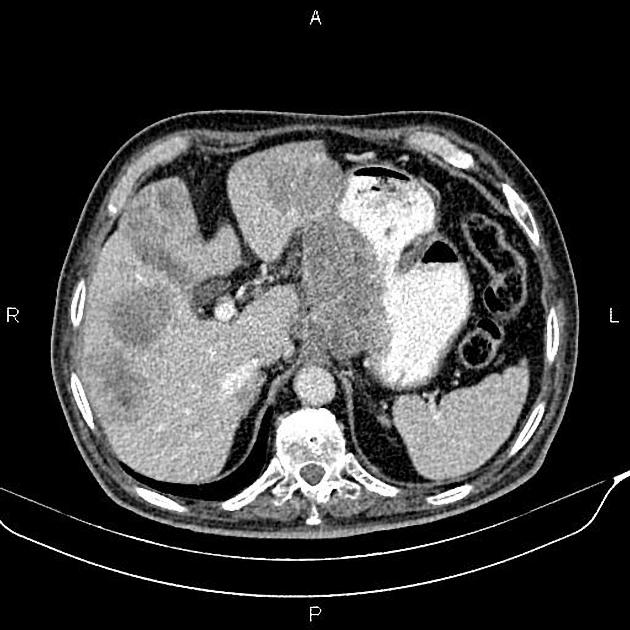
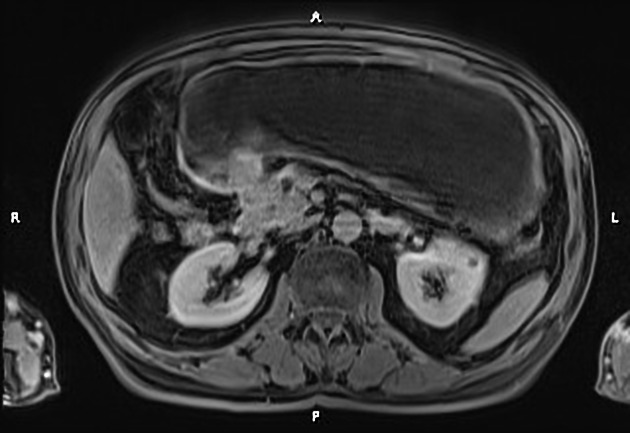
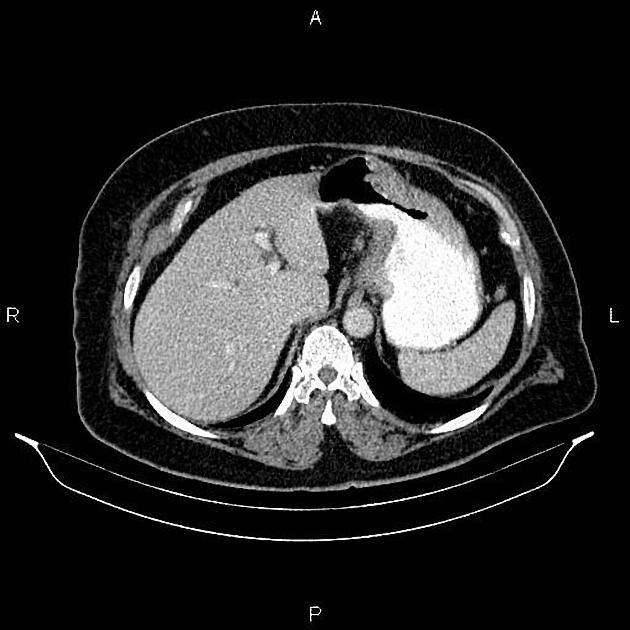
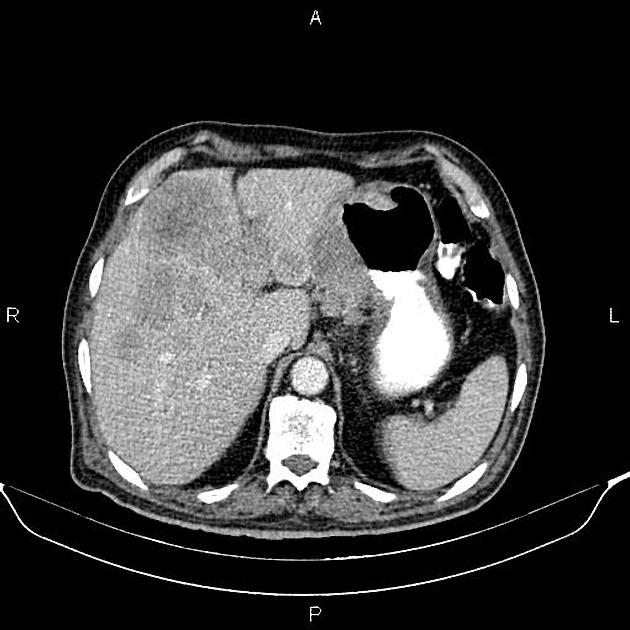
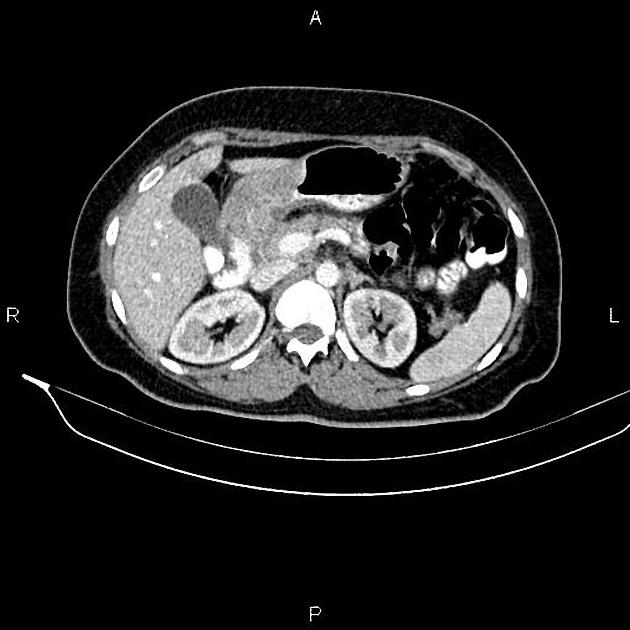
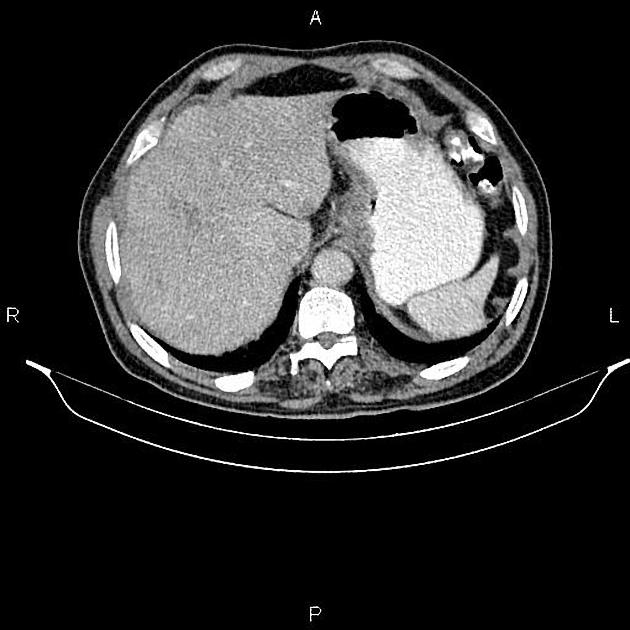
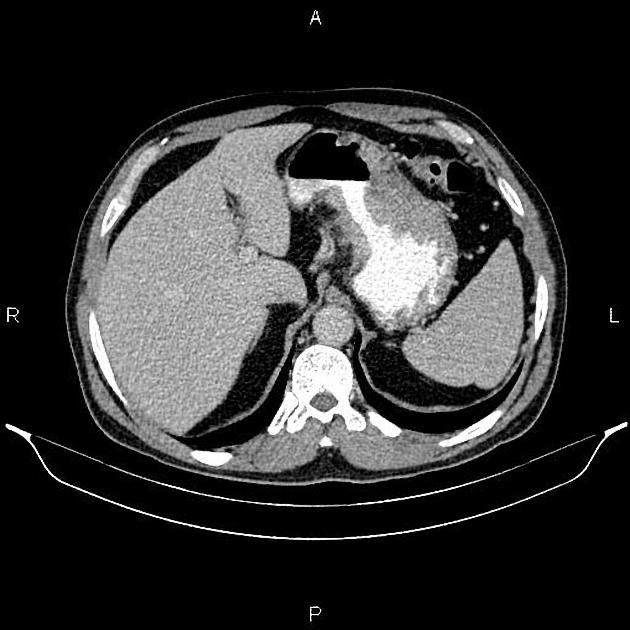
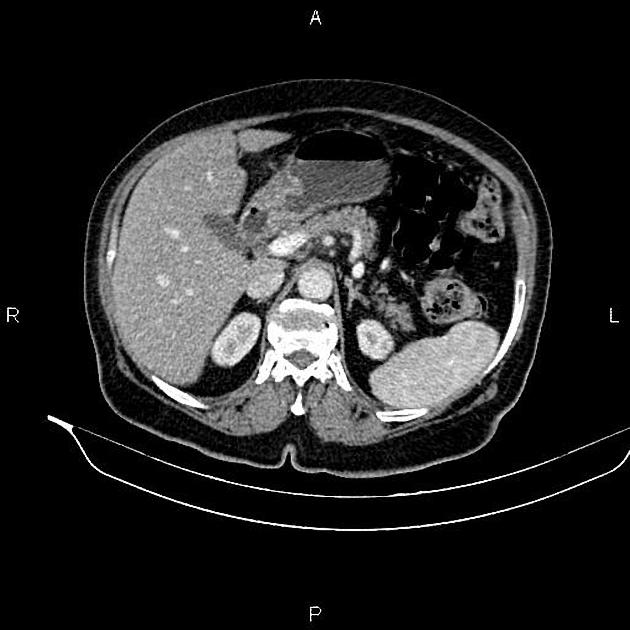
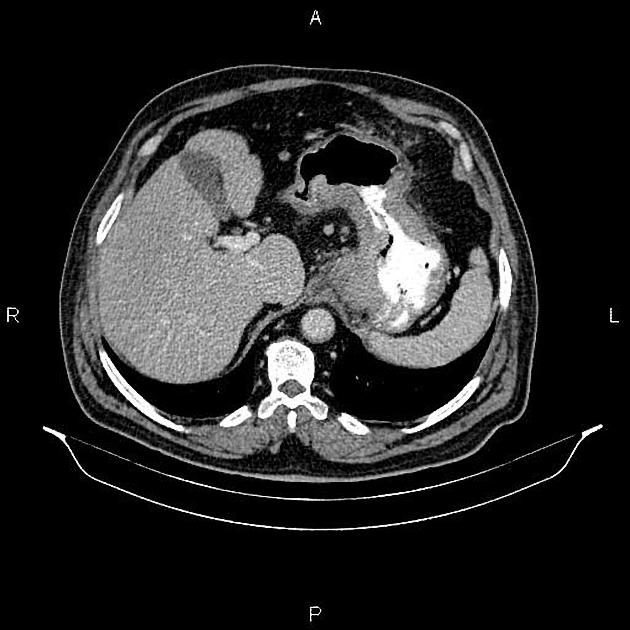
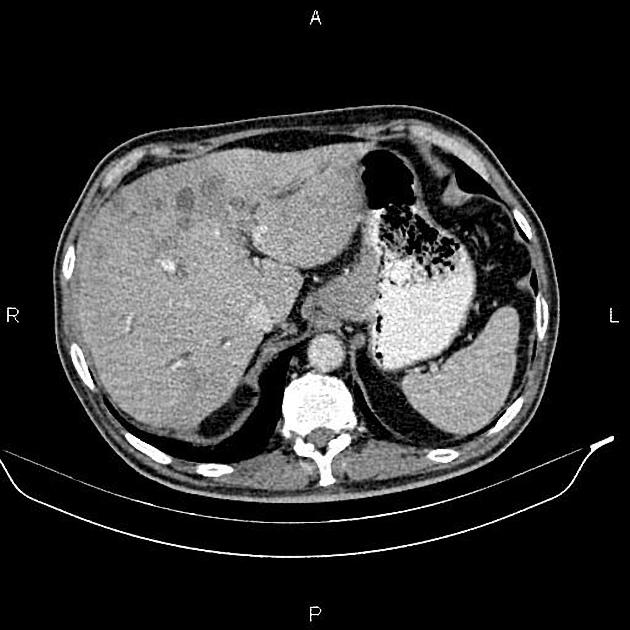
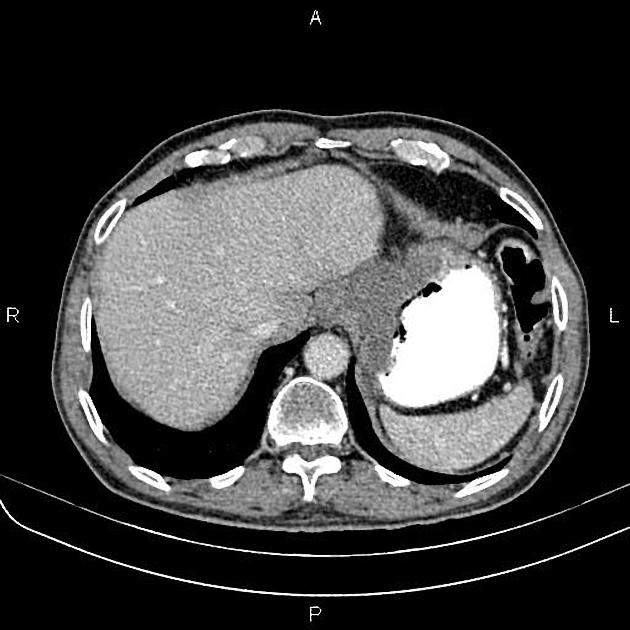
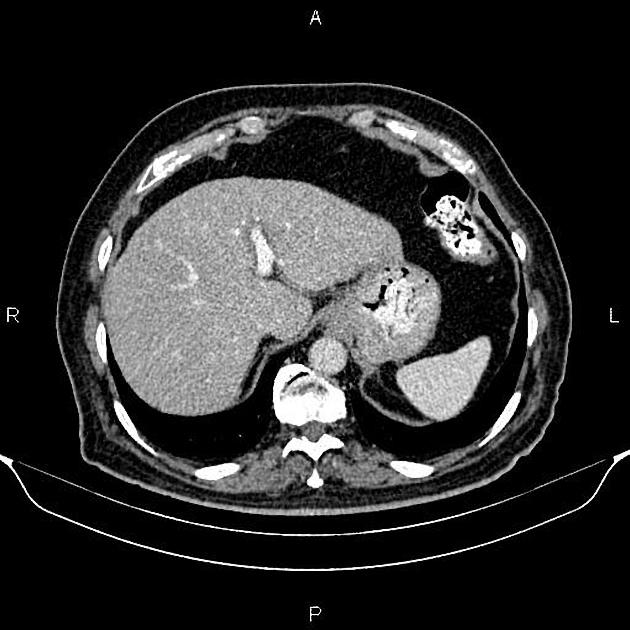
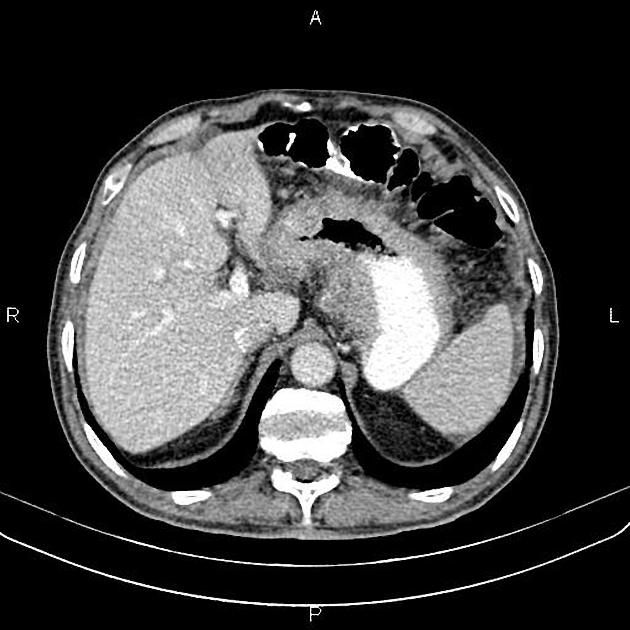
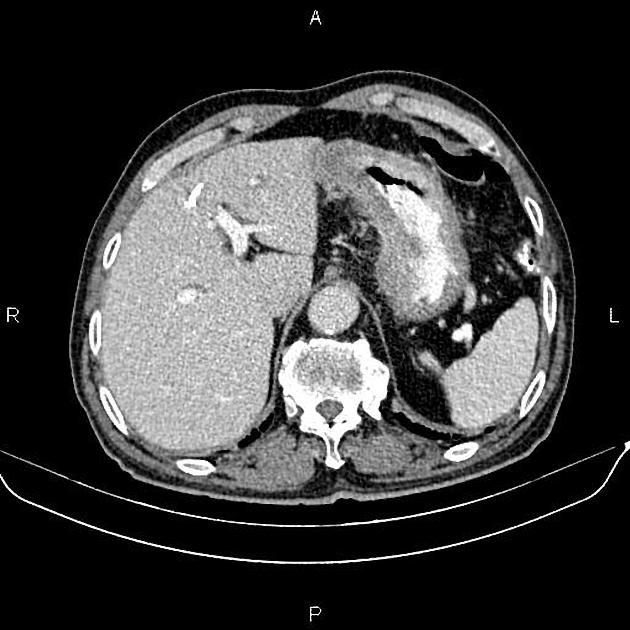
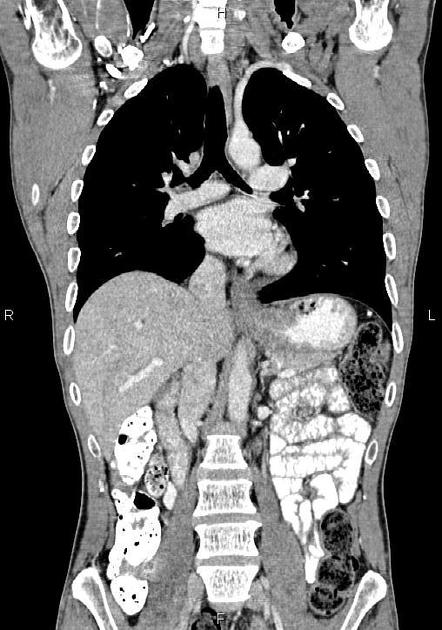
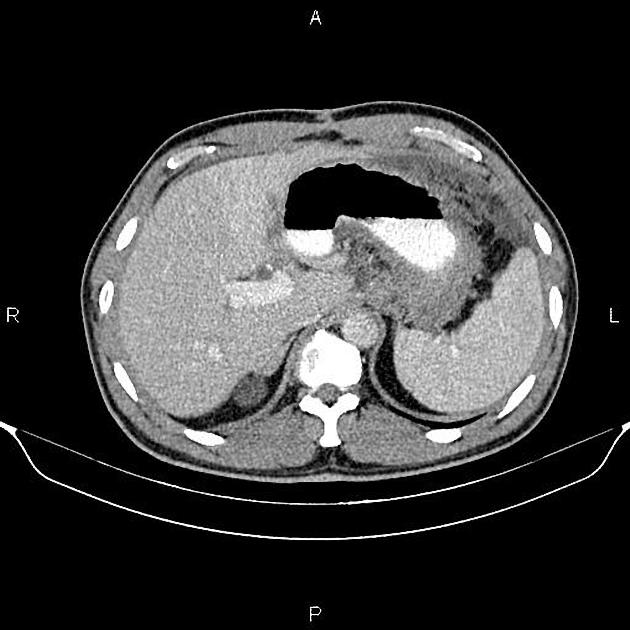
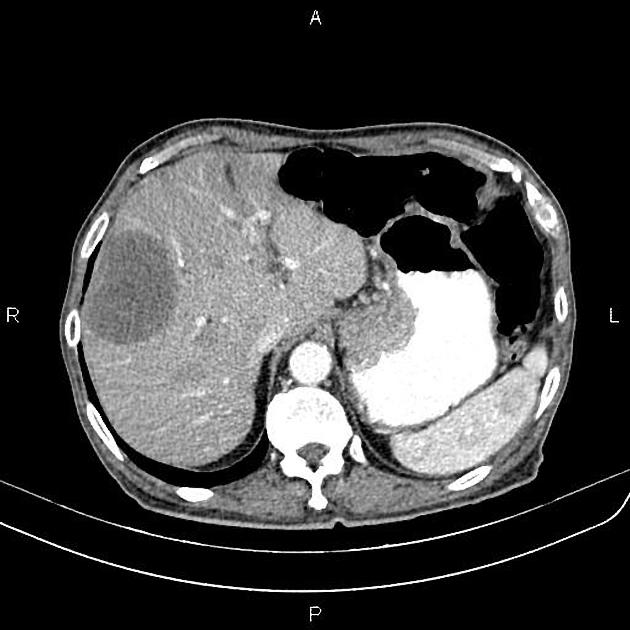
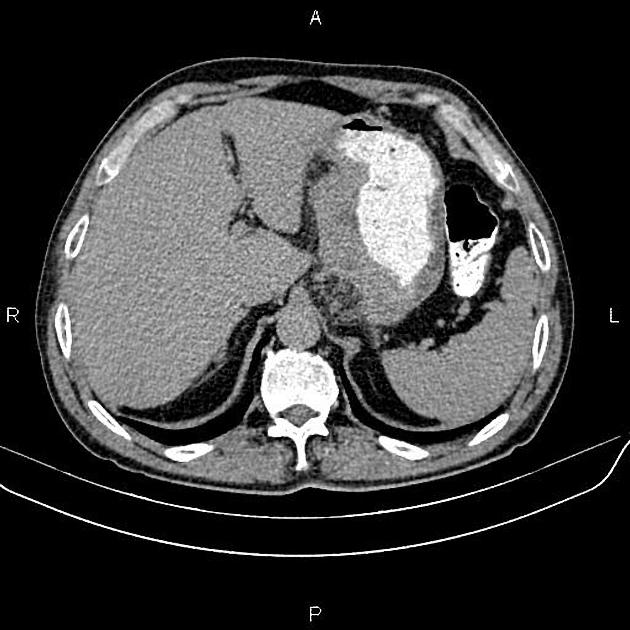
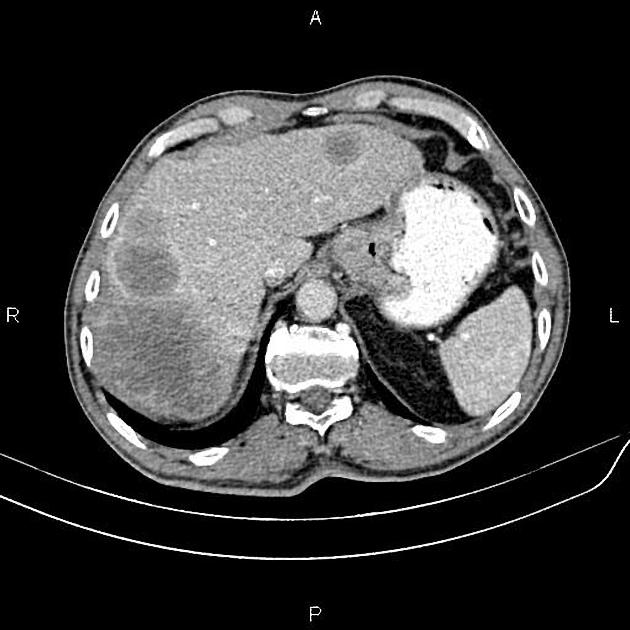
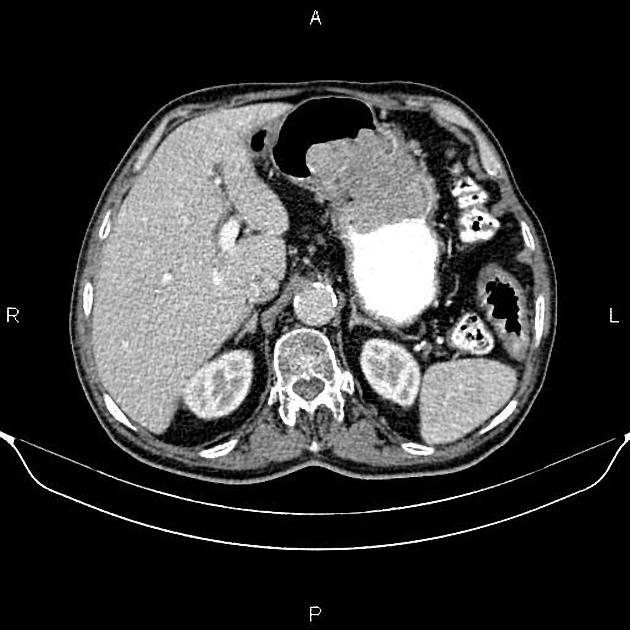
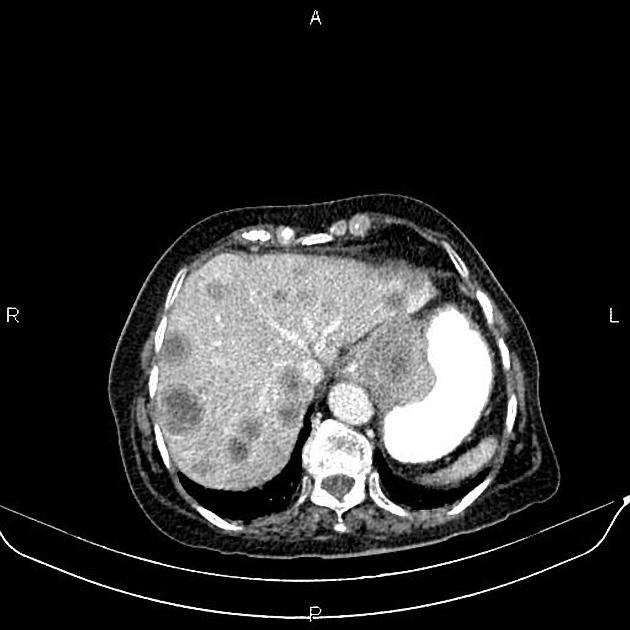
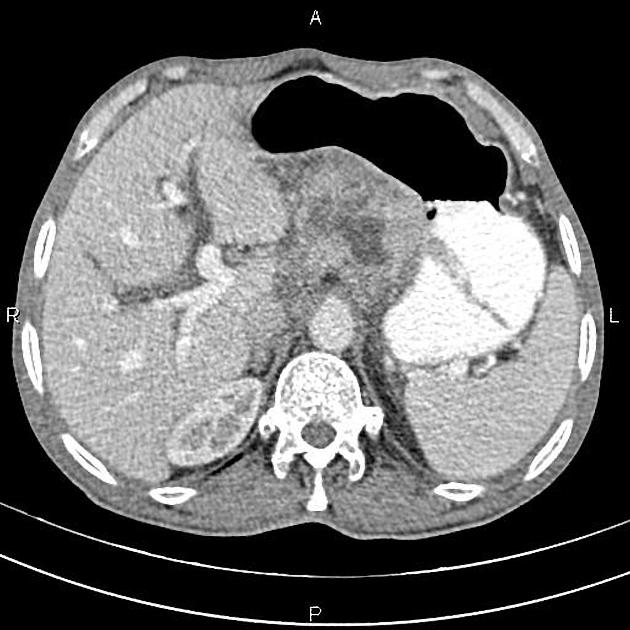
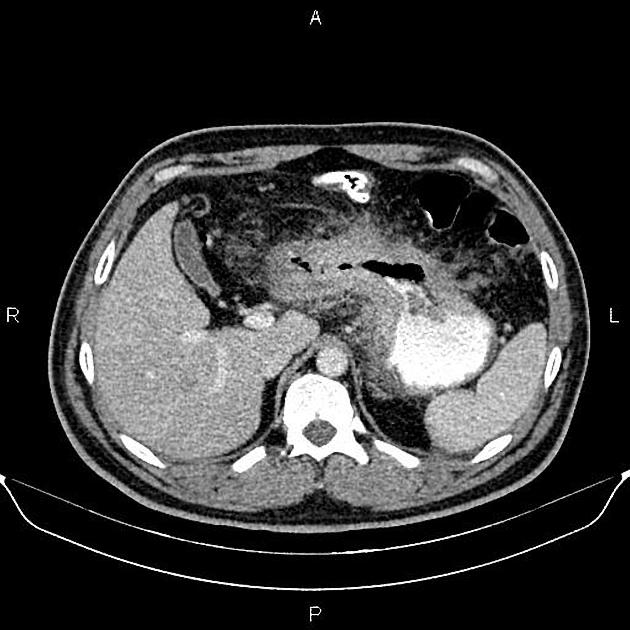
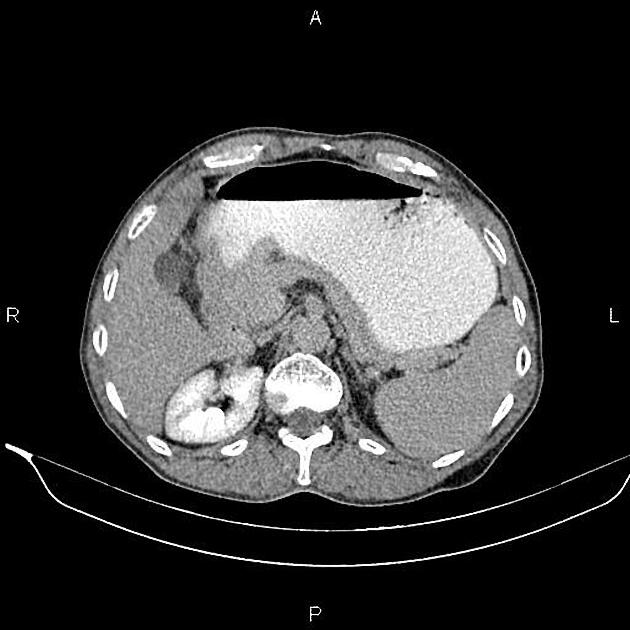
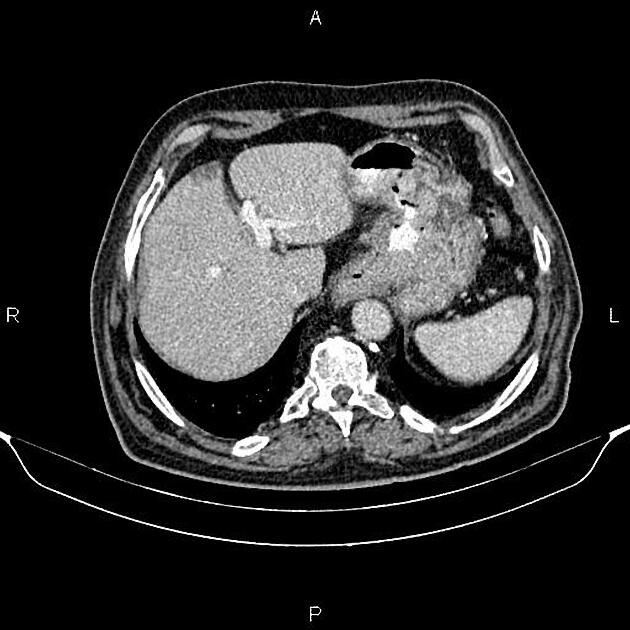
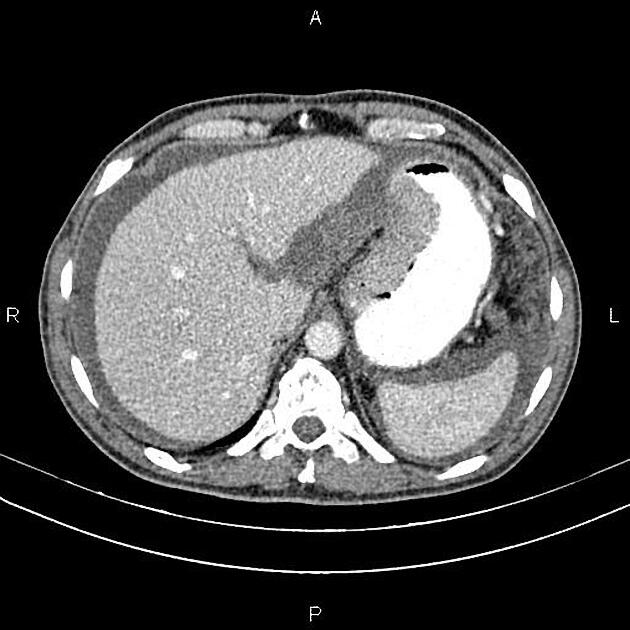
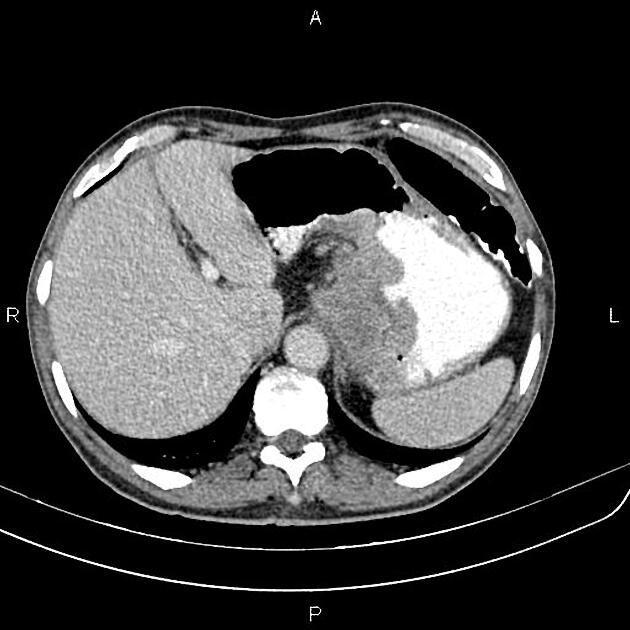
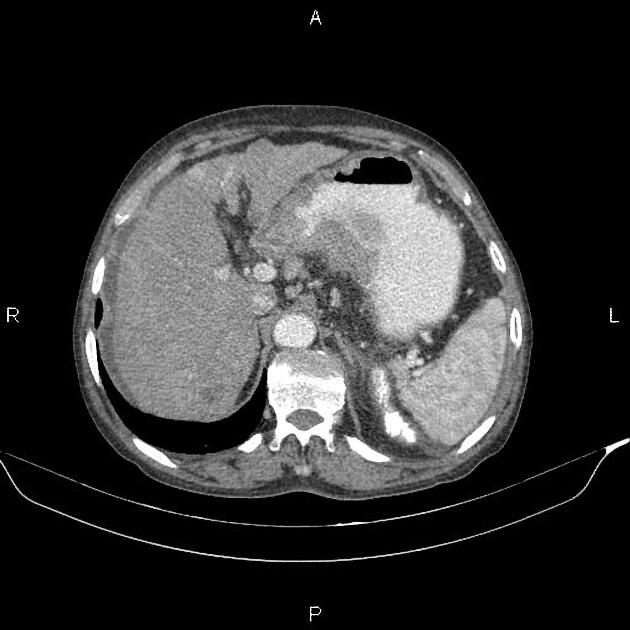
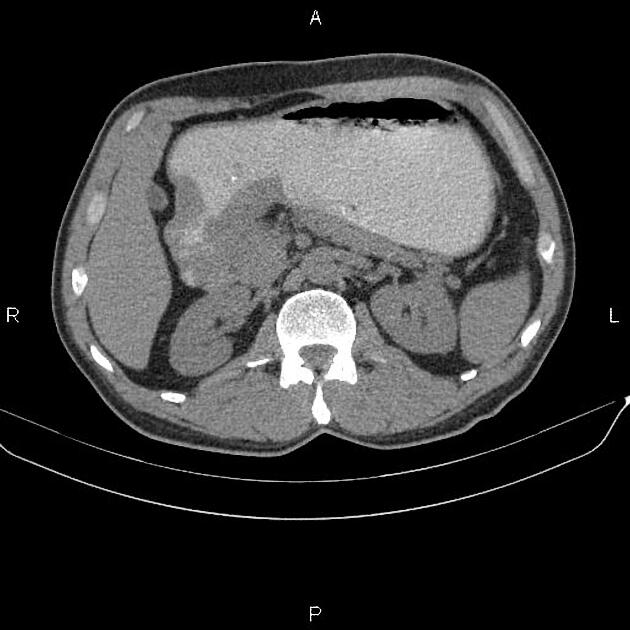
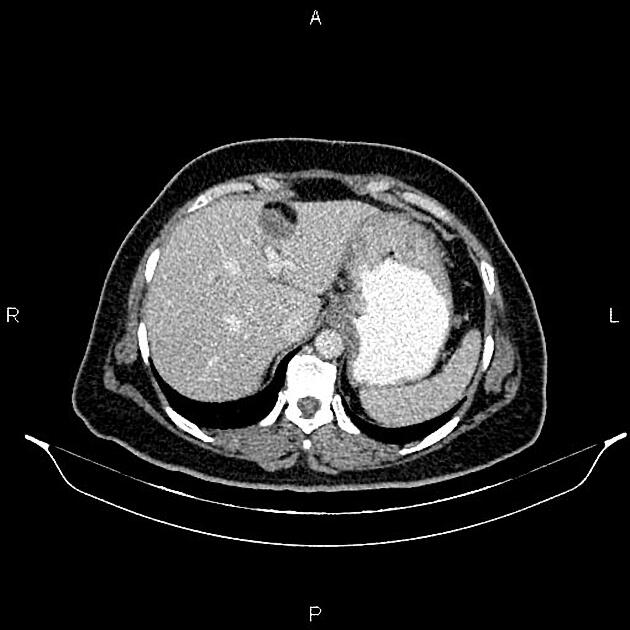
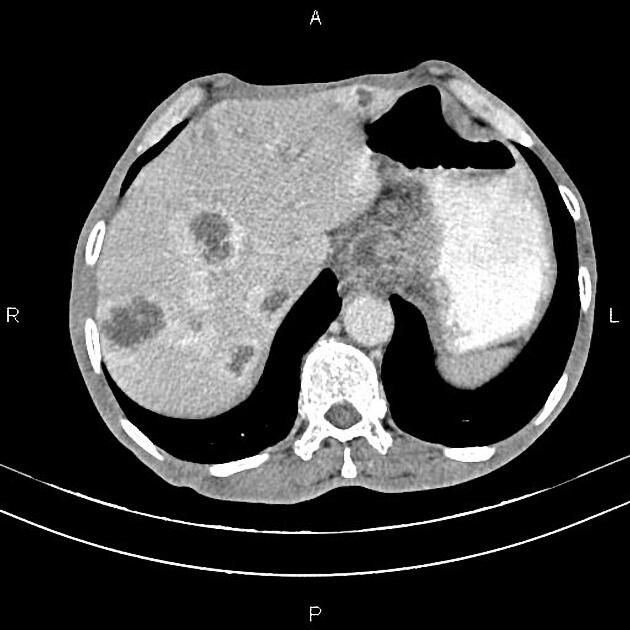
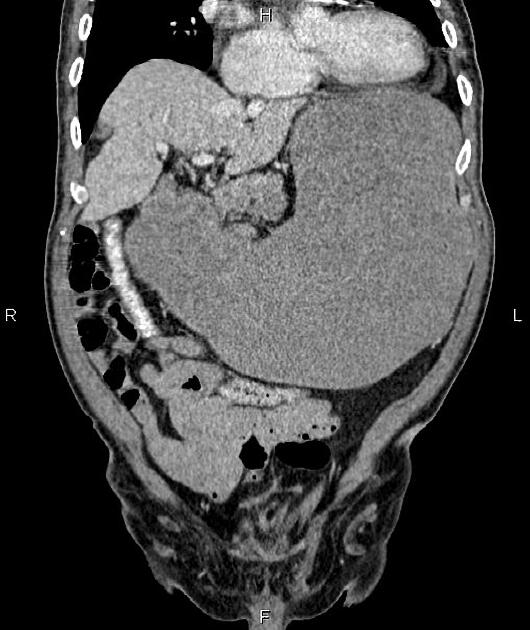
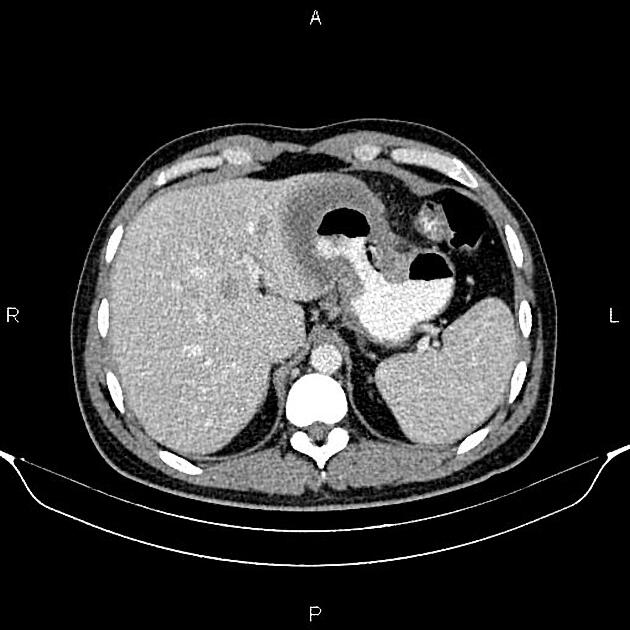
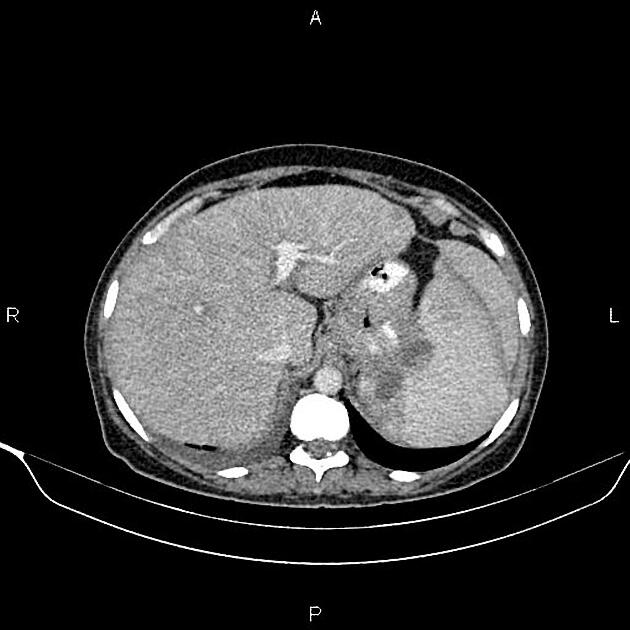
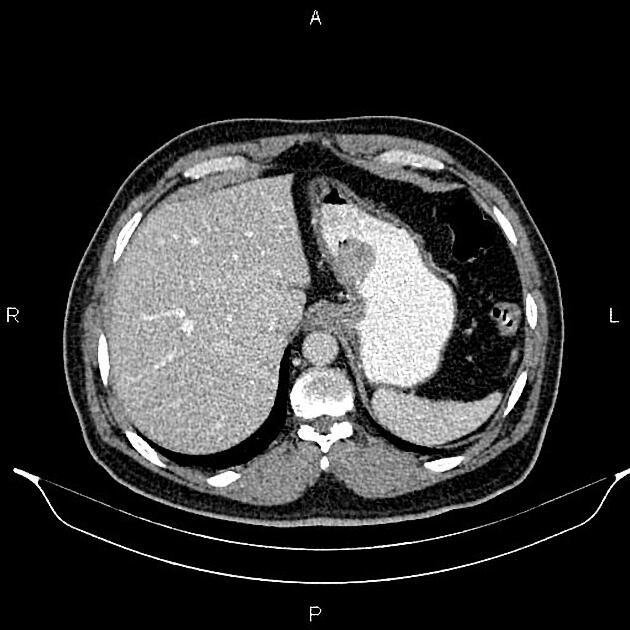
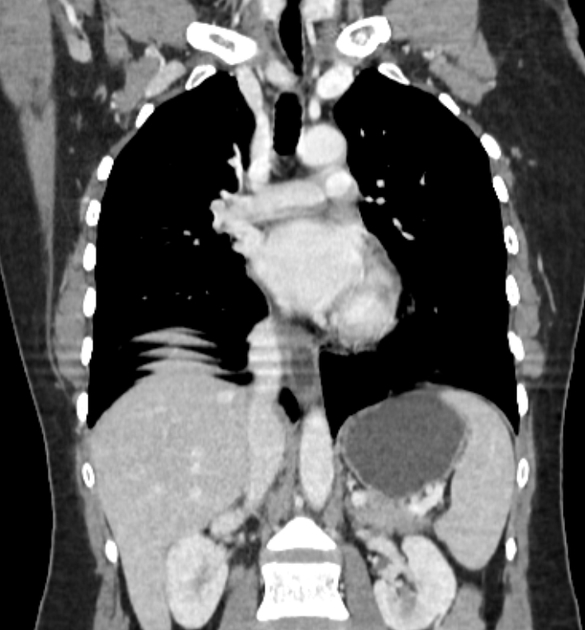
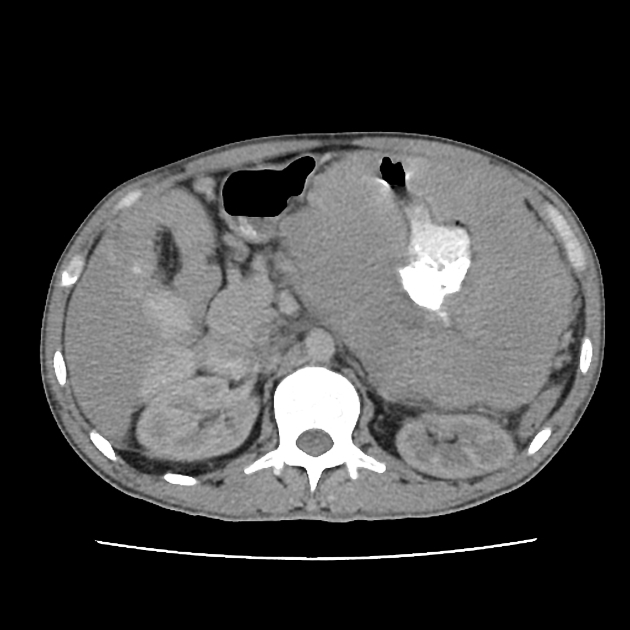
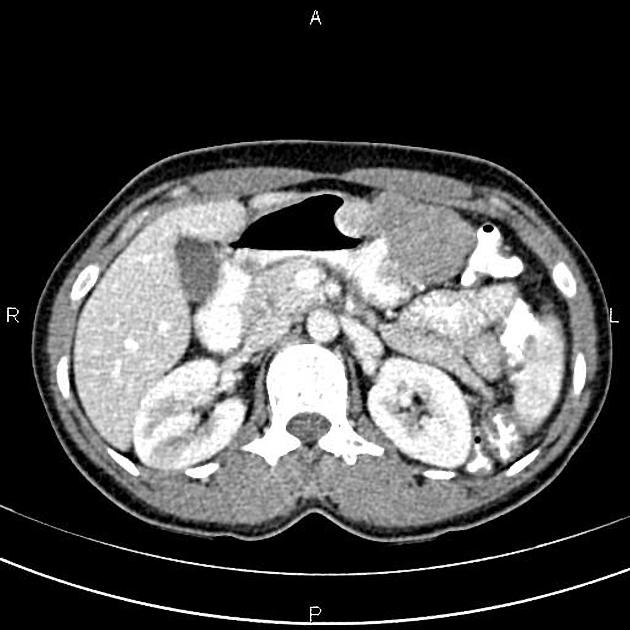
CT
CT is the staging modality of choice because it can help identify the primary tumour, assess for the local spread, and detect nodal involvement and distant metastases 1.
Demonstration of lesions facilitated by negative contrast agents (water or gas):
a polypoid mass with or without ulceration
focal wall thickening with mucosal irregularity or focal infiltration of the wall
ulceration: gas-filled ulcer crater within the mass
infiltrating carcinoma: wall thickening and loss of normal rugal fold pattern 4
Calcifications are rare but when present, they are usually mucinous adenocarcinoma.
Treatment and prognosis
It is an aggressive tumour with a 5-year survival rate of less than 20%. Prognosis is correlated to the stage of the tumour at presentation. Therefore, accurate staging of gastric cancer is essential because surgical resection is the treatment for localised disease 1.
Peritoneal metastases (gastric carcinomatosis) can occur especially in advanced stage gastric cancer and is frequently considered to be an incurable disease 12-13.
Complications
perforation with peritonitis: rare (thought to occur in ~2% of cases) 5,6
Differential diagnosis
The imaging differential can be broad and includes:
gastric stromal tumour (GIST)
gastric neuroendocrine tumour (GNET) type 3, which is the sporadic and more aggressive form
benign gastric (peptic) ulcer
secondary changes from pancreatitis (from extrinsic inflammatory change)


























 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.