Hydrosalpinx is a descriptive term and refers to a fluid-filled dilatation of the fallopian tube. If the fluid is infected, i.e. pus, then it is a pyosalpinx; if bloody, then haematosalpinx.
On this page:
Clinical presentation
Patients may be asymptomatic or may present with pelvic pain or infertility.
Pathology
One or both fallopian tubes may be affected. A hydrosalpinx results from an accumulation of secretions when the tube is occluded at its distal end (obstruction of the ampullary segment) or both ends. On rare occasions, transient distention of the fallopian tubes occurs because of retrograde passage of blood from the uterus without complete distal occlusion.
Aetiology
endometriosis (often haematosalpinx)
pelvic inflammatory disease (e.g chlamydial or gonococcal infection): a hydrosalpinx is most commonly a sequela of adhesions from pelvic inflammatory disease
-
post-hysterectomy (without salpingo-oophorectomy)
unilateral or bilateral hydrosalpinx may also occur in women after a hysterectomy when only the fallopian tubes are left to protect the blood supply to the ovary
this is from the accumulation of tubal secretions caused by surgical blockage proximally and adhesion-related blockage distally
tubal malignancy: primary or secondary tumours of the fallopian tubes
Radiographic features
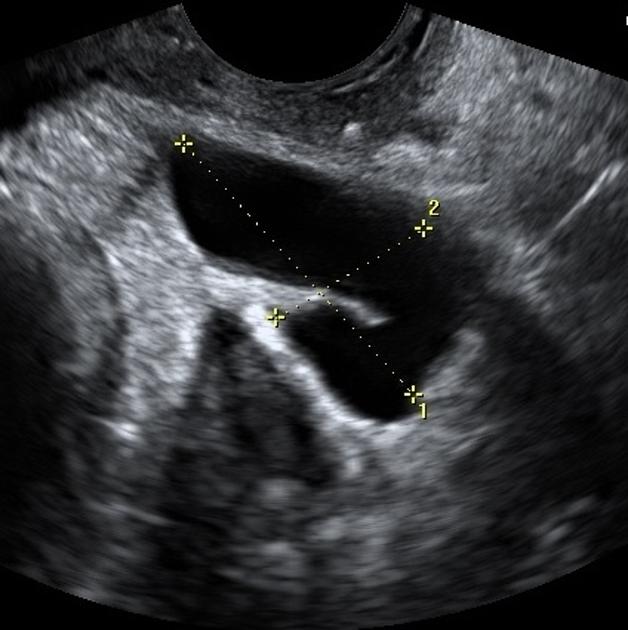
Ultrasound
thin- or thick-walled (in chronic cases)
elongated or folded, tubular, C-shaped, or S-shaped fluid-filled structure
distinct from the uterus and ovary.
Longitudinal folds in a normal fallopian tube may become thickened in the presence of a hydrosalpinx. The folds may produce a characteristic “cogwheel” appearance when imaged in cross-section. These folds are pathognomonic of a hydrosalpinx. Indentations on the opposite sides of the wall are referred to as the waist sign, which strongly predicts hydrosalpinx. The waist sign, in combination with a tubular-shaped cystic mass, has been found to be pathognomonic of a hydrosalpinx 9. Incomplete septa may also give a "beads on a string" sign.
Sometimes, the dilated fallopian tube may not show longitudinal folds. If the elongated nature of these folds is not noted, they may be mistaken for mural nodules of an ovarian cystic mass. A significantly scarred hydrosalpinx may present as a multilocular cystic mass with multiple septa (often incomplete) creating multiple compartments. These septa are generally incomplete, and the compartments can be connected. However, with more pronounced scarring, differentiation from an ovarian mass may not be possible.
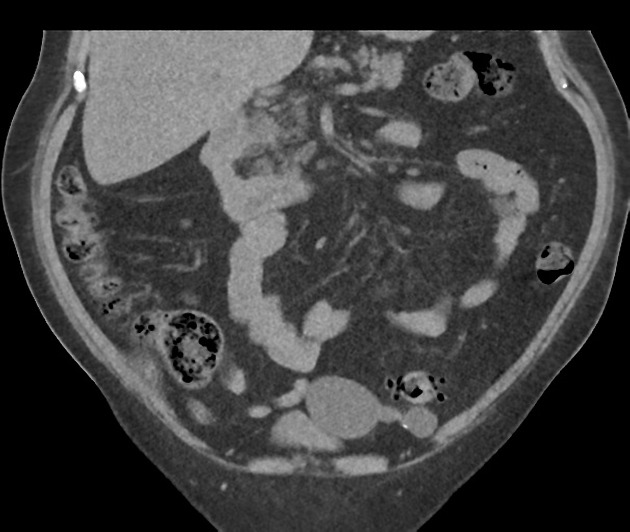
CT
A hydrosalpinx may be seen incidentally at CT as a fluid-attenuation tubular adnexal structure, separate from the ovary. A simple hydrosalpinx is not accompanied by pelvic inflammation. The tubal wall may enhance following contrast.
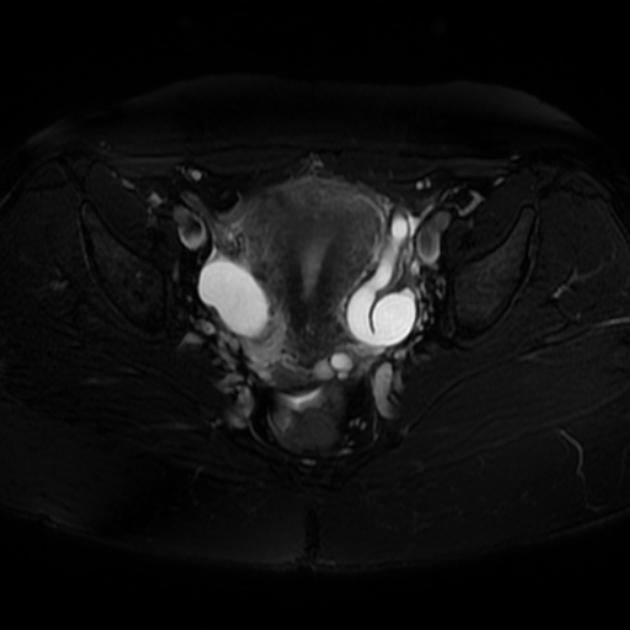
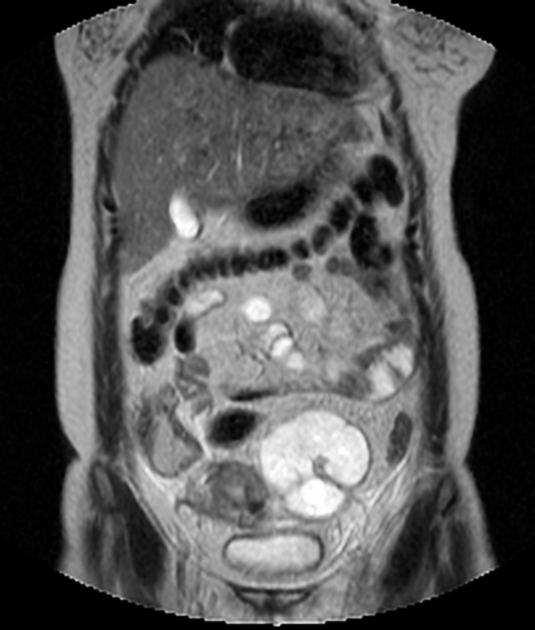
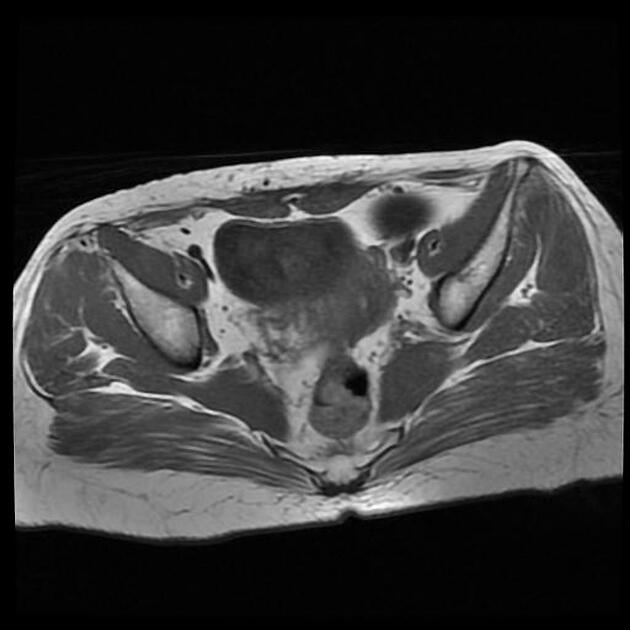
MRI
MR imaging is the modality of choice for the characterisation and localisation of adnexal masses that are inadequately evaluated with ultrasound. A dilated fallopian tube is interposed between the uterus and ovary and demonstrates fluid signal intensity. Incomplete septa or folds can be seen. The mucosal plicae are usually effaced, and the tube wall is uniformly smooth and thin.
Signal characteristics of the dilated tube(s) include:
T1: typically hypointense although can be hyperintense if there is proteinaceous fluid
T2: hyperintense
T1 C+ (Gd): the mucosal plicae and the tube walls may show mild enhancement
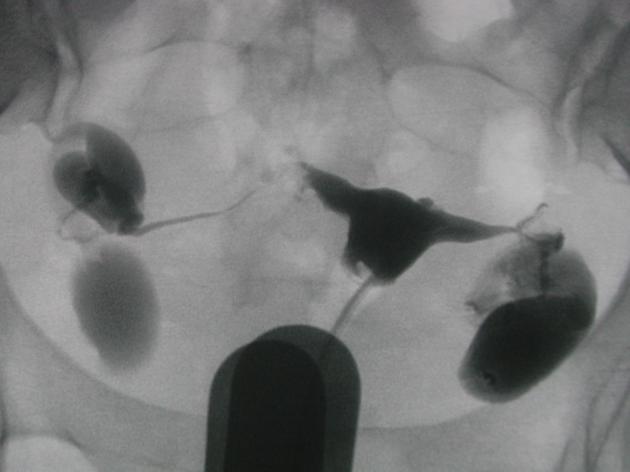
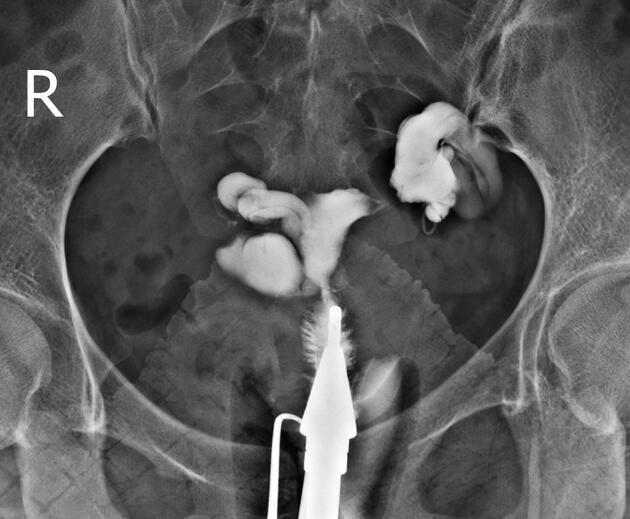
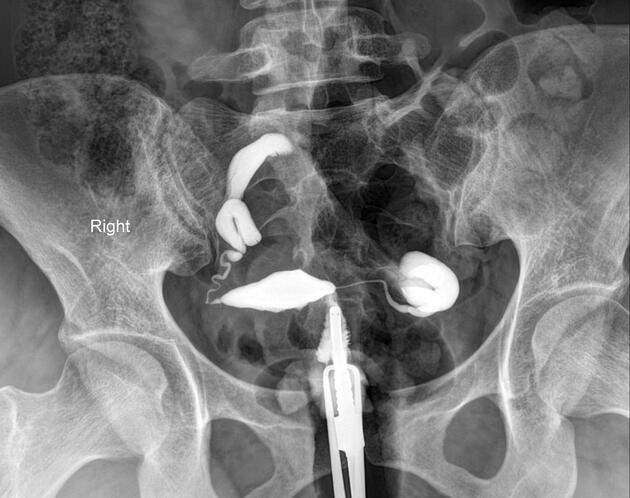
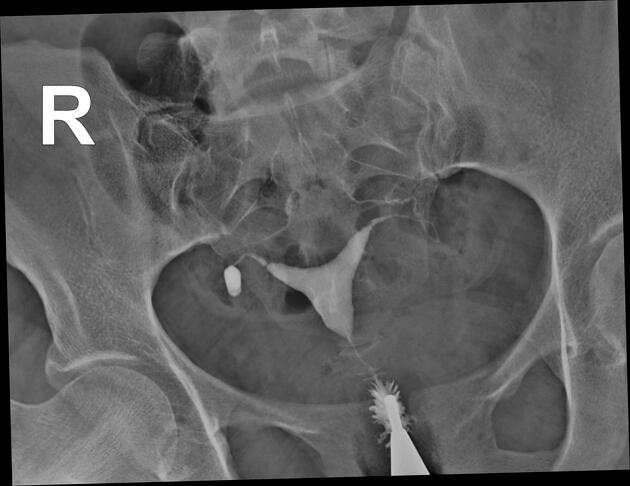
Hysterosalpingogram
Will classically show a dilated fallopian tube, filling with contrast and with absence of free spillage.
Treatment and prognosis
Complications
tubal torsion: can be a late complication 4,7
Differential diagnosis
General imaging differential considerations include
elongated paraovarian cyst
cystic ovarian neoplasm(s): identification of a separate ovary helps distinguish a hydrosalpinx from a cystic ovarian mass, an important distinction because malignancy is rare with an extraovarian cystic adnexal mass
bowel obstruction: at the pelvic level with dilated bowel loops: a dilated tube can be distinguished from pelvic bowel loops from the lack of peristalsis
dilated pelvic veins: pelvic veins can be recognised from the presence of moving low-level internal echoes, and blood flow may be detectable on Doppler interrogation
elongated pelvic perineural cyst






































 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.