Pituitary macroadenomas are the most common suprasellar mass in adults, and responsible for the majority of transsphenoidal hypophysectomies. They are defined as pituitary adenomas greater than 10 mm in size and are approximately twice as common as pituitary microadenomas.
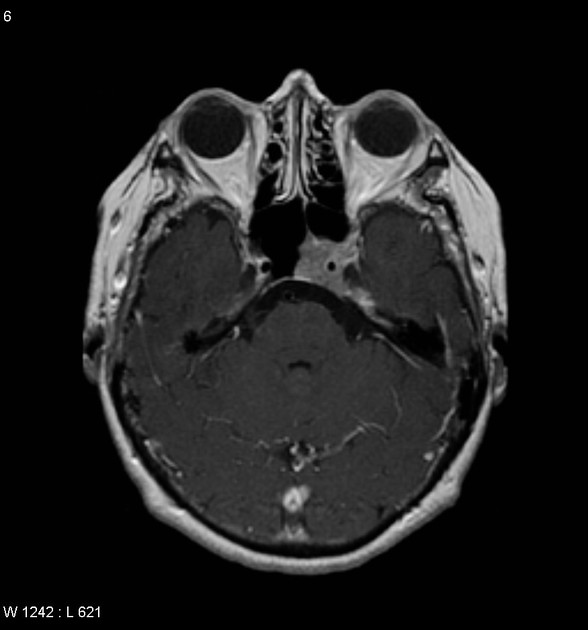
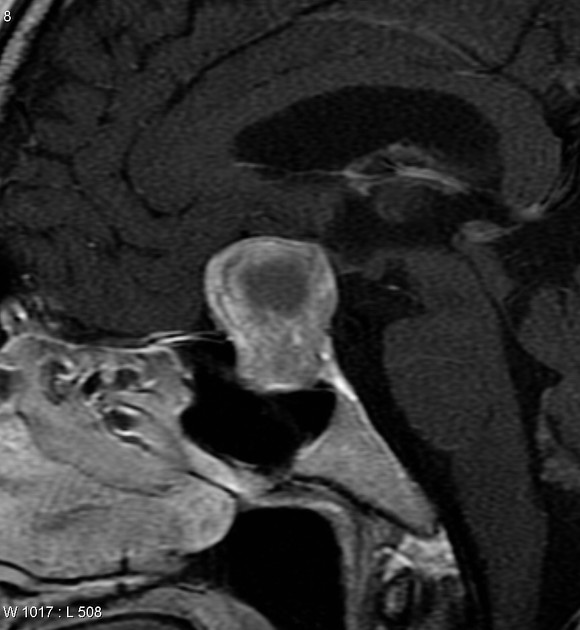
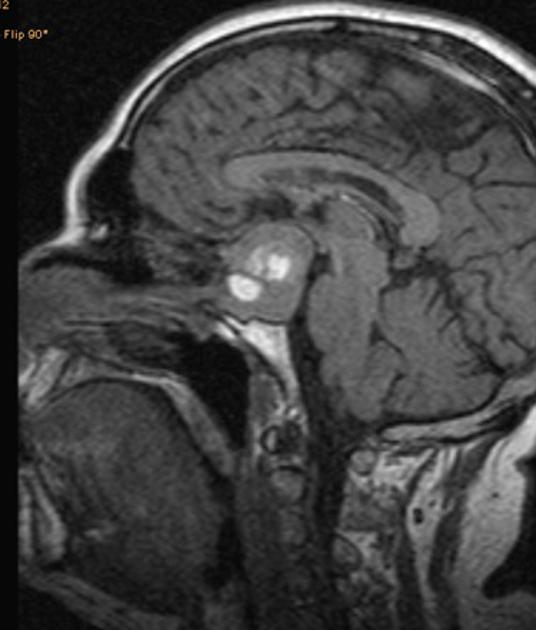
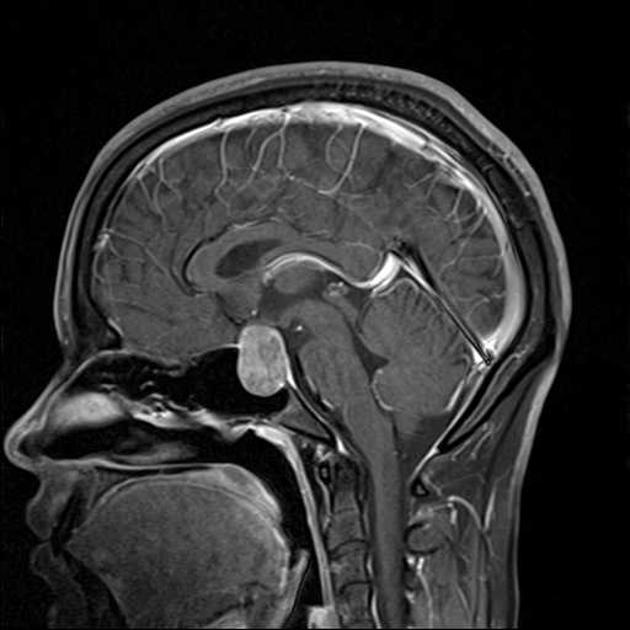
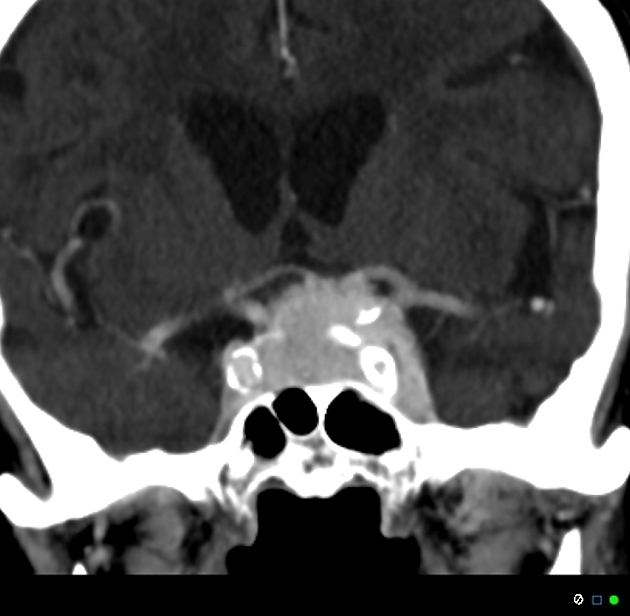
On imaging, they usually present as a solid tumor with CT attenuation values similar to the brain (30-40 HU) and demonstrate moderate contrast enhancement. The same is observed on MRI, where they are isointense to the grey matter both on T1- and T2-weighted images. However, attenuation and signal characteristics can significantly vary depending on tumor components such as hemorrhage, cystic transformation, or necrosis.
For a general discussion, including epidemiology, treatment, and prognosis, please refer to the article on pituitary adenomas.
On this page:
Clinical presentation
Patients typically present with symptoms of local mass effect on adjacent structures (especially optic chiasm). Some may present due to hormonal imbalance, with symptoms of hypopituitarism (from compression) or secretion. Hormonal imbalance due to overproduction tends to present earlier and tumors are thus usually small at presentation. This mode of presentation is discussed in the article on pituitary microadenomas.
Rarely pituitary apoplexy may present acutely and often catastrophically.
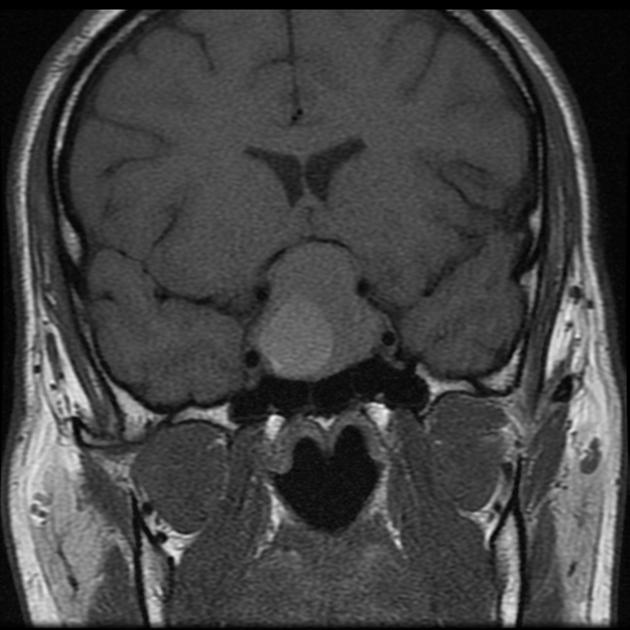
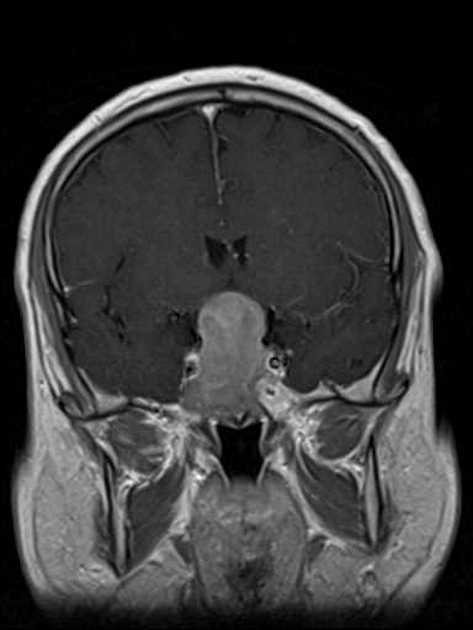
Optic chiasm compression
The optic chiasm is located directly over the pituitary gland in 80% of individuals. The rest is divided between pre and postfixed chiasms. A prefixed optic chiasm is located anterior to its normal position over the tuberculum sellae, whereas a postfixed chiasm is located over the dorsum sellae 10.
A macroadenoma growing superiorly out of the pituitary fossa (or for that matter other pituitary region masses) will contact, elevate and compress the central part of the chiasm in most individuals. This central part carries fibers from the nasal retina, and thus results in the classical bitemporal hemianopia 10. Patients typically complain of bumping into things or having car accidents, but as the macular fibers are often spared, they may not be aware of their visual deficits.
In cases of prefixed or postfixed chiasms, or when the macroadenoma grows asymmetrically, then the optic nerves or optic tracts can be compressed, resulting in a variety of visual deficits.
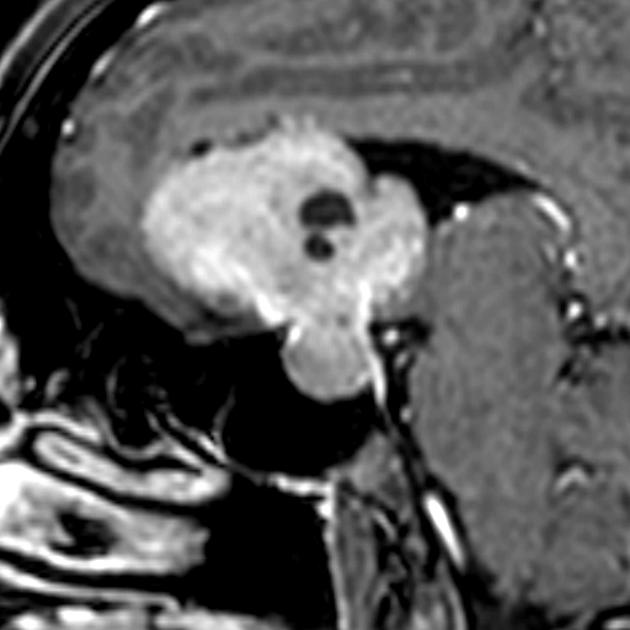
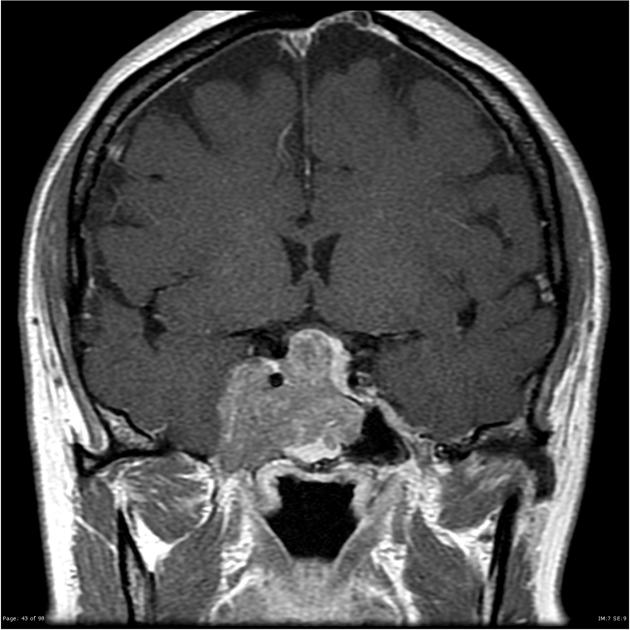
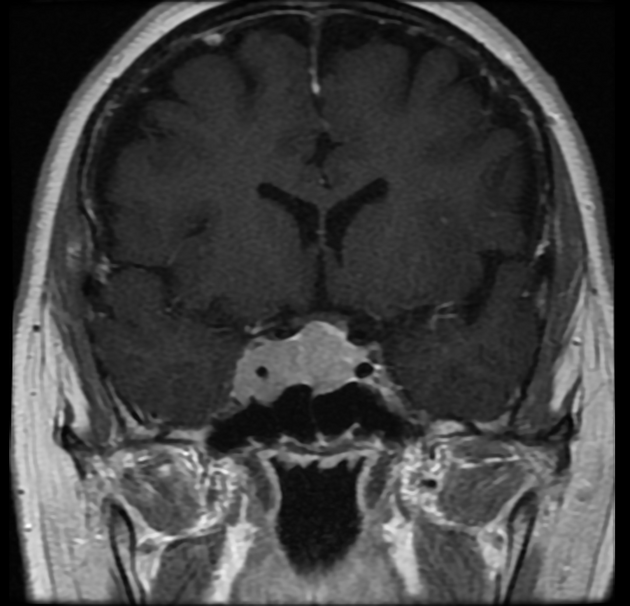
Cavernous sinus invasion
Some macroadenomas demonstrate invasive growth, and extension into the cavernous sinuses is characteristic. Prolactin-secreting tumors are most frequently responsible for cavernous sinus extension, and typically prolactin levels increase significantly when the tumor gains access to the sinus 10. Once in the sinus, these tumors are difficult to resect completely.
They may compress cranial nerves resulting in deficits, although this is uncommon, seen in only 1-14% of cases 10. The oculomotor nerve (CN III) is most commonly involved, followed by the abducens nerve (CN VI) 10.
The likelihood of surgical/histological invasion can be estimated with the Knosp classification.
Pathology
Most macroadenomas are non-secretory (endocrinologically inactive). They are a type of benign epithelial tumor composed of adenohypophyseal cells.
Radiographic features
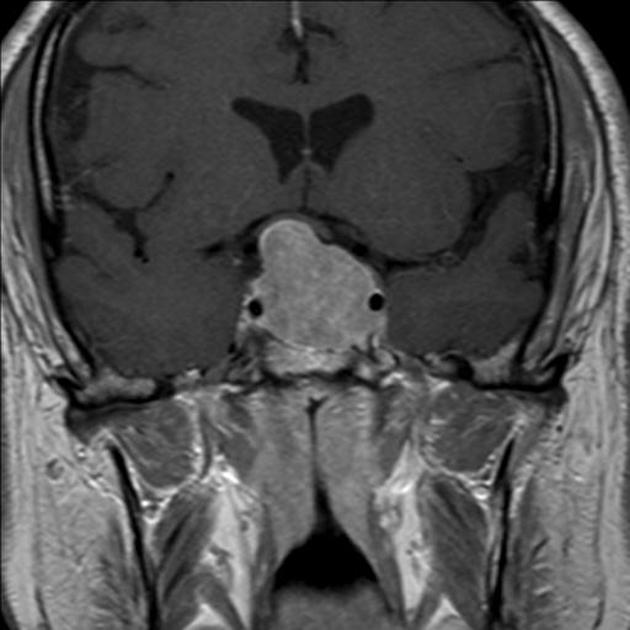
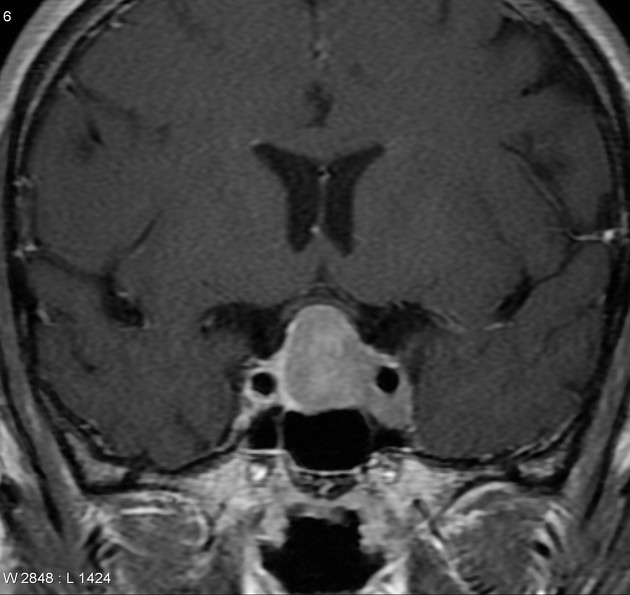
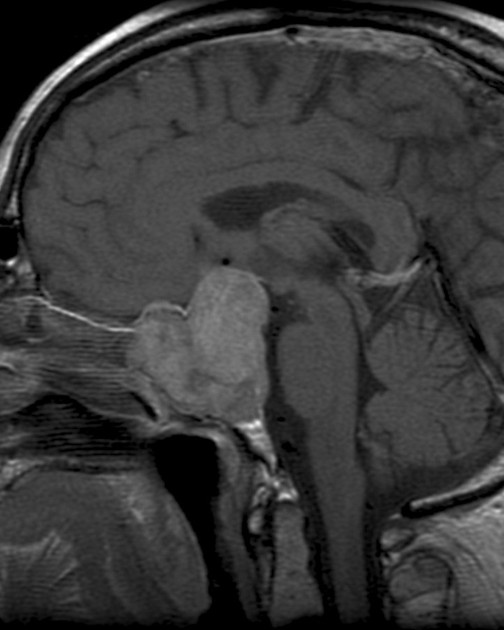
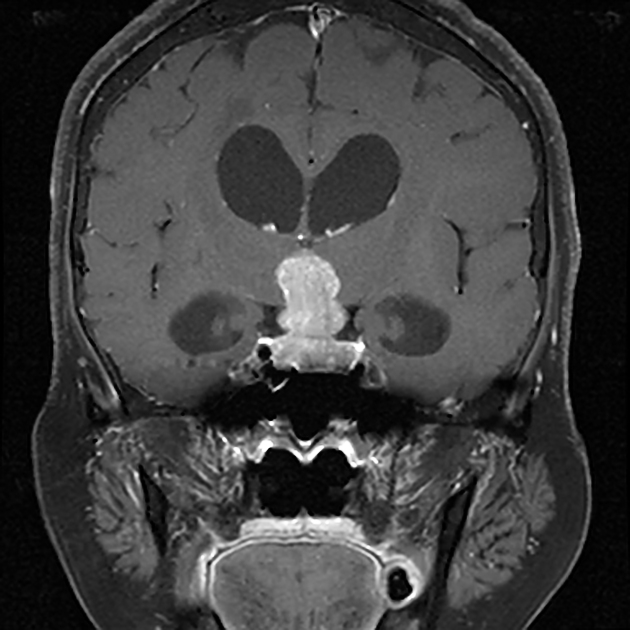
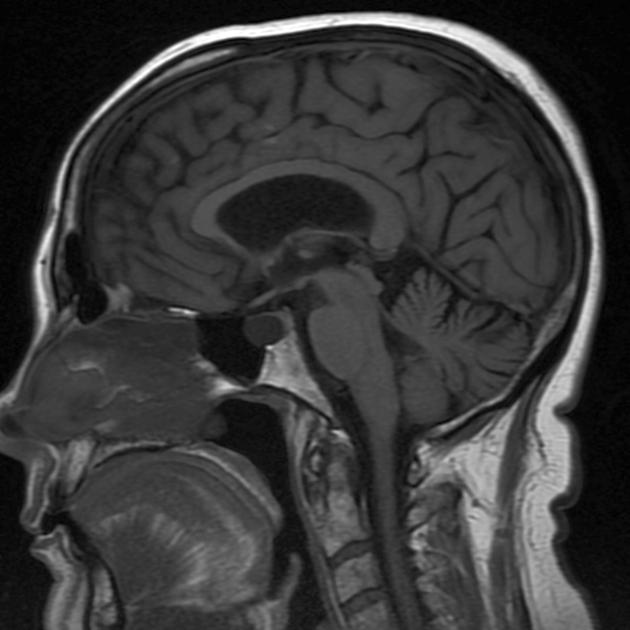
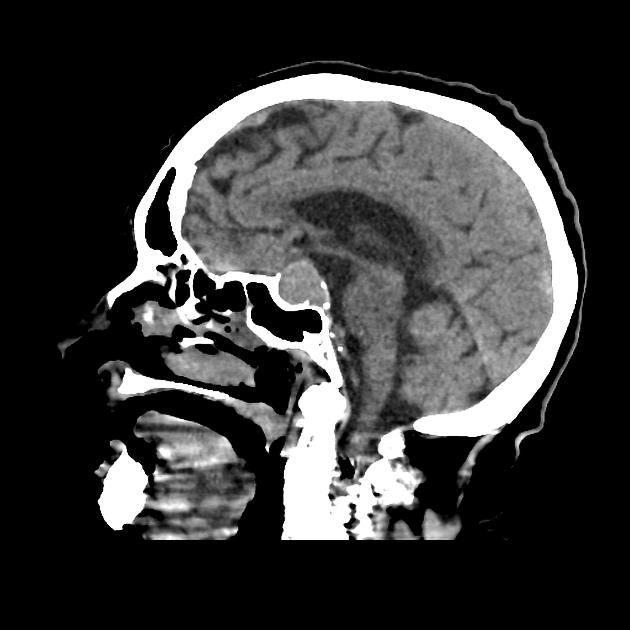
Pituitary macroadenomas are by definition >10 mm diameter masses arising from the pituitary gland, and usually extending superiorly into the suprasellar cistern where it can compress the chiasm. Bilateral indentation by the diaphragma sellae as the tumor passes superiorly can give a snowman or figure-eight configuration 10.
Because these tumors are typically slow-growing, the pituitary fossa is almost invariably enlarged with thinned remodeled bone.
CT
Non-contrast attenuation can vary depending on hemorrhagic, cystic, and necrotic components. Solid adenomas without hemorrhage, typically have attenuation similar to the brain (30-40 HU) and demonstrate moderate contrast enhancement; less marked than one typically sees in meningiomas. Calcification is rare.
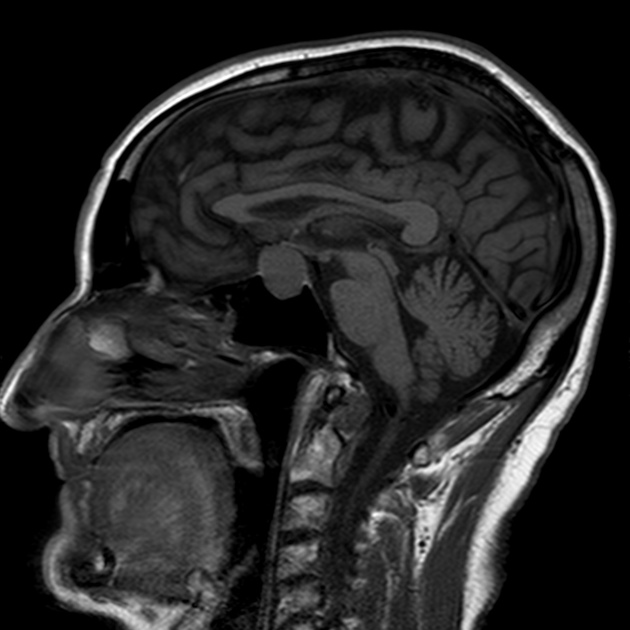
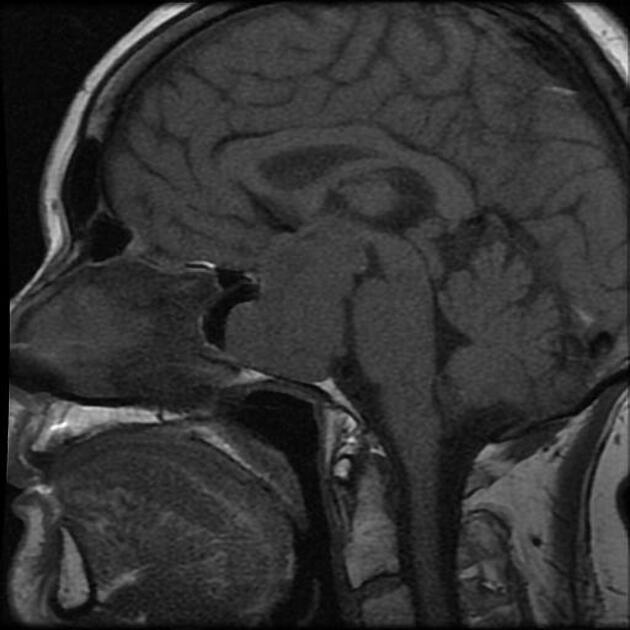
MRI
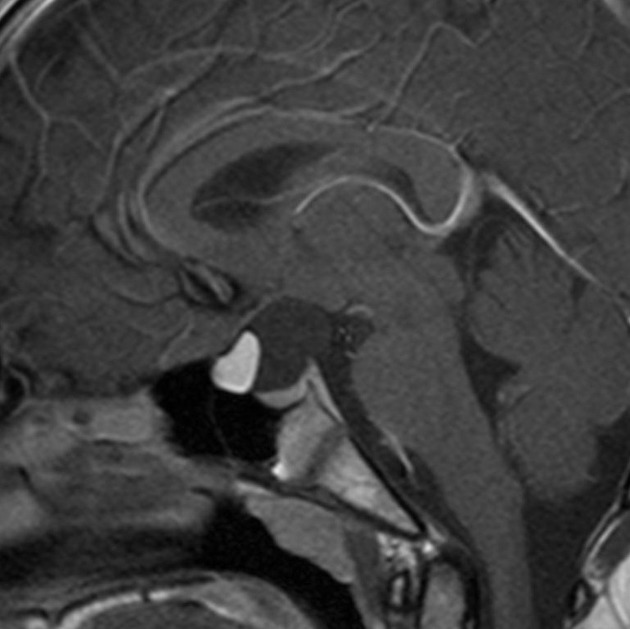
MRI is the preferred imaging modality. It is able to delineate the mass exquisitely as well as clearly visualize the optic chiasm, anterior cerebral vessels, and cavernous sinuses.
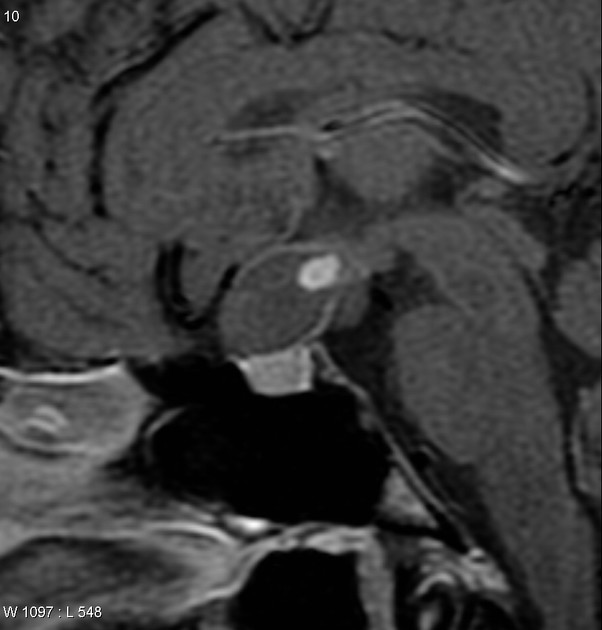
Overall signal characteristics can significantly vary depending on tumor components such as hemorrhage, cystic transformation, or necrosis. In such cases, a fluid-fluid level may be seen that is a helpful feature in strongly favoring a cystic pituitary adenoma over a Rathke cleft cyst 14.
Signal characteristics
-
T1
typically isointense to grey matter 10
larger lesions are often heterogeneous and vary in signal due to areas of cystic change/necrosis/hemorrhage
-
T1 C+ (Gd)
solid components demonstrate moderate to bright enhancement
-
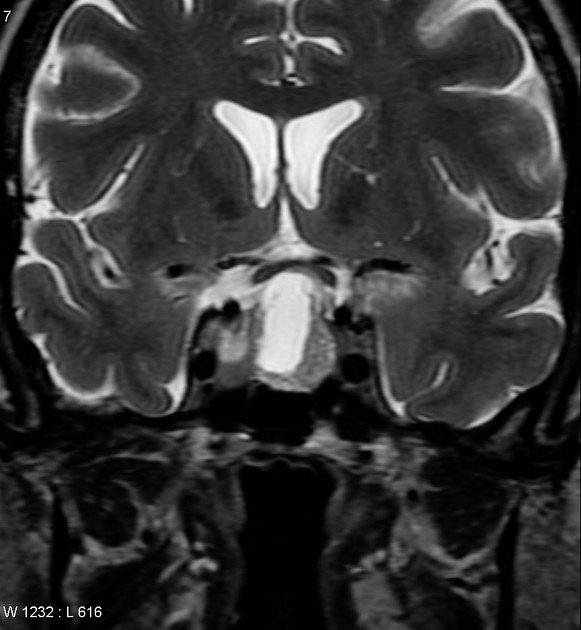
T2
typically isointense to grey matter 10
larger lesions are often heterogeneous and vary in signal due to areas of cystic change/necrosis/hemorrhage
a hypointense rim is often present (75%) 14
-
GRE/SWI
most sensitive for detecting any hemorrhagic components, which appear as areas of signal loss
calcification is rare but should be excluded by reviewing CT scans
Cavernous sinus invasion
Attempting to predict invasion based on imaging is important preoperatively. Generally, the more laterally a tumor extends into the cavernous sinus, and the more it encircles the internal carotid artery, the greater the likelihood of invasion.
The most convenient method is to assess the degree of encasement of the cavernous portion of the internal carotid artery. Less than 90 degrees makes involvement of the sinus very unlikely, whereas >270 degrees makes involvement almost certain 10.
Alternatively, an MRI grading system described by Knosp et al. based on tumor extension past tangents drawn along the medial, central, and lateral aspects of the supra- and intracavernous internal carotid arteries is easy to use and is predictive of surgical and histological invasion (see Knosp classification system) 11,13.
Nuclear medicine
PET-CT
The normal pituitary gland should not demonstrate significant FDG uptake and are normally not seen on PET-CT 12. Pituitary macroadenomas are highly hypermetabolic both with FDG and choline tracers.
Treatment and prognosis
Follow-up
For non-operated, non-functioning macroadenomas, follow-up should occur every 6-12 months based on proximity to the optic chiasm (less or more than 5 mm). If stable, annual follow-ups are recommended for the first three years, then continued thereafter 15.
Following complete surgical resection, some authors suggest biennial follow-ups for the first four years, then less frequently 15. For incomplete resections, follow-ups should be more frequent.
Differential diagnosis
The differential of a pituitary macroadenoma is essentially the list of conditions leading to a pituitary region mass. The most common considerations include:
-
often in the setting of known disseminated malignancy
often less well defined
bone destruction rather than remodeling may be seen
-
indistinguishable on imaging
CSF seeding may be evident
rare
-
separate pituitary is usually identifiable
dural tail usually visible
enhancement more vivid
hyperdense on non-contrast CT
-
craniopharyngioma (papillary type)
adamantinomatous craniopharyngiomas are more common in children
more likely to be cystic and to have areas of calcification (although still a minority of cases)
more likely to have areas of T1 intrinsic hyperintensity (although blood can result in similar appearances)
-
common in peripartum female
-
flow void common on MR
CTA can show flow
more likely to have calcification
-
Rathke cleft cyst (if cystic)
intracystic mural nodule is specific but not very sensitive 14
fluid-fluid levels are rare
more likely to be midline
less likely to have a dark T2 rim











 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.