Tuberculous spondylitis, also known as Pott disease, refers to vertebral body osteomyelitis and intervertebral discitis from tuberculosis (TB). The spine is the most frequent location of musculoskeletal tuberculosis, and commonly related symptoms are back pain and lower limb weakness/paraplegia.
On this page:
Epidemiology
Tuberculous spondylitis is one of the more common infections of the spine in countries where TB is prevalent. Due to the increase of multi drug-resistant mycobacteria, the incidence of TB and therefore tuberculous spondylitis is increasing.
Discitis and/or osteomyelitis comprise about 50% of manifestations of musculoskeletal tuberculosis, and usually affects the lower thoracic and upper lumbar levels of the spine 2.
Clinical presentation
Patients usually present with back pain, lower limb weakness/paraplegia, and kyphotic deformity. Constitutional symptoms (fever and weight loss) are also common but not as pronounced as with bacterial discitis/osteomyelitis due to the insidious nature of mycobacterial infection.
Pathology
The spine is involved due to hematogenous spread that can occur via both arteries and veins, resulting in different patterns of infection.
Anterior involvement
Spread through the anterior arterial arcade that richly supplies the subchondral paradiscal bone results in infection anteriorly in the bone immediately superior and inferior to the intervertebral disc 8.
In adults and particularly older individuals the disc is conspicuously spared due to its sparse vascularity. In contrast, in younger individuals, especially children, the disc may be involved early as it has a far richer blood supply 8.
Infection then spreads beneath the longitudinal ligaments and can lead to infection of adjacent vertebral bodies.
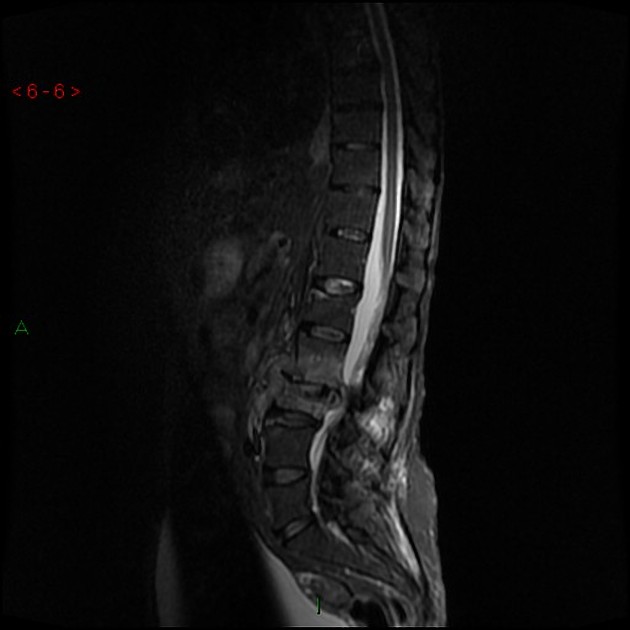
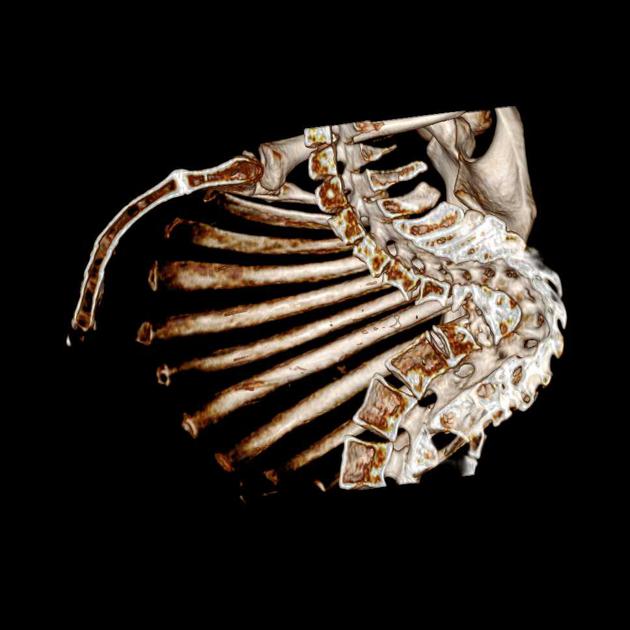
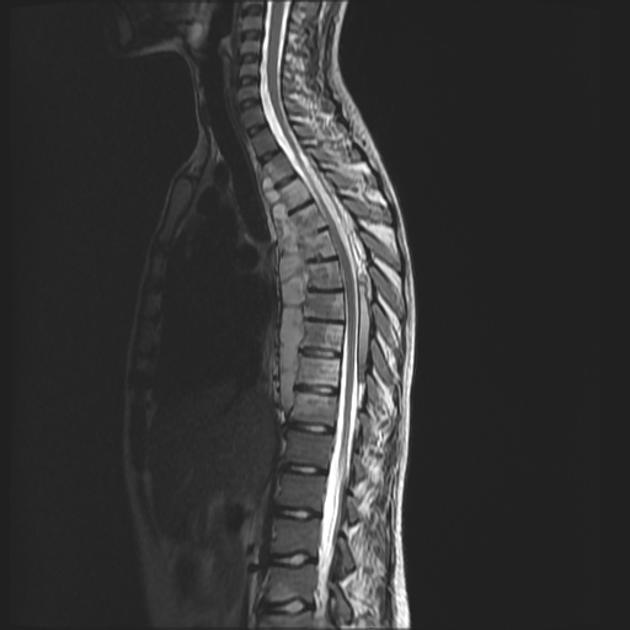
Gradual anterior collapse typically results in an acute kyphotic or gibbus deformity. This angulation, coupled with epidural granulation tissue and bony fragments, can lead to cord compression.
Central involvement
Spread via the venous plexus of Batson typically results in infection arising centrally within the vertebral body 2,8. This is more common in older individuals.
Gradual collapse can result in vertebra plana and acute kyphotic or gibbus deformity. This angulation, coupled with epidural granulation tissue and bony fragments, can lead to cord compression.
Posterior involvement
Posterior involvement, also known as an appendiceal pattern is similarly due to venous hematogenous spread via the posterior venous plexus.
Synovial/joint involvement
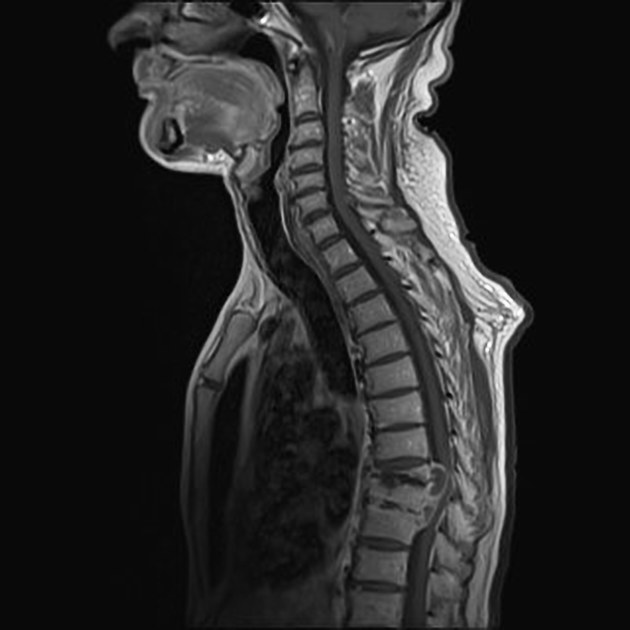
Synovial involvement is relatively rare but can be seen involving facet joints and atlantoaxial and atlanto-occipital joints.
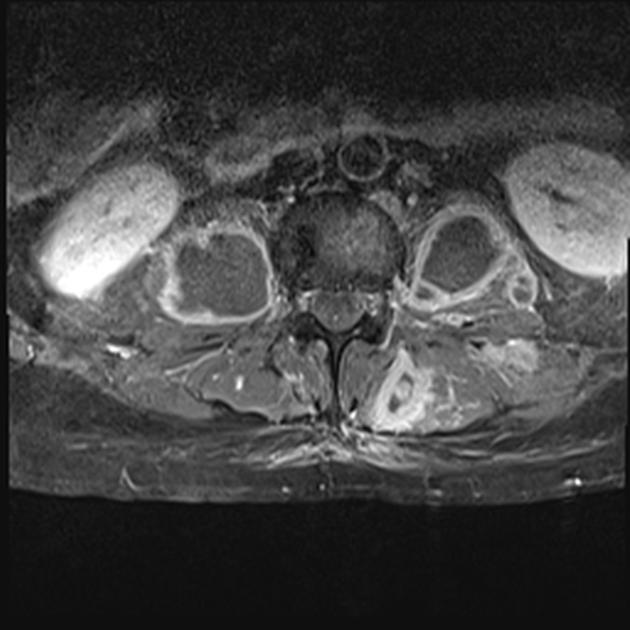
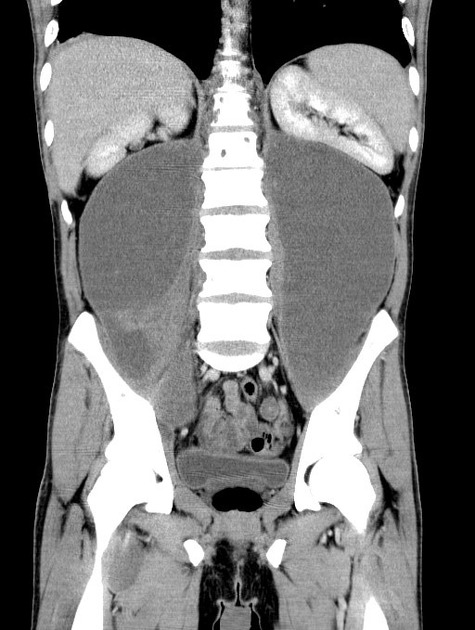
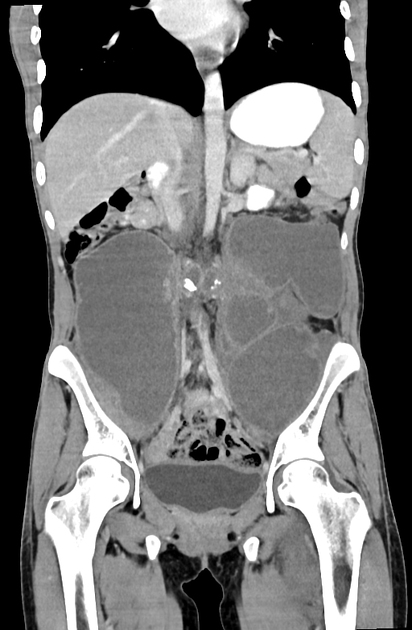
Cold abscess
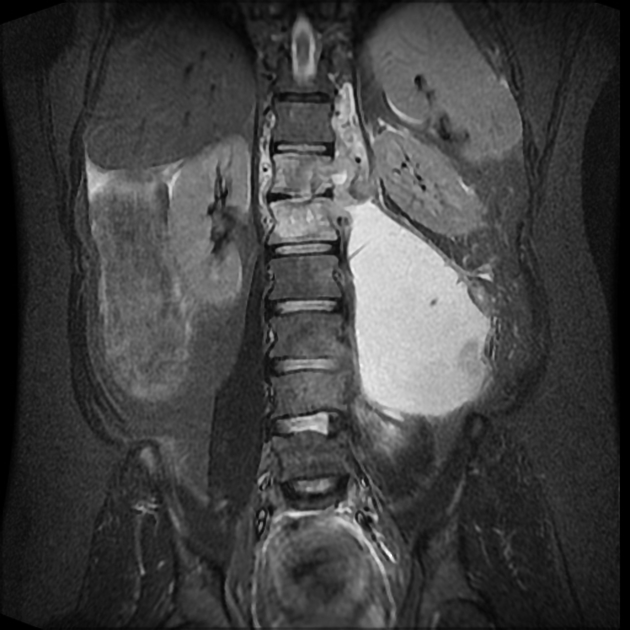
In late-stage spinal tuberculosis, large paraspinal abscesses can develop without severe pain or frank pus or prominent inflammatory signs and symptoms; thus "cold abscess".
Radiographic features
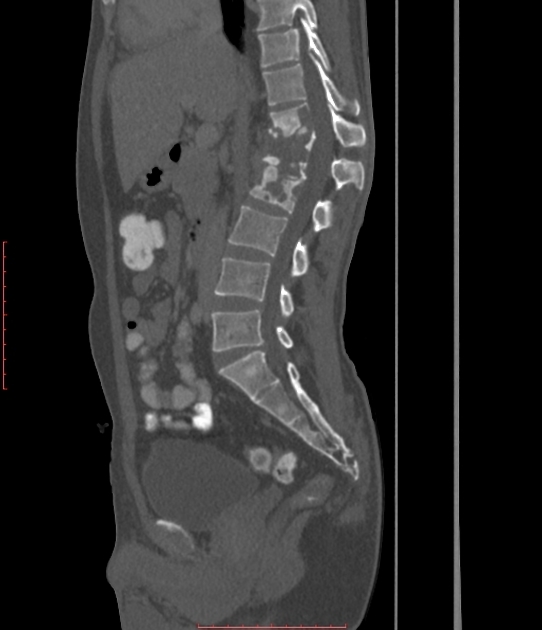
Plain radiograph
The spread of infection is typically described as 'subligamentous': beneath the anterior longitudinal ligament, usually sparing the posterior elements and often involving multiple levels.
Tuberculous spondylitis can be difficult to detect in early stages because of relative preservation of the disc space.
A reduction in vertebral height is often seen with the irregularity of the anterosuperior endplate being relatively early and subtle sign. Due to the subligamentous extension, there may be some irregularity of the anterior vertebral margin. This is a classical appearance with TB spondylitis.
Later, paraspinal collections can develop which can be remarkably large.
Ivory vertebrae can result in re-ossification. Other associated features may include:
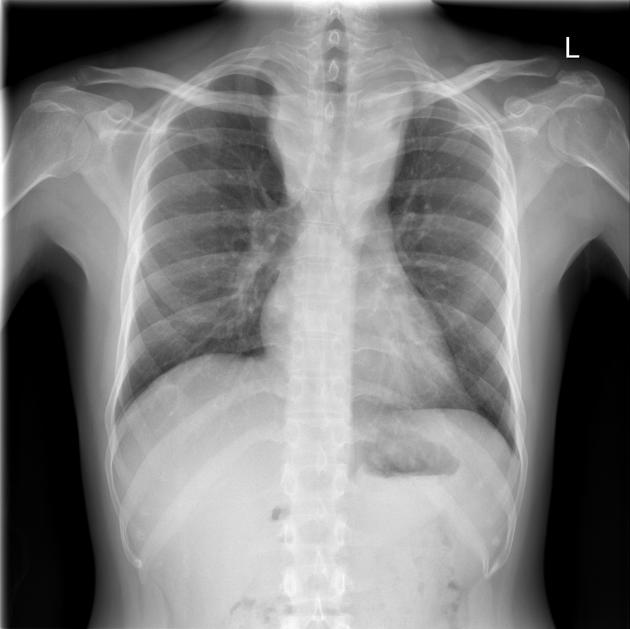
As with other extrapulmonary TB, a plain chest radiograph is often unremarkable (no pulmonary lesions seen in up to 50% of cases), with the source being a primary lung lesion that is clinically silent.
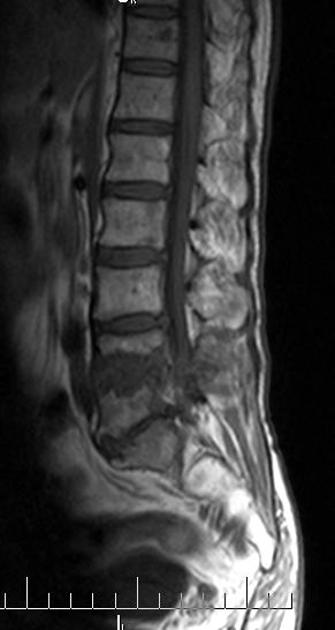
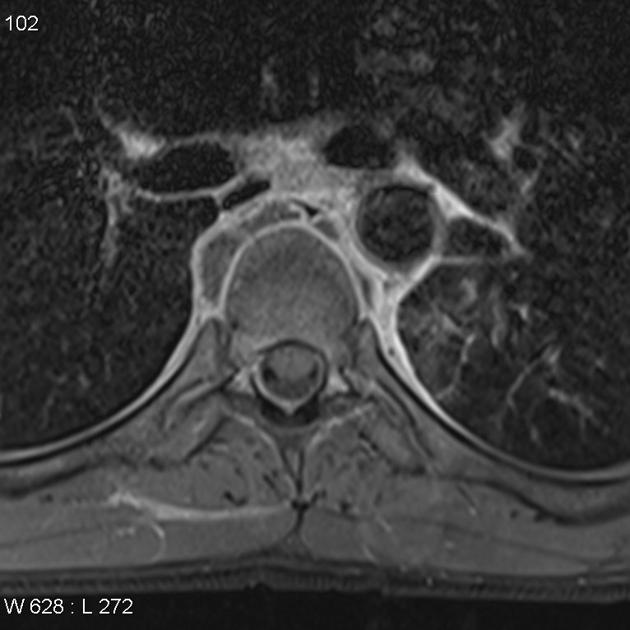
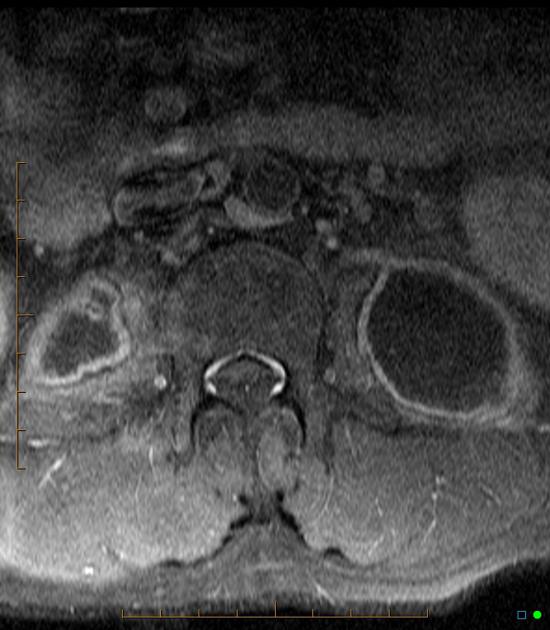
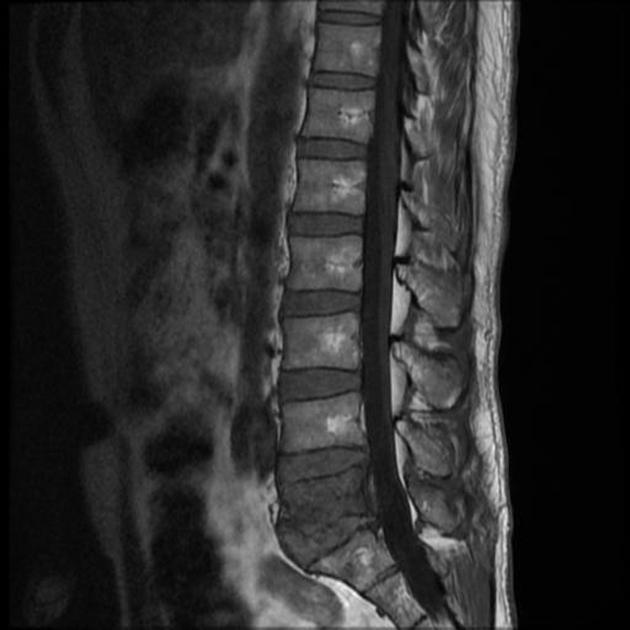
CT and MRI
Cross-sectional imaging is required to better assess the extent of involvement and particularly for the presence of an epidural component and cord compression. MRI is the modality of choice for this, with CT with contrast being a distant second.
Features include irregularity of both the endplate and anterior aspect of the vertebral bodies, with bone marrow edema and enhancement seen on MRI:
T1: hypointense marrow in adjacent vertebrae
T2: hyperintense marrow, disc, soft tissue infection
T1 C+ (Gd): marrow, subligamentous, discal, dural enhancement
The paraspinal collections are typically well-circumscribed, with fluid centers and well-defined enhancing margins 7.
History and etymology
Pott disease is named after English surgeon Percivall Pott (1714-1788) who first described tuberculosis affecting the spine in 1779 9. Many sources erroneously cite this description as occurring in 1799, which is actually after Pott's death 10.
Differential diagnosis
In many parts of the developing world, TB is the most common cause of vertebral body infection, with the majority of cases seen in patients under the age of 20. TB can also affect the meninges of the spine, causing an intense pachymeningitis that enhances dramatically.
-
infections
pyogenic infection: compared to pyogenic infection tuberculous spondylitis has relatively preserved disk-space height, forms large paraspinal abscesses with a smooth enhancing wall and there is usually systemic involvement of multiple organs. See: tuberculous spondylitis versus pyogenic spondylitis
-
brucellosis: can present as granulomatous osteomyelitis of the spine that can be difficult to distinguish from TB. Both are acid-fast bacilli, which may cause caseating granuloma(s)
fungal infection (e.g. cryptococcosis)



























 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.