Rasmussen encephalitis, also known as chronic focal encephalitis, is a chronic inflammatory disease of unknown origin, usually affecting one brain hemisphere.
It is not to be confused with a Rasmussen aneurysm.
On this page:
Epidemiology
Most cases (85% of cases) occur in children under the age of 10 years 1. However, detection in adults is increasing with routine MRI investigations for intractable seizures 5.
Clinical presentation
Clinically, Rasmussen encephalitis can be considered in three stages 17:
-
prodromal stage
infrequent seizures, usually focal seizures
mild focal neurological deficits, e.g. subtle hemiparesis
-
acute stage
frequent seizures due to drug-refractory focal epilepsy, including epilepsia partialis continua and focal-to-bilateral tonic-clonic seizures
progressive focal neurological deficits, e.g. hemiparesis, dysphasia (if dominant hemisphere), homonymous hemianopia
cognitive impairment may develop
-
residual stage
ongoing drug-refractory focal epilepsy
permanent and stable focal neurological deficits and cognitive impairment
Pathology
Pathologic features are similar to viral encephalitis, with lymphocytes surrounding round cells and diffuse proliferation of microglia. The observed inflammatory changes in Rasmussen encephalitis include perivascular cuffing, microglial nodules, T-lymphocytic infiltration gliosis, meningeal inflammation, and neuronal injury or loss 9,10. In the later phases, spongiform degeneration and cortical atrophy manifest.
The exact cause of the disease is unknown. However, various viral (SSPE-like, EBV or CMV) or inflammatory episodes have been implicated by different authors 3,4,6. Additionally, an autoimmune mechanism has also been proposed describing antibodies against the GluR3 subunit of the α-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid (AMPA) receptor in a few patients 11,17.
Radiographic features
Radiographic features are usually isolated to a single hemisphere; however, bilateral Rasmussen encephalitis has also been described in numerous case reports 12-14.
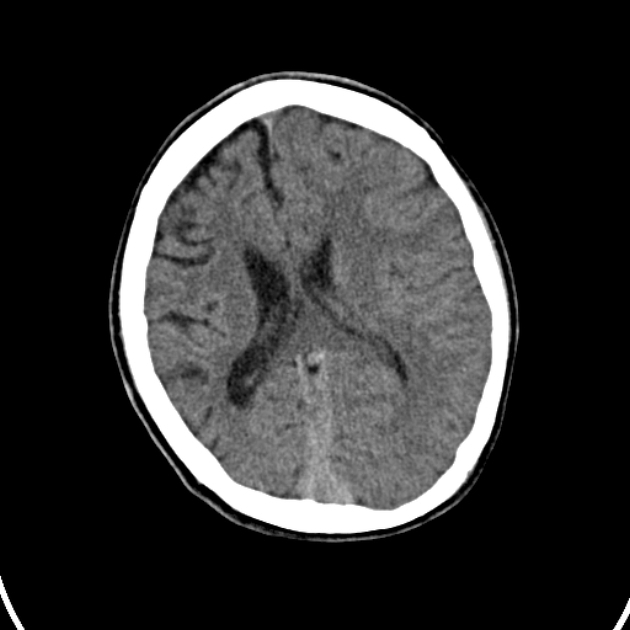
CT
CT may not show any specific feature in early imaging; however, patchy hypodense attenuation areas (similar to viral encephalitis) may be seen. The late-stage disease may show unilateral cortical atrophy. CT perfusion may show decreased cerebral blood flow (CBF) 1.
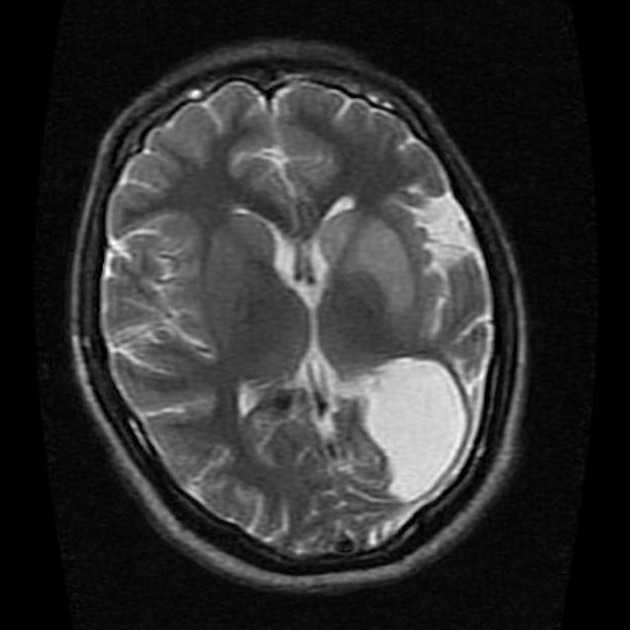
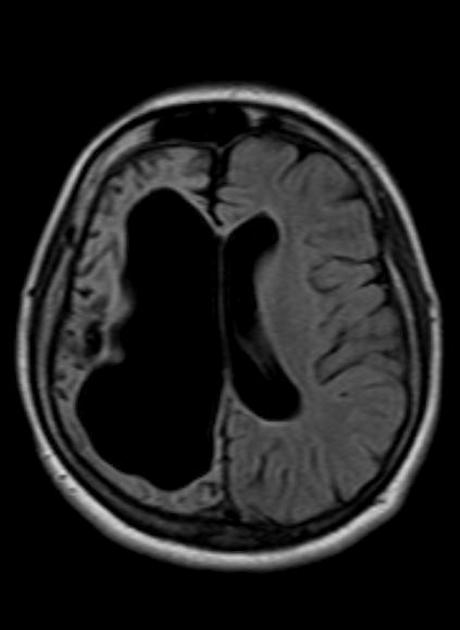
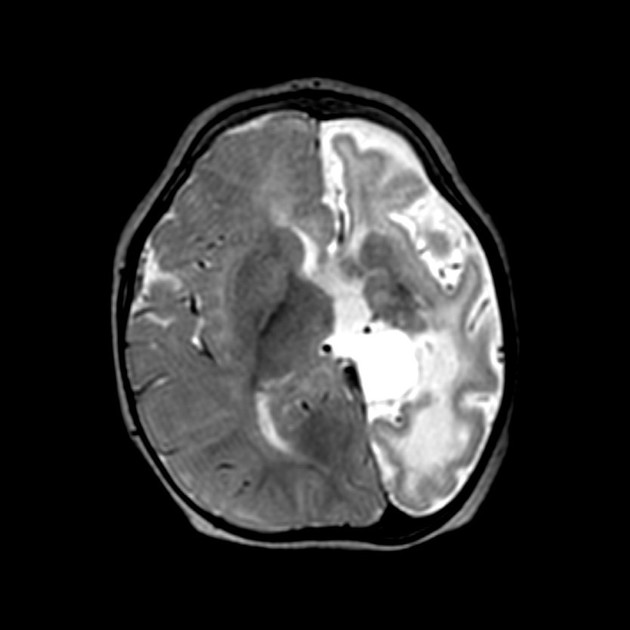
MRI
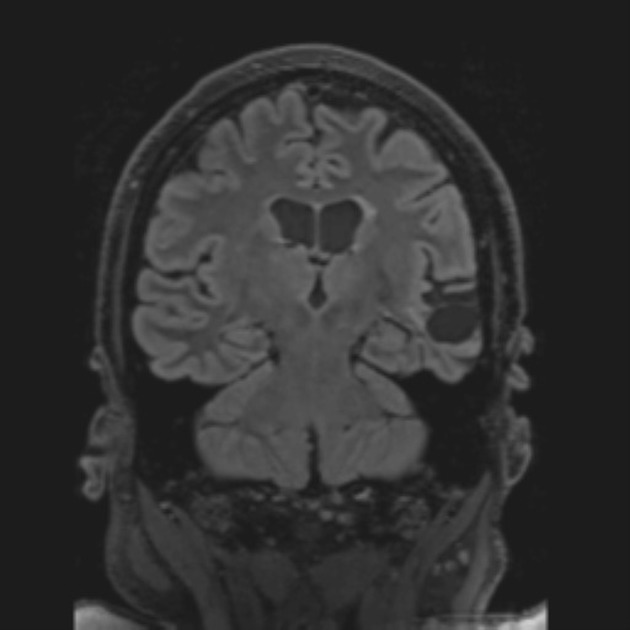
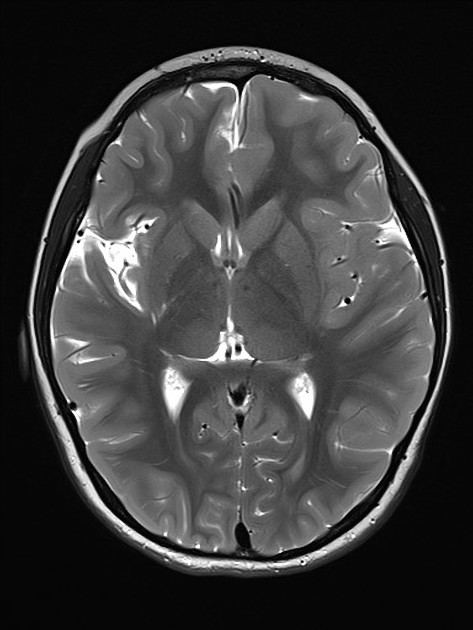
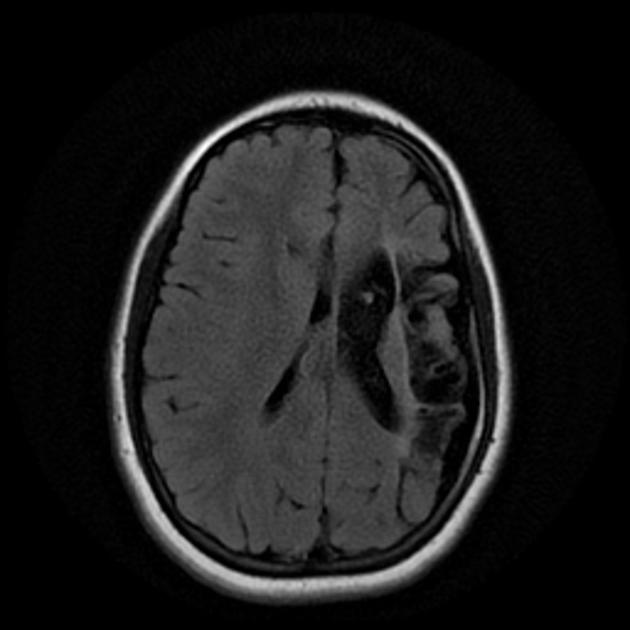
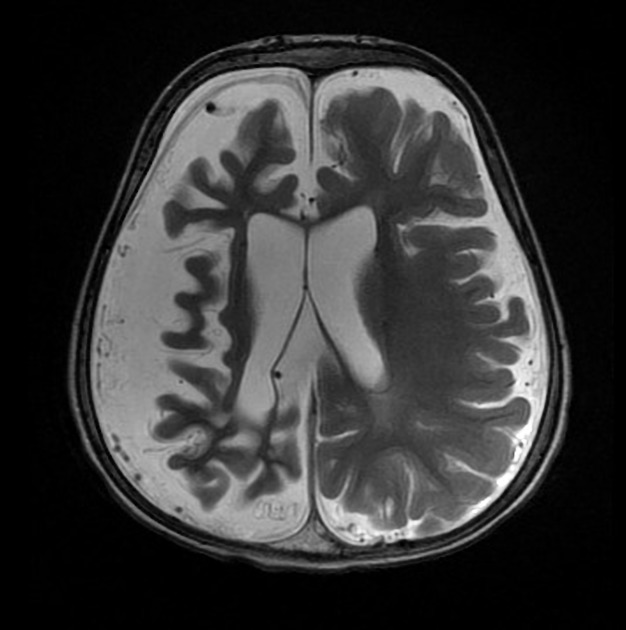
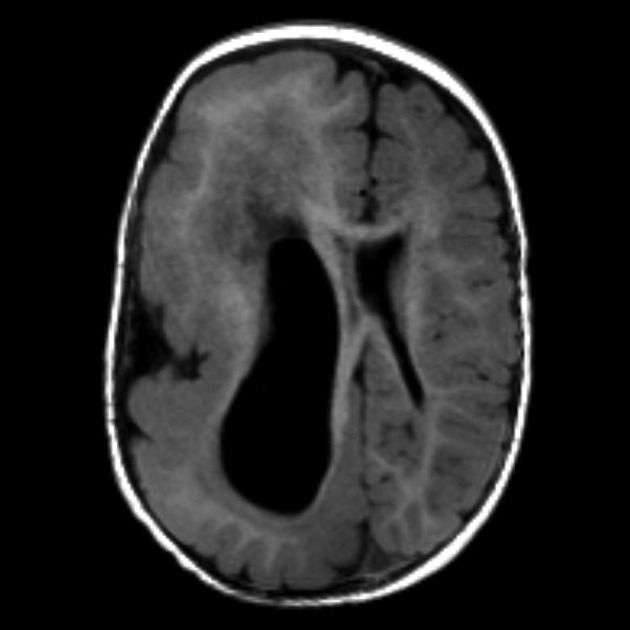
Atrophy is typically earliest appreciated in the ipsilateral caudate nucleus, before atrophy and signal changes are appreciated more generally in the hemisphere. Signal characteristics include:
T1: unilateral cortical atrophy with ex vacuo ventricular dilatation 15
T2: hyperintense signal areas in the cortical and subcortical regions of the affected hemisphere 15
DWI/ADC: restricted diffusion may be seen in altered signal areas 15
T1 C+ (Gd): no significant post-contrast enhancement 15
Treatment and prognosis
Treatment with immunosuppression (e.g. high-dose methylprednisolone, intravenous immunoglobulin, plasma exchange) has been positive in the acute stage, further supporting the autoimmune nature of the disease 16,17.
Antiseizure medications have a symptomatic role, but epilepsy due to Rasmussen encephalitis tends to be drug-refractory in nature 17. Hemispherectomy or functional hemispherectomy are the only definitive treatments for epilepsy in drug-refractory cases, which resolves seizure activity or significantly decreases seizure frequency in most patients 16.
History and etymology
It was first described by Theodore Brown Rasmussen (1910-2002), American neurologist, in 1958 2.
Differential diagnosis
General imaging differential considerations include:
Dyke-Davidoff-Masson syndrome: associated with calvarial changes
hemiconvulsion-hemiplegia epilepsy (HHE) syndrome: usually shows a seizure-free interval of months to years from initial presentation 7,8








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.