Rathke cleft cysts, also known as pars intermedia cysts, are non-neoplastic, sellar or suprasellar epithelium-lined cysts arising from the embryologic remnants of Rathke pouch in the pituitary gland. They are common lesions and usually incidentally identified.
On this page:
Epidemiology
-
common
found in ~20% (range 11-33%) of autopsies 2,6,17
prevalence on imaging is dependent on technique and field strength 16
-
rare in childhood; mostly seen in adults with a peak incidence at 30-50 years 17
since the underlying substrate is congenital, lesions thought to enlarge throughout life 2
recognized female preponderance (F:M = ~2:1) 17
Clinical presentation
The vast majority of Rathke cleft cysts, particularly when <3 mm, are asymptomatic and incidentally found 3.
If large, they may cause:
visual disturbances: due to compression of the optic chiasm
-
pituitary dysfunction
common but not necessarily clinically evident
due to compression of adjacent pituitary tissue and distortion of the pituitary stalk
present in up to 69% of symptomatic cases 10
increase in prolactin most common due to stalk effect 15
headaches 3
When presenting in childhood, growth impairment and precocious puberty are commonly encountered 14,15.
Pathology
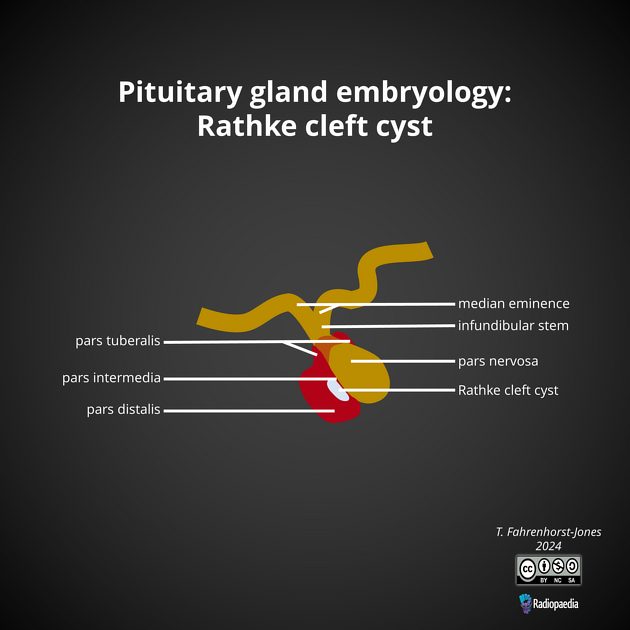
Rathke pouch forms during the 3rd and 4th week of embryologic development as a rostral outpouching from the roof of the primitive oral cavity 16. The anterior wall of the pouch gives rise to the anterior lobe of the pituitary (pars distalis). The posterior wall of the pouch does not proliferate and remains as the intermediate lobe of the pituitary (pars intermedia). The lumen of the pouch narrows to form a cleft (Rathke cleft) that normally regresses. Persistence of this cleft with the expansion is believed to be the origin of a Rathke cleft cyst 16.
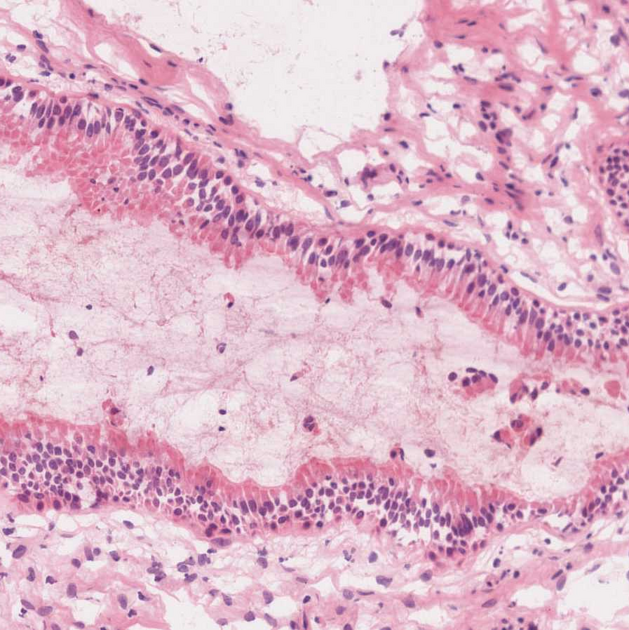
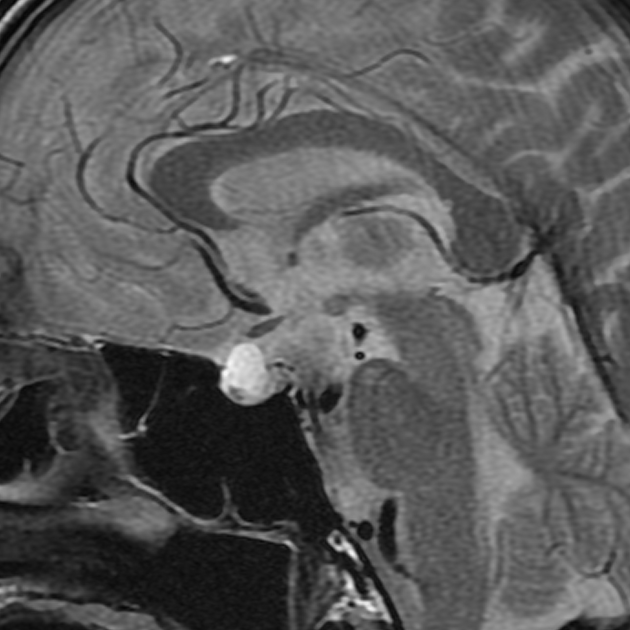
The wall of the cyst is typically lined by a single columnar cell layer of epithelium, often containing goblet cells, and is often ciliated. An intraluminal nodule which macroscopically appears white and is often adherent to the cyst wall (although it may be free-floating) is composed of solid tissue that represents desquamated cellular debris 3,10.
Radiographic features
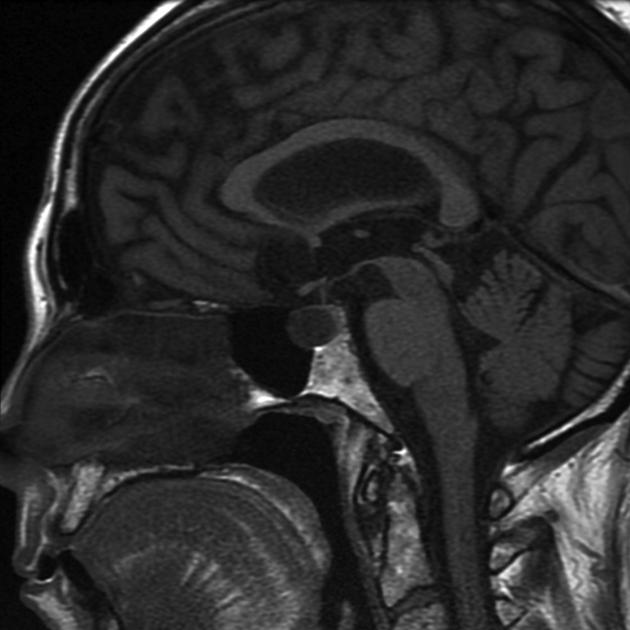
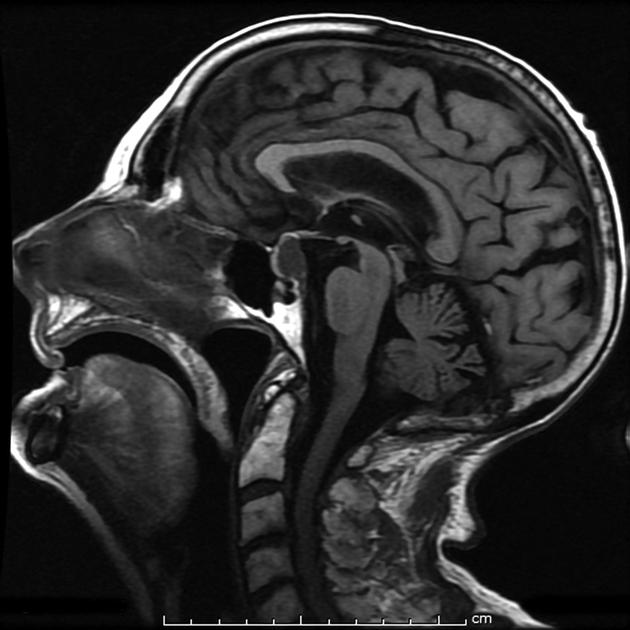
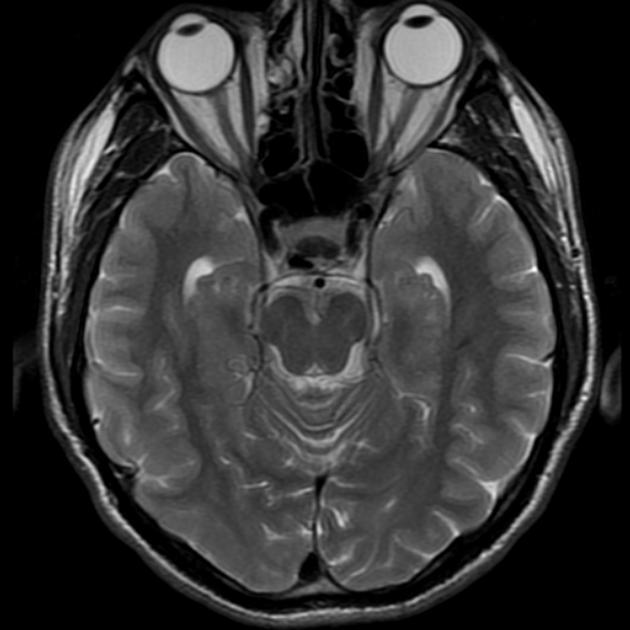
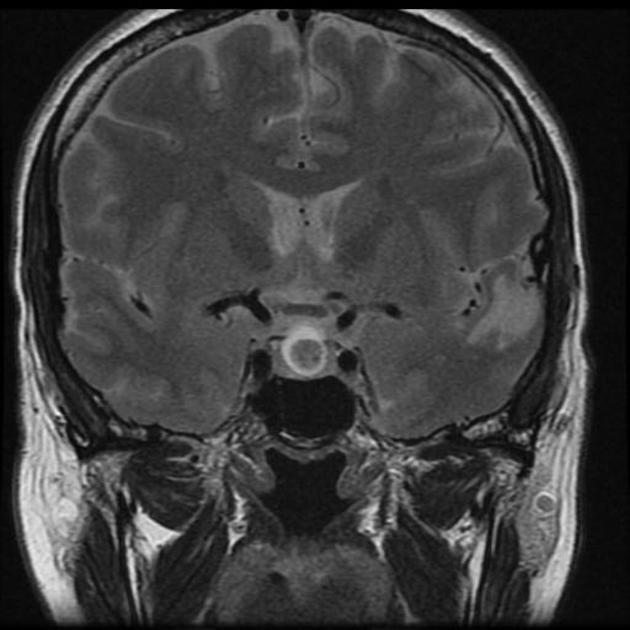
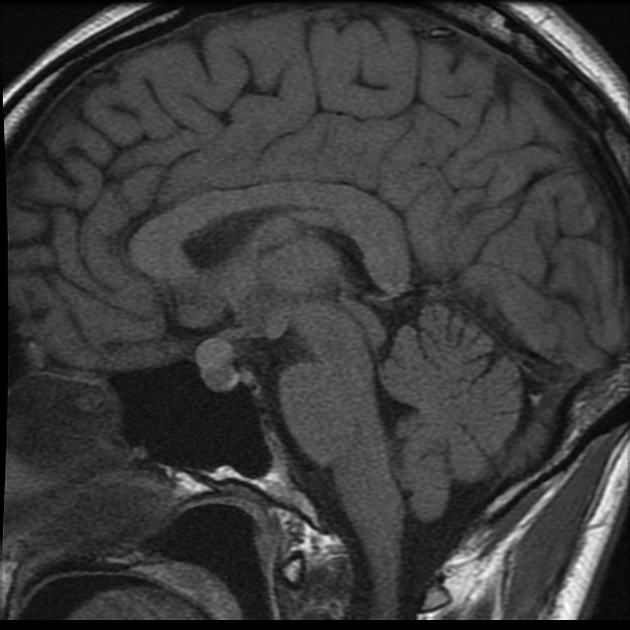
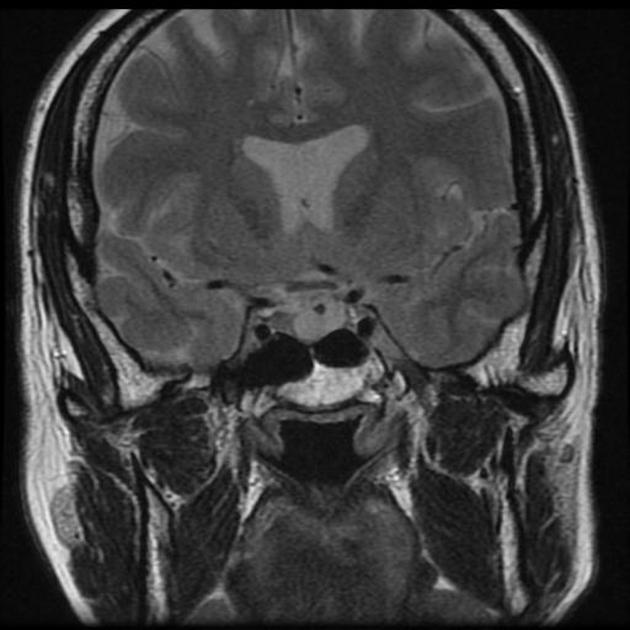
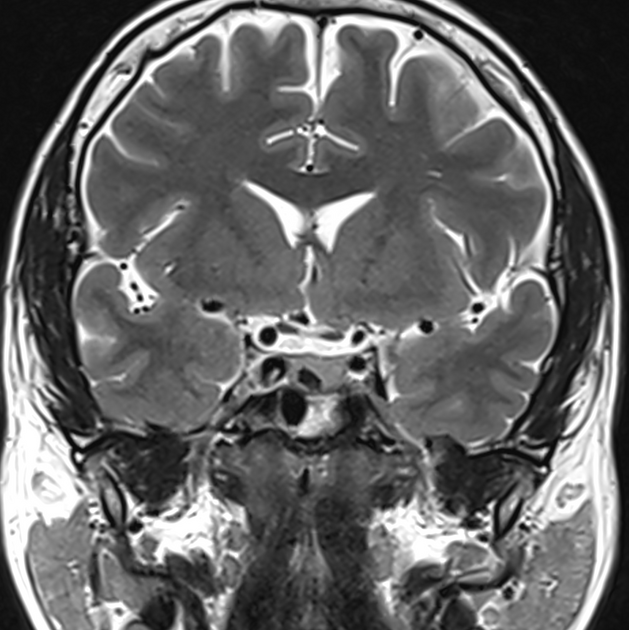
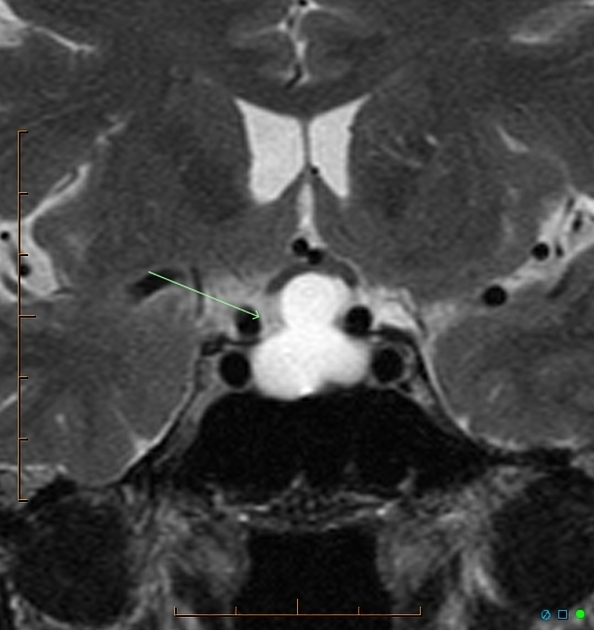
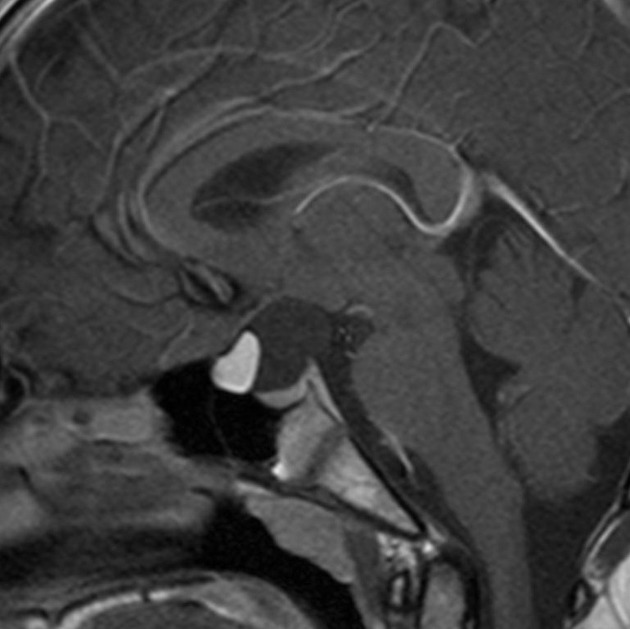
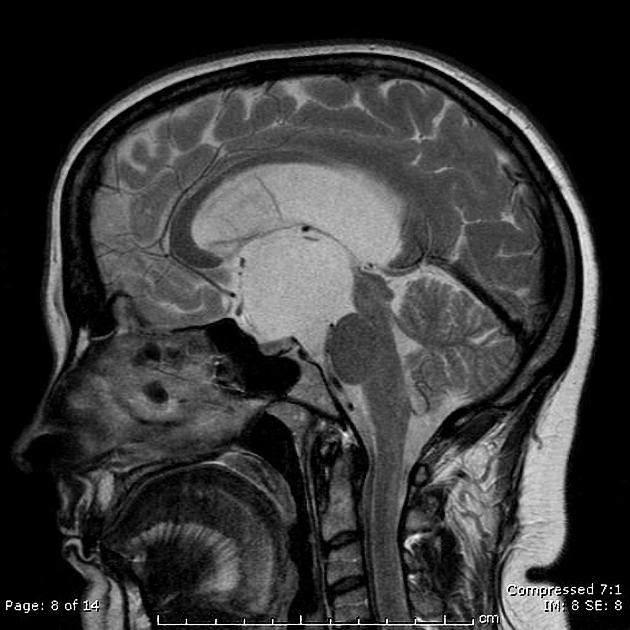
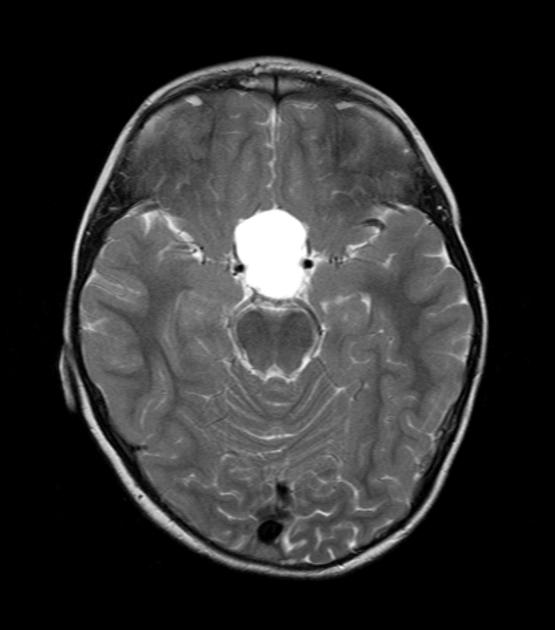
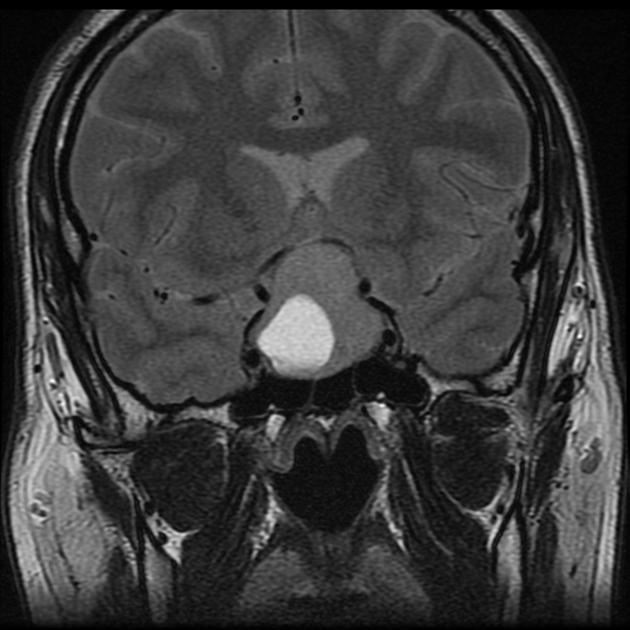
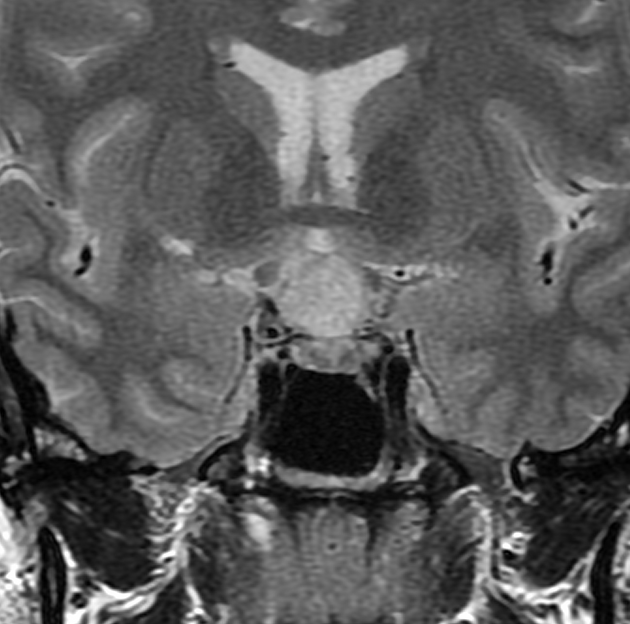
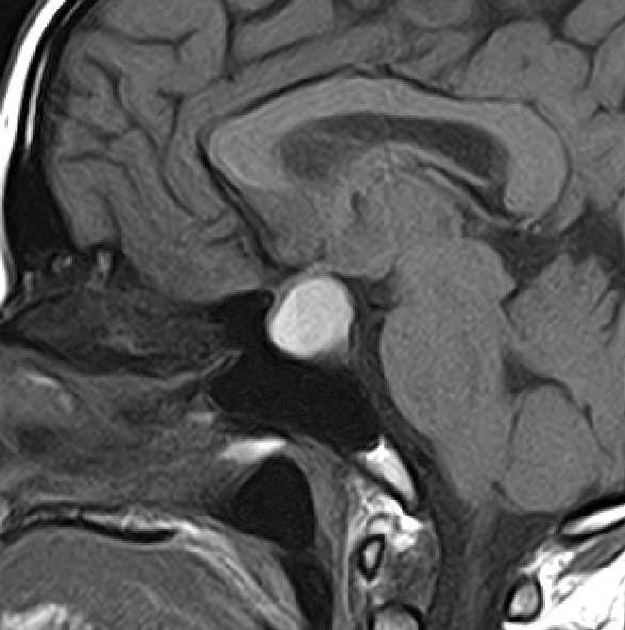
On imaging, a Rathke cleft cyst is seen as a well defined non-enhancing midline cyst within the sella arising between the anterior and intermediate lobes of the pituitary. 40% are purely intrasellar and 60% have suprasellar extension. Purely suprasellar location, although reported, is rare.
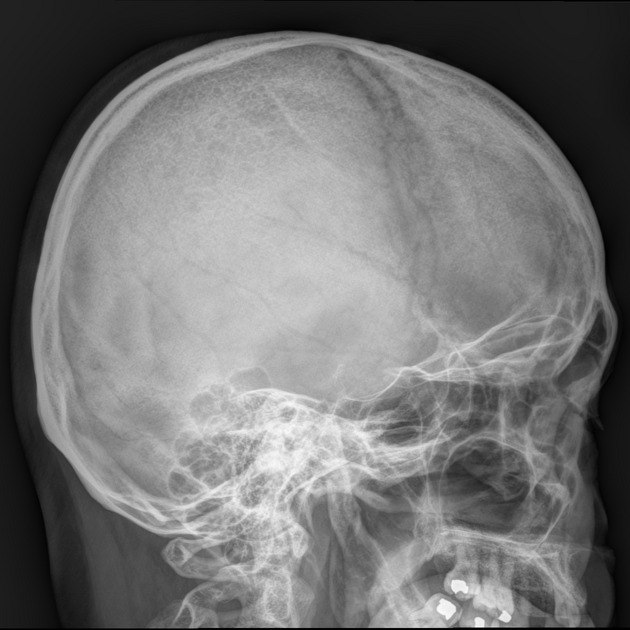
Plain radiograph
On lateral skull x-rays, Rathke cleft cysts can rarely cause sellar enlargement, although this is non-specific, if they reach a large enough size 12.
CT
-
non-contrast
typically non-calcified and of homogeneous low attenuation
uncommonly it may be of mixed iso- and low-attenuation, or contain small curvilinear calcifications in the wall (seen in 10-15% of cases)
-
post-contrast
typically non-enhancing, although the cyst wall may enhance in some cases 8
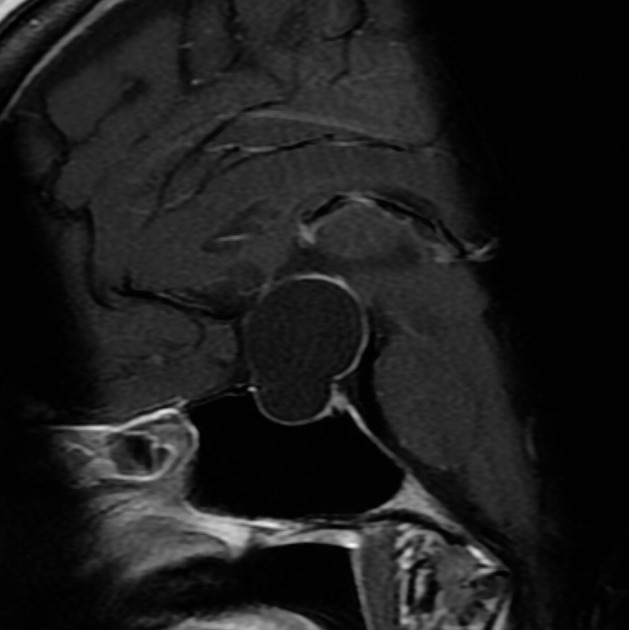
MRI
Rathke cleft cysts are usually in the midline, unicameral (without septations) and homogeneous in signal intensity 13. Fluid-fluid levels are uncommon and are more suggestive of a pituitary adenoma 13.
An intracystic nodule (sometimes referred to as cyst with dot sign) is present in ~70% (range 65-75%) of cases 3,13. When present it is usually hyperintense on T1 and hypointense on T2 compared to surrounding fluid, although, depending on the signal of the surrounding fluid, it may be inapparent on one sequence or the other 3.
Signal characteristics
The signal characteristics vary according to the cyst composition, which may be mucoid or serous:
-
T1
50% are hyperintense (high protein content)
50% are hypointense
-
T2
70% are hyperintense
30% are iso or hypointense
20% have a hypointense rim (this is more common in adenomas) 13
-
T1 C+ (Gd)
no contrast enhancement of the cyst is seen; however, a thin enhancing rim of surrounding compressed pituitary tissue may be apparent 9,10
Treatment and prognosis
Surgical treatment is indicated for cases with symptomatic mass effect.
The recurrence rate after surgical resection is ~17.5% (range 3-33%) 17, supporting the theory that a relationship exists between symptomatic Rathke cleft cyst and craniopharyngioma 11.
In children presenting with endocrinopathy (growth impairment and/or precocious puberty) hormone replacement and gonadotropin suppression may be effective 14.
Differential diagnosis
The main differential diagnoses are:
-
cleft like space without mass effect 16
found in the majority of scans if sufficiently high resolution
J or C shaped between anterior and postior pituitary
most likely represents a Rathke cleft (remnant of the Rathke pouch)
-
fluid-fluid level or hemorrhagic debris 11,13
off midline location 13
septations 13
-
no gender difference
similar age group
usually suprasellar or have a suprasellar component
tend to calcify
-
older patients
no gender difference
-
usually suprasellar
restriction on DWI
-
usually has solid components
often fatty signal










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.