Sacroiliitis (rare plural: sacroiliitides) is an inflammation of one or both sacroiliac (SI) joints. It is a common cause of buttocks or lower back pain and can manifest as a wide range of disease processes.
On this page:
Clinical presentation
Symptoms of sacroiliitis can vary. People with sacroiliitis commonly present with ipsilateral or bilateral buttock and/or midline lower lumbar area pain. Up to 50% may have pain radiating to the lower extremity.
Pathology
The causes of sacroiliitis can be unilateral or bilateral. See article: sacroiliitis (differential)
Classifications
New York criteria (plain radiograph)
Radiographic features
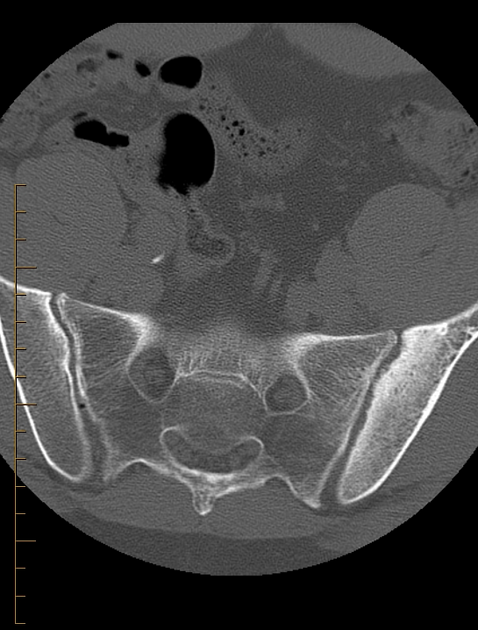
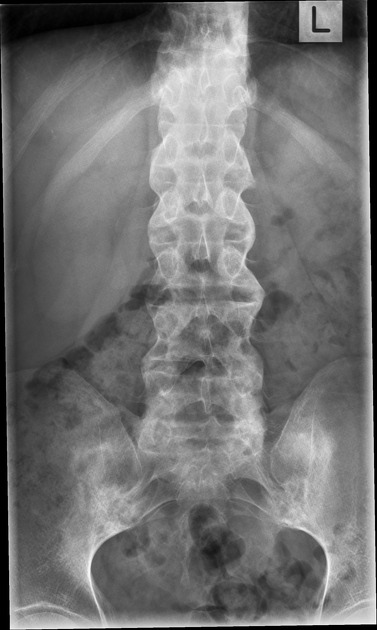
Plain radiograph
Conventional radiography remains the first line of imaging despite its poor sensitivity and specificity in early disease. Specific sacroiliac joint views are helpful in the evaluation and comparing both sides of sacroiliac joints.
Radiograph findings include:
sclerosis of the endplates particularly on the iliac side
irregular joint end plates
widening of joint spaces
ankylosis (end stage)
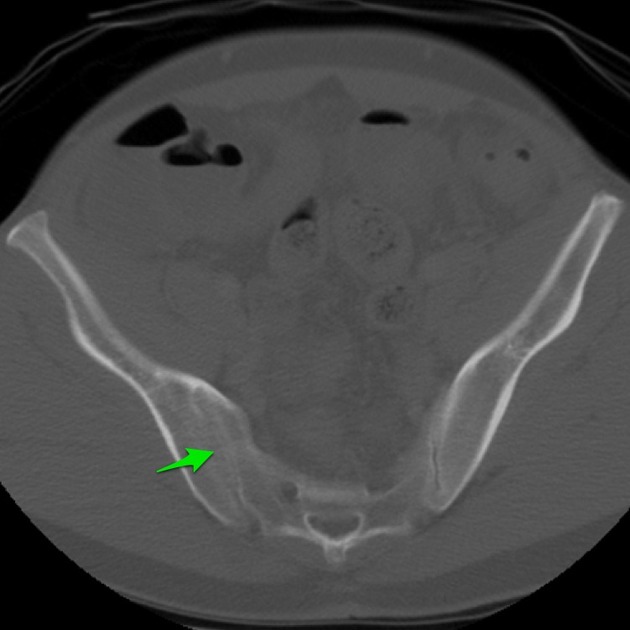
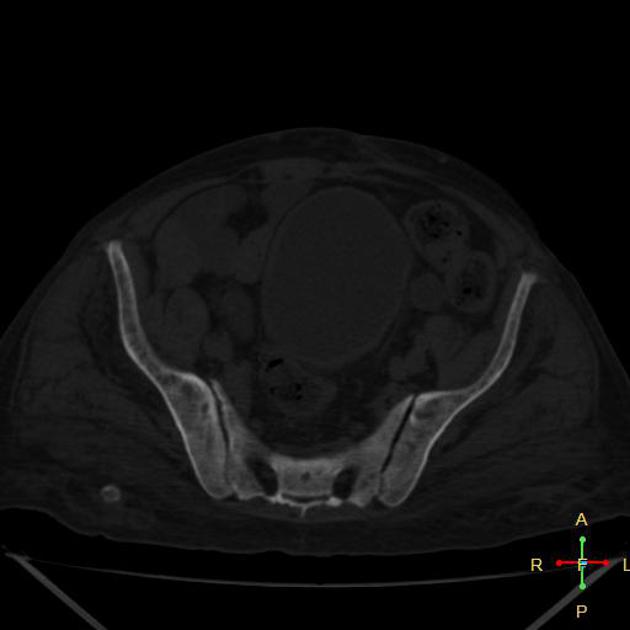
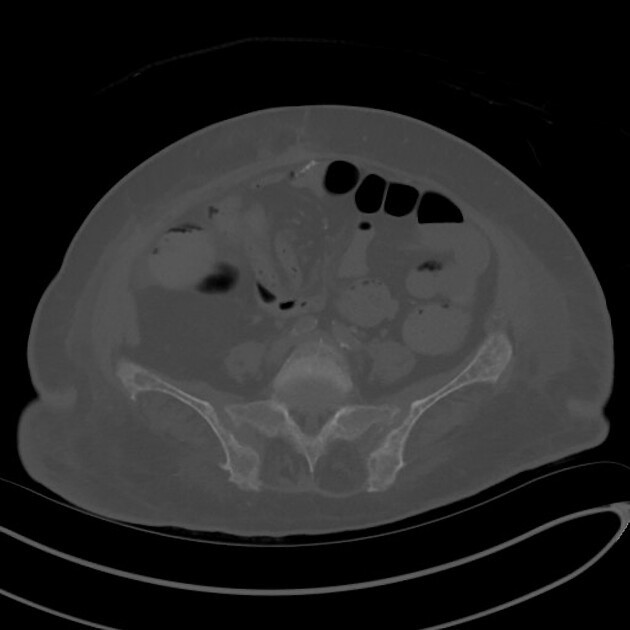
CT
CT examinations offer greater sensitivity, accuracy and detailed information compared to plain radiography. However, due to higher radiation exposure, it is not advisable to use CT for diagnosis or follow-up purposes.
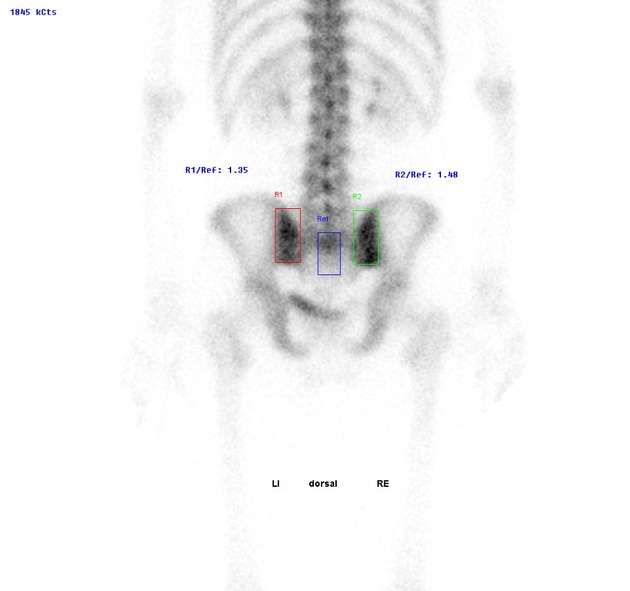
Nuclear medicine
Bone scans demonstrate increased radioisotope activity of the joints and helpful in localizing the source of the pain. It is also valuable in excluding stress fractures and other bone pathologies.
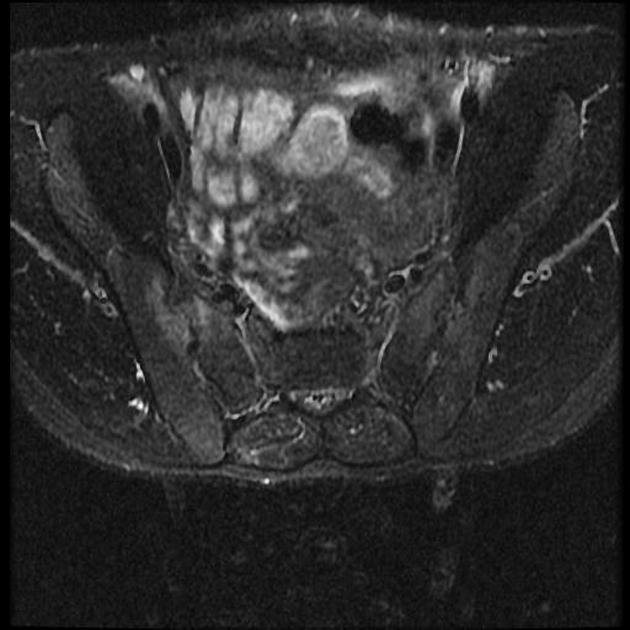
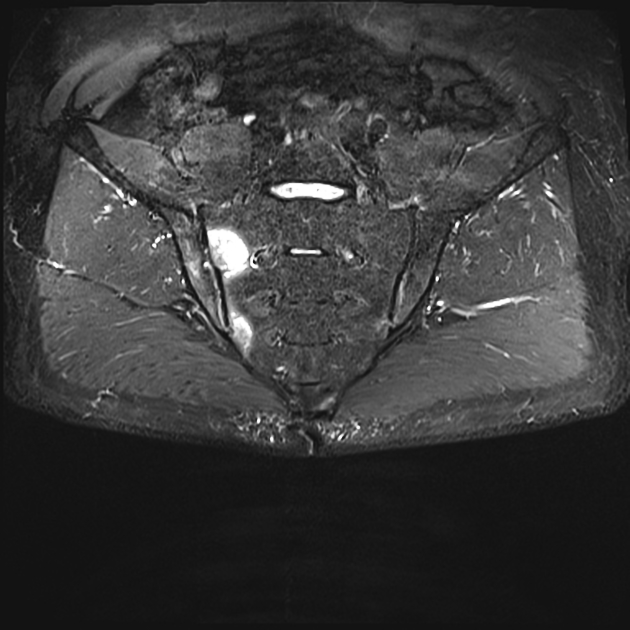
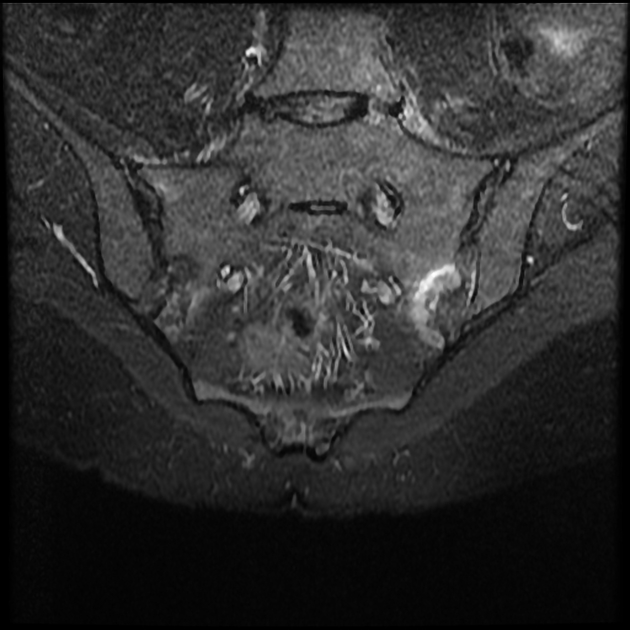
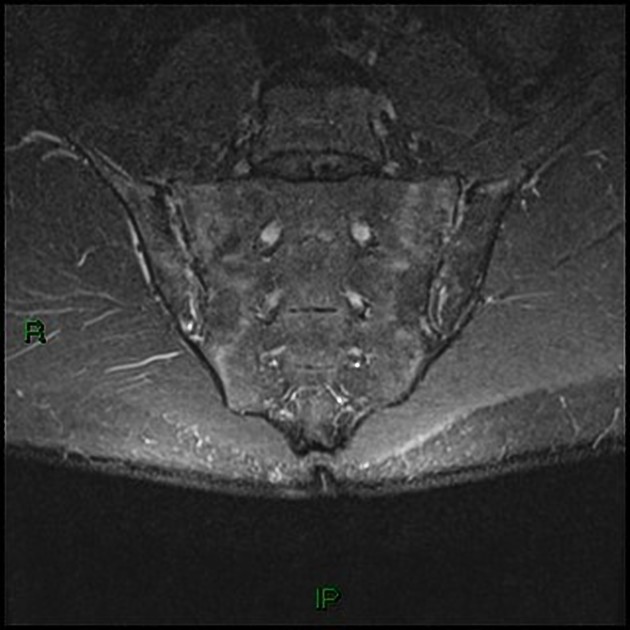
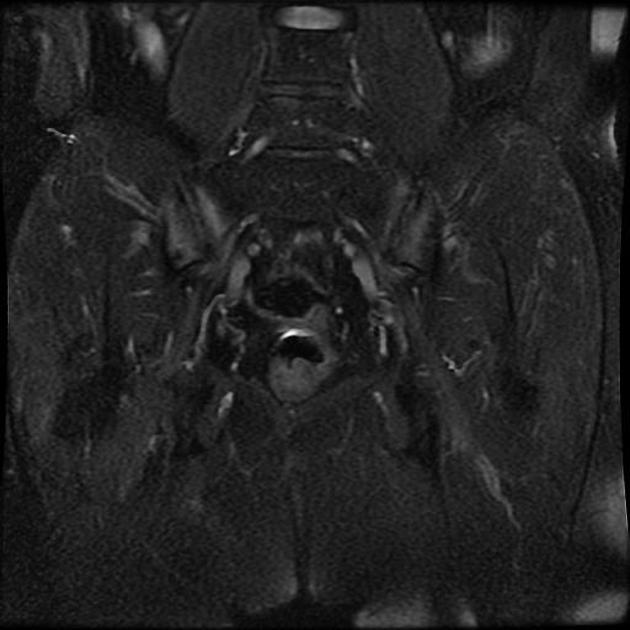
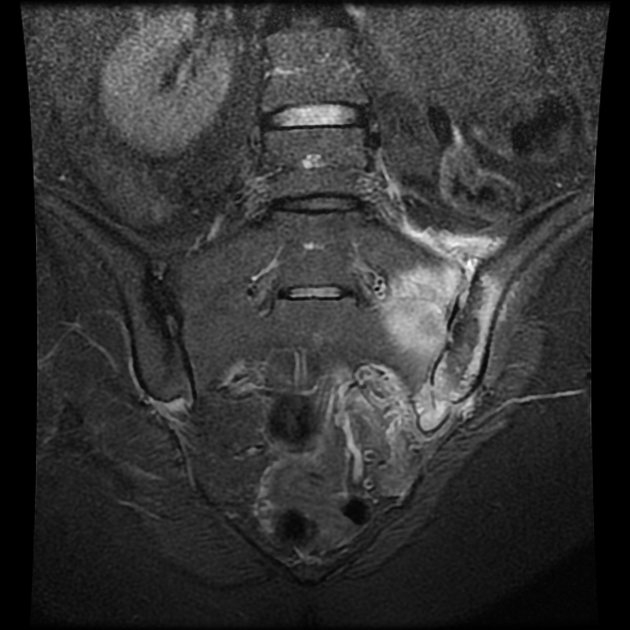
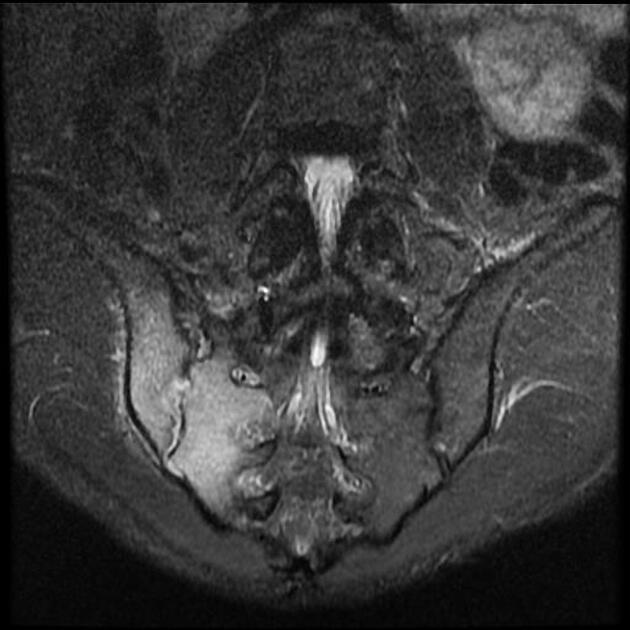
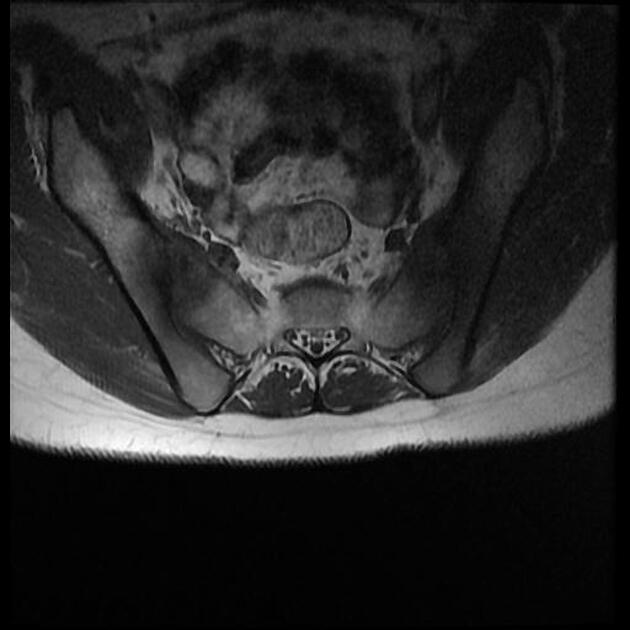
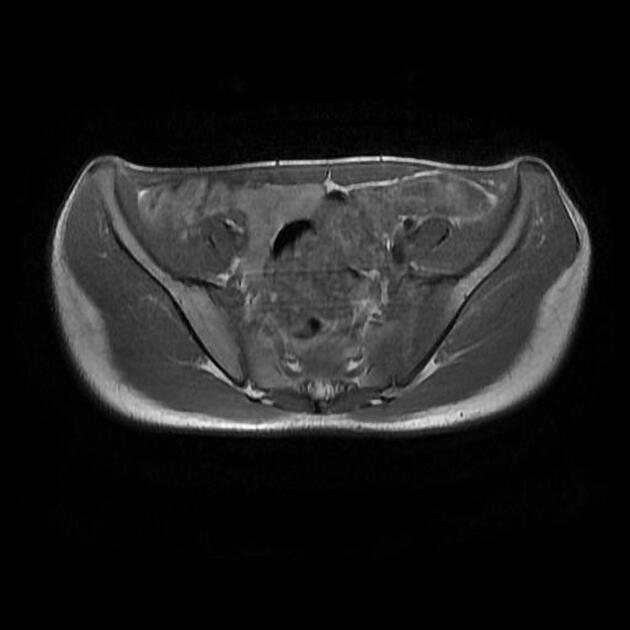
MRI
Though not routinely used for evaluating the sacroiliac joints, MRI is capable of identifying early inflammatory changes of joints when other imaging is negative and excludes other differential causes such as disc prolapse which may resemble clinical symptoms of sacroiliitis.
MRI features of sacroiliitis can be divided into inflammatory and structural lesions 6,7:
-
inflammatory lesions
marrow edema (first to appear): high signal on water sensitive sequences
synovitis and capsulitis: thickening and contrast enhancement of the synovium and joint capsule
enthesitis: thickening and contrast enhancement of ligaments and tendons at their attachments to bone
-
structural lesions
subchondral sclerosis: bands of low signal (on all sequences) paralleling the joint margins, at least 5 mm from the joint space
-
erosions: marginal foci of articular bone loss
low T1 signal
high T2/STIR signal if active
more prominent anteroinferiorly and on the iliac side of the SIJ
when confluent may appear as joint space widening
backfill: intra-articular high T1 signal filling up excavated bone erosions
fat metaplasia: periarticular fat deposition
ankylosis
Treatment and prognosis
Treatment depends on the underlying cause of the sacroiliitis. Physiotherapy may also be helpful in strengthening the pelvic muscle and increase the mobilization of the SI joint. Analgesics such as NSAIDs may be useful in symptomatic management. Corticosteroid injection to the affected sacroiliac joint can be performed to reduce inflammation and pain.
Surgical fusion of the SI joint is only considered as a last resort when conservative management is ineffective.
Differential diagnosis
The following conditions may mimic sacroiliitis:
hyperparathyroidism: not true sacroiliitis but mimics its appearances
osteitis condensans ilii: benign sclerosis on the iliac side of the joint











 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.