Solitary fibrous tumors of the thorax are rare pleural-based tumors that account for <5% of all primary pleural tumors 16. While their behavior is variable, they are typically indolent, benign-behaving tumors. Locally aggressive features with malignant transformation, into undifferentiated sarcoma, is possible but atypical.
On this page:
Terminology
Throughout much of the 20th century, there was a continual debate about the precise histology of both normal pleura and pleural tumors. The properties of the mesothelial cell itself were controversial, mostly due to its unique expression of both mesenchymal and epithelial attributes.
Gradually, a distinction was recognized between "localized" versus "aggressive" mesothelial tumors (i.e. "malignant" mesothelioma). Solitary fibrous tumors have been variably termed benign mesothelioma, localized fibrous tumor of the pleura, localized mesothelioma, localized fibrous mesothelioma, localized benign fibroma, pleural fibroma, submesothelial fibroma, hemangiopericytoma, or giant cell angiofibroma 10,16. "Solitary fibrous tumor of the thorax" is now the recommended term in the WHO classification of thoracic tumors (5th edition) 16.
Epidemiology
Solitary fibrous tumors usually present in the 6th to 7th decades with no gender predilection 16. They have an incidence of 2.8 in 100,000 11.
Associations
hypoglycemia (2-4%) 6: thought to be due to the production of insulin-like growth factor 2 (known as Doege-Potter syndrome)
hypertrophic pulmonary osteoarthropathy (~20%) 6: thought to be due to abnormal production of hyaluronic acid
asbestos exposure is not an association 15
Diagnosis
The diagnostic criteria according to the WHO classification of thoracic tumors (5th edition) are 16:
essential: well-circumscribed mass; spindled to ovoid cells arranged around a branching and hyalinized vasculature; variable stromal collagen deposition; CD34 and/or STAT6 expression by immunohistochemistry
desirable (in selected cases): demonstration of NAB2-STAT6 gene fusion
Clinical presentation
Usually asymptomatic and discovered as an incidental finding 3. Of those who are symptomatic, the clinical presentation can be with either a cough, chest pain, or shortness of breath 16.
Pathology
The etiology of solitary fibrous tumors is unknown. They are mostly slow-growing and benign-behaving, although a significant minority will demonstrate aggressive behavior 16. Rarely, they can transform into undifferentiated sacroma 16.
Location
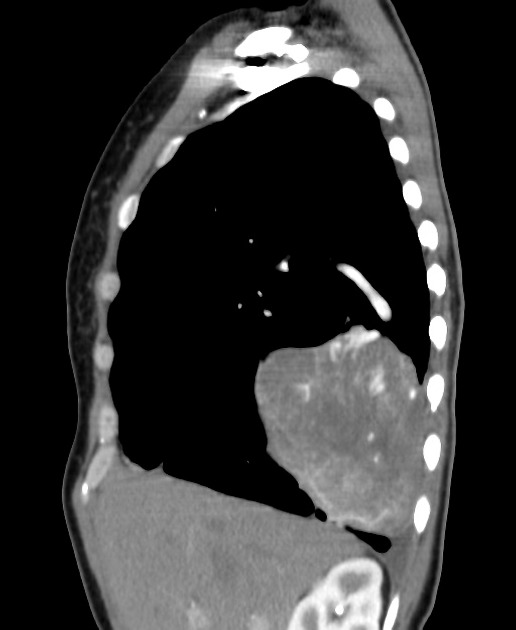
There may be a predilection towards the mid to lower zones of the chest. They arise from visceral pleura (~80%), parietal pleura, lung parenchyma (3%), pericardium, or rarely the mediastinum 12,16.
Microscopic appearance
Solitary fibrous tumors consist of uniform fibroblastic spindle cells with varying cellularity, featureless architecture, fibrosis and branching staghorn vessels. Myxoid or cystic degeneration can occur 16.
Classification
The use of "benign" or "malignant" in solitary fibrous tumors is not recommended. Risk stratification for likelihood of aggressive behavior (into low, intermediate, high categories) is preferred over staging 16. Various risk models have been proposed 16.
Radiographic features
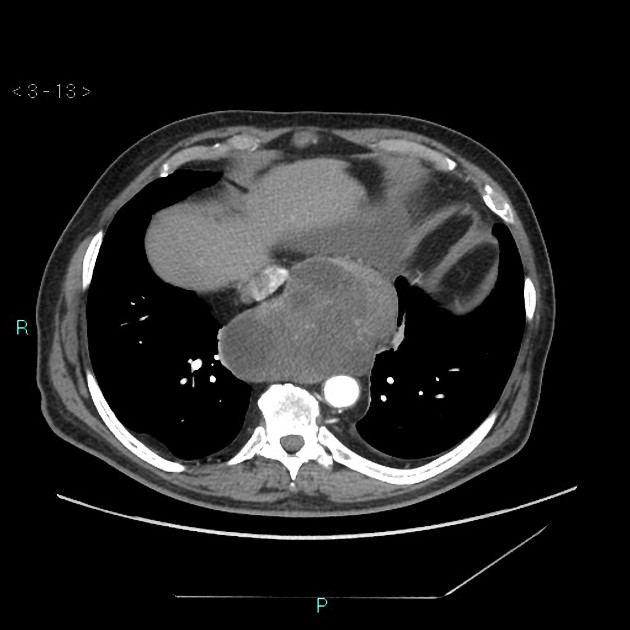
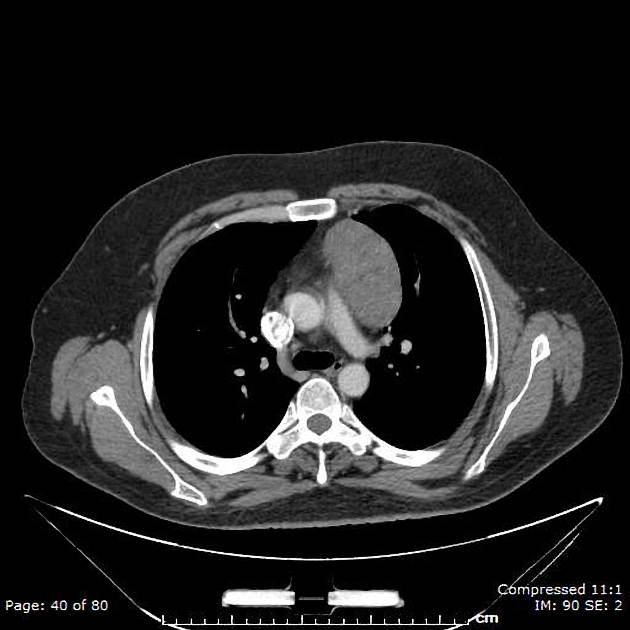
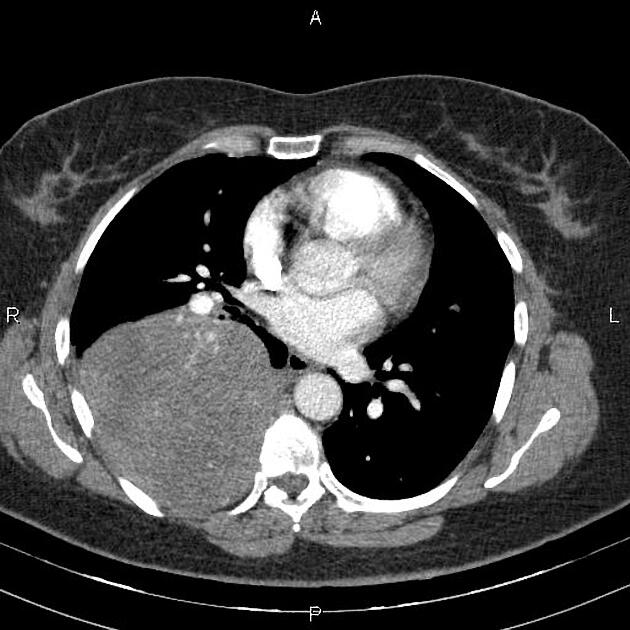
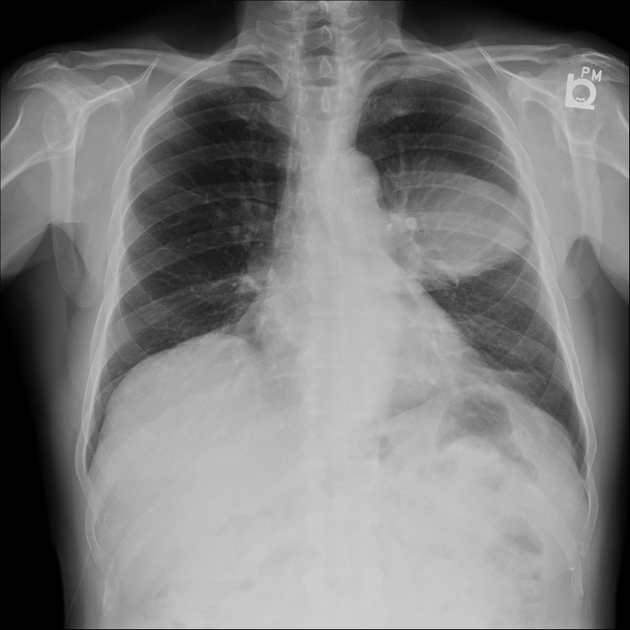
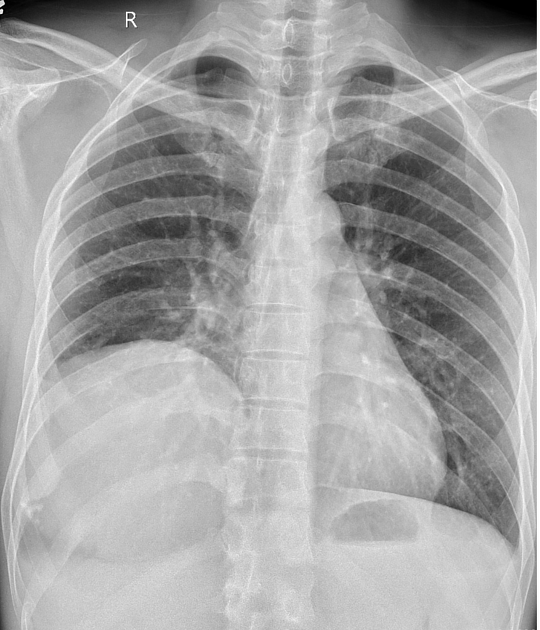
Plain radiograph
Presents as a pleural-based mass, which tends to be relatively circumscribed, but can also be lobulated. It often forms an obtuse angle with the chest wall and may grow to a large size. Pedunculated lesions can change position and appearance with respiration or with a change in position on serial radiographs.
Calcification, rib destruction, and pleural effusions are typically not associated features.
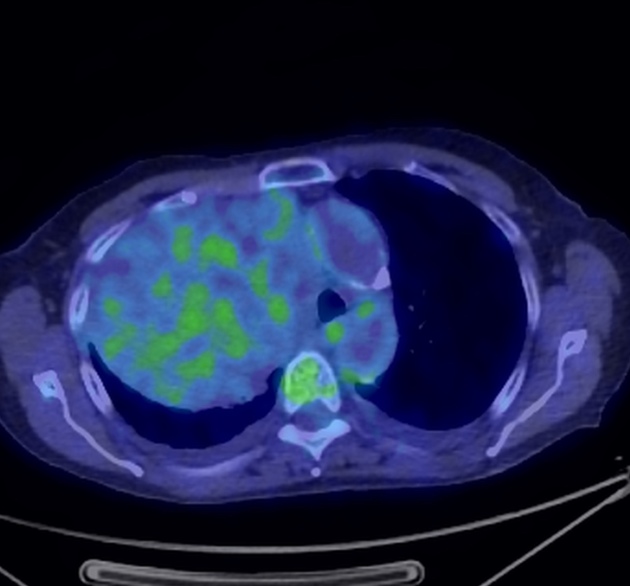
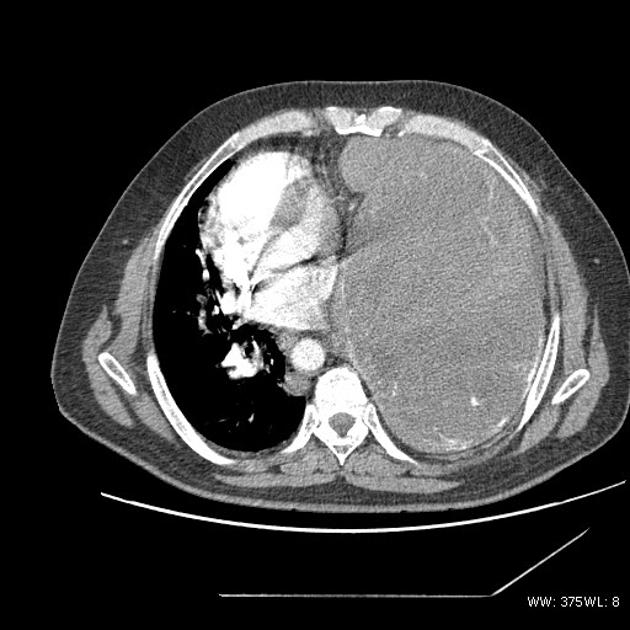
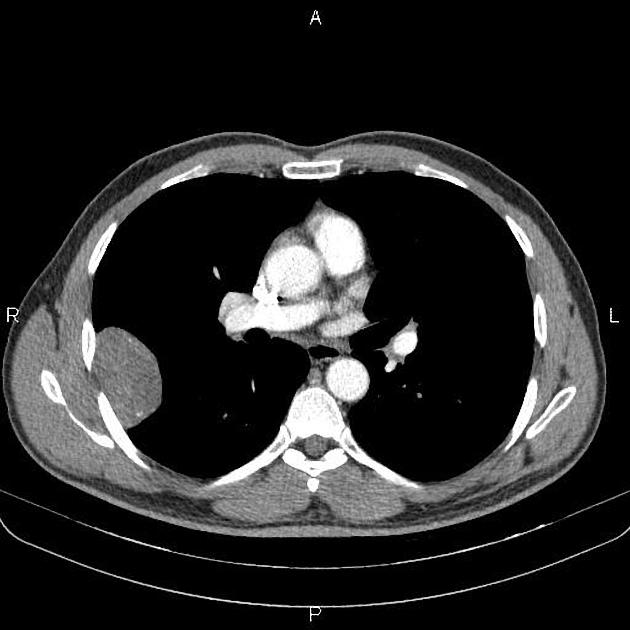
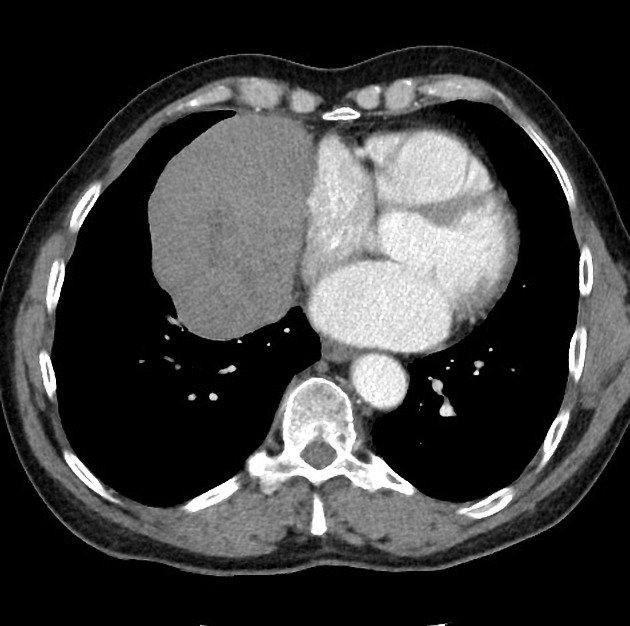
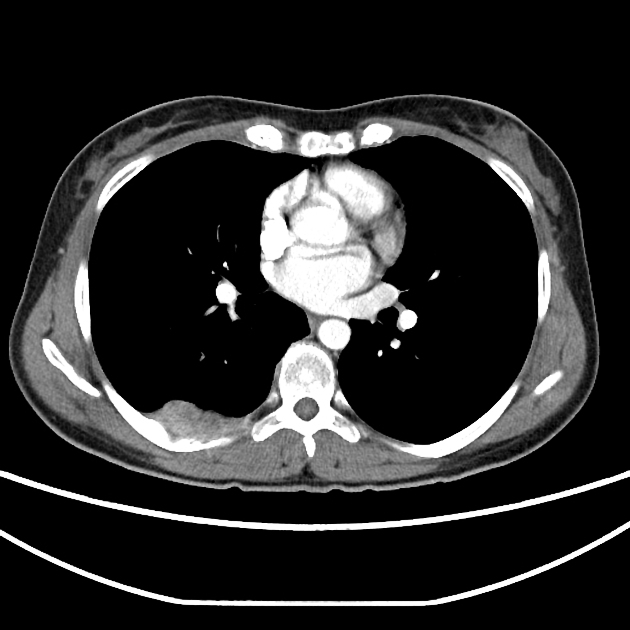
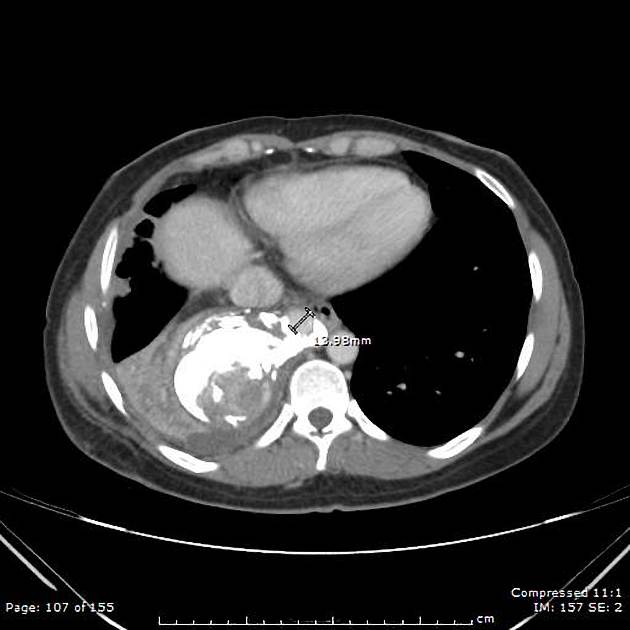
CT
Tends to have soft tissue attenuation on unenhanced scans and shows relatively homogeneous intense background enhancement on contrast-enhanced scans (from rich vascularization). Non-enhancing areas may be present, corresponding to necrosis, myxoid degeneration, or hemorrhage within the tumor. A pedicular attachment may also be seen. The incomplete border sign may be present in the portion of the mass contiguous with the pleura.
MRI
Due to the fibrous component, signal characteristics tend to be:
T1: typically low to intermediate signal
T2: typically low signal overall (thought to be due to high cellularity and abundant collagen); areas of necrosis and myxoid degeneration can have high signal
T1 C+ (Gd): In general, increased vascularity causes intense enhancement post intravenous gadolinium administration 14
MRI may also show necrotic, hemorrhagic, and cystic components in greater detail if these are present.
Treatment and prognosis
The majority of tumors tend to be indolent and slow-growing. Aggressive tumors occur at a rate of ~30% (range 10-57%) 12. Surgical resection is the treatment of choice 5,6. Chemotherapy and radiotherapy are used in the minority (<5%) of patients 12.
Solitary fibrous tumors can metastasize (in order of frequency) to the pleura, chest/abdominal wall, lung, peritoneum, and/or liver. Metastases to the brain or bone are rare 13.
Recurrence rates are ~18% (range 10-25%) and are higher with incomplete resection and a higher risk category 16. The 5-year survival is ~85% 12.
History and etymology
Understanding of primary pleural neoplasia has changed drastically since the late 1800s, and so the associated terminology has also changed. German pathologist Ernst Leberecht Wagner (1829-1888) is generally credited with the first description of pleural mesothelioma/fibroma in 1870, although he described it "tuberkelähnliche" lymphadenome ("tubercle-like" lymphadenoma) 9. Primary pleural malignancies were rare until the 20th century when the incidence increased considerably due to environmental exposures.
Differential diagnosis
Considerations for extremely well-defined lesions include:
intercostal nerve neurilemoma (schwannoma)
If not extremely well defined, consider:
organized inflammation
peripheral lung cancer 12
localized mesothelioma 12
solitary pleural metastasis
Also, consider the differential for a single pleural mass.







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.