Sturge-Weber syndrome
Updates to Article Attributes
Sturge-Weber syndrome (SWS),or encephalotrigeminal angiomatosis, is a phakomatosis characterized by facial port wine stains and pial angiomas.
Epidemiology
It is a rare syndrome, with an incidence estimated at 1 case in 20,000-50,000 persons 12.
Clinical presentation
The diagnosis is usually obvious on account of a congenital facial cutaneous haemangioma (also known as port wine stain or facial naevus flammeus). This feature is almost always present and usually involves the ophthalmic division (V1) of the trigeminal nerve 4, if it not involves this territory SWS is unlikely 11. Only rarely, in about 5%, it has intracranial involvement present without associated cutaneous naevus 1-2. In the majority of cases (72%) the naevus is unilateral and ipsilateral to the intracranial abnormality.
The most common clinical manifestation is with childhood seizures, present in 71-89% of cases 2, that are often refractory to medical therapy 1. These usually begin in the first few years of life and are often associated with developmental delay and hemispheric symptoms including hemiplegia / hemiparesis/hemiparesis and / or/or hemianopsia.
Approximately a third of patients have choroidal or scleral angiomatous involvement, which may be complicated with retinal detachment, buphthalmos or glaucoma 1.
Pathology
Unlike most phakomatoses, it is sporadic with no definite identifiable hereditary component 5,11.
The leptomeningeal haemangioma results in a vascular steal affecting the subjacent cortex and white matter producing localised ischaemia. In about 80% of the cases there is an unihemispherical involvement.
It is a type of craniofacial arteriovenous metameric syndrome (CAMS)
Associations
Radiographic features
Plain film
Skull x-rays were historically useful and capable of identifying the gyriform calcification of the subcortical white matter although they no longer play a significant role in the diagnosis or management of this condition. The finding usually becomes evident between 2 and 7 years of age 2.
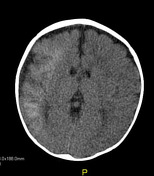
CT
- detects subcortical calcification at an earlier age than plain film and can also demonstrate associated parenchymal volume loss
- appearance liken to 'tram-track' in nature
- calvarial and regional sinus enlargement may be evident
- ipsilateral choroid plexus may be enlarged
- in severe cases a Dyke-Davidoff-Masson appearence may be seen
MRI
- T1: signal of affected region largely normal, with anatomic volume loss evident at older age
-
T1 C+ (Gd)
- prominent leptomeningeal enhancement in affected area
- much later in life the angioma may 'burn out' losing enhancement 1
- enlarged ipsilateral choroid plexus
-
T2: low signal in white matter subjacent to angioma representing
- postulated accelerated myelination in neonate 1
- calcification later in life
- abnormal deep venous drainage seen as flow voids
- GE/SWI/EPI: sensitive to calcification, seen as regions of signal drop out
- MR spectroscopy: decreased NAA 7
DSA: angiography
In most cases (82%) angiography is abnormal and demonstrates absent superficial cortical veins with abnormal and enlarged deep venous drainage 2.
Treatment and prognosis
Treatment revolves primarily around seizure control, with surgical resection only indicated rarely in refractory cases. Ophthalmological examination is also essential to identify and treat ocular involvement 4.
History and etymology
Sturge-Weber syndrome was first described by Sturge in 1879, followed by Weber and Volland in 1912 who described the intracranial calcification. Radiographic identification of cerebral calcification was first described by Dimitri in 1922 2-3.
- William Allen Sturge: English physician (1850-1919) 3
- Frederick Parkes Weber: English physician (1863-1962) 3
- Vincente Dimitri: Austrian dermatologist (1885-1955) 3
Differential diagnosis
The differential is a combination of that for multiple intracranial calcifications, cerebral hemiatrophy and leptomeningeal enhancement, and therefore includes:
- cerebral arteriovenous malformation (AVM)
- infection
- cutaneous haemangioma–vascular complex syndrome 8
- healed cortical infarct
- radiotherapy
-<p><strong>Sturge-Weber syndrome (SWS)</strong>,<strong> </strong>or <strong>encephalotrigeminal angiomatosis</strong>, is a <a href="/articles/phakomatosis">phakomatosis</a> characterized by facial port wine stains and pial angiomas.</p><h4>Epidemiology</h4><p>It is a rare syndrome, with an incidence estimated at 1 case in 20,000-50,000 persons <sup>12</sup>.</p><h4>Clinical presentation</h4><p>The diagnosis is usually obvious on account of a congenital facial cutaneous haemangioma (also known as <a href="/articles/port-wine-stain">port wine stain</a> or facial naevus flammeus). This feature is almost always present and usually involves the ophthalmic division (V1) of the <a href="/articles/trigeminal-nerve">trigeminal nerve</a> <sup>4</sup>, if it not involves this territory SWS is unlikely <sup>11</sup>. Only rarely, in about 5%, it has intracranial involvement present without associated cutaneous naevus <sup>1-2</sup>. In the majority of cases (72%) the naevus is unilateral and ipsilateral to the intracranial abnormality. </p><p>The most common clinical manifestation is with childhood seizures, present in 71-89% of cases <sup>2</sup>, that are often refractory to medical therapy <sup>1</sup>. These usually begin in the first few years of life and are often associated with developmental delay and hemispheric symptoms including hemiplegia / hemiparesis and / or hemianopsia.</p><p>Approximately a third of patients have choroidal or scleral angiomatous involvement, which may be complicated with retinal detachment, <a href="/articles/buphthalmos">buphthalmos</a> or glaucoma <sup>1</sup>.</p><h4>Pathology</h4><p>Unlike most phakomatoses, it is sporadic with no definite identifiable hereditary component <sup>5,11</sup>.</p><p>The leptomeningeal haemangioma results in a vascular steal affecting the subjacent cortex and white matter producing localised ischaemia. In about 80% of the cases there is an unihemispherical involvement.</p><p>It is a type of <a href="/articles/craniofacial-arteriovenous-metameric-syndrome">craniofacial arteriovenous metameric syndrome (CAMS)</a></p><h5>Associations</h5><ul>- +<p><strong>Sturge-Weber syndrome (SWS)</strong>,<strong> </strong>or <strong>encephalotrigeminal angiomatosis</strong>, is a <a href="/articles/phakomatosis">phakomatosis</a> characterized by facial port wine stains and pial angiomas.</p><h4>Epidemiology</h4><p>It is a rare syndrome, with an incidence estimated at 1 case in 20,000-50,000 persons <sup>12</sup>.</p><h4>Clinical presentation</h4><p>The diagnosis is usually obvious on account of a congenital facial cutaneous haemangioma (also known as <a href="/articles/port-wine-stain">port wine stain</a> or facial naevus flammeus). This feature is almost always present and usually involves the ophthalmic division (V1) of the <a href="/articles/trigeminal-nerve">trigeminal nerve</a> <sup>4</sup>, if it not involves this territory SWS is unlikely <sup>11</sup>. Only rarely, in about 5%, it has intracranial involvement present without associated cutaneous naevus <sup>1-2</sup>. In the majority of cases (72%) the naevus is unilateral and ipsilateral to the intracranial abnormality. </p><p>The most common clinical manifestation is with childhood seizures, present in 71-89% of cases <sup>2</sup>, that are often refractory to medical therapy <sup>1</sup>. These usually begin in the first few years of life and are often associated with developmental delay and hemispheric symptoms including hemiplegia/hemiparesis and/or hemianopsia.</p><p>Approximately a third of patients have choroidal or scleral angiomatous involvement, which may be complicated with retinal detachment, <a href="/articles/buphthalmos">buphthalmos</a> or glaucoma <sup>1</sup>.</p><h4>Pathology</h4><p>Unlike most phakomatoses, it is sporadic with no definite identifiable hereditary component <sup>5,11</sup>.</p><p>The leptomeningeal haemangioma results in a vascular steal affecting the subjacent cortex and white matter producing localised ischaemia. In about 80% of the cases there is an unihemispherical involvement.</p><p>It is a type of <a href="/articles/craniofacial-arteriovenous-metameric-syndrome">craniofacial arteriovenous metameric syndrome (CAMS)</a></p><h5>Associations</h5><ul>
Image 8 CT (non-contrast) ( create )







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.