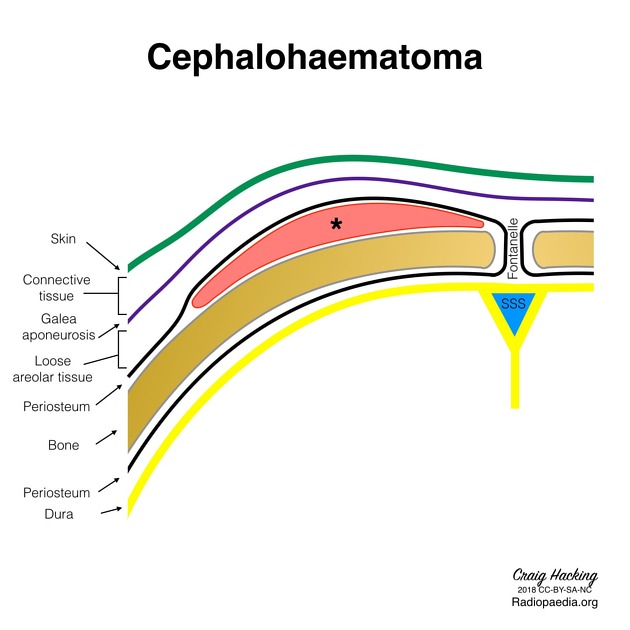
Subgaleal hematoma describes scalp bleeding in the potential space between the periosteum and the galeal aponeurosis. It is a rare but possibly lethal emergency.
On this page:
Epidemiology
Moderate to severe presentations occur in 1.5 of 10,000 live births. It most commonly occurs after vacuum-assisted and forceps delivery, but may also be seen following head trauma or occur spontaneously. The association with vacuum extraction is as high as 89% of cases 4. In patients with intracranial hemorrhage or skull fractures, the incidence of subgaleal hemorrhage is increased 4.
Clinical presentation
Signs include pallor on inspection. On examination, there may be tachycardia and/or hypotonia. A fluctuant scalp mass with increasing head circumference may be seen on palpation.
As the potential space extends into the neck, a subgaleal hematoma may also extend into the neck. This is in contrast to a cephalohematoma which remains confined to the skull and will not cross suture lines 4.
Pathology
Etiology
Bleeding occurs as a result of rupture to emissary veins which drain the scalp veins into the dural sinuses.
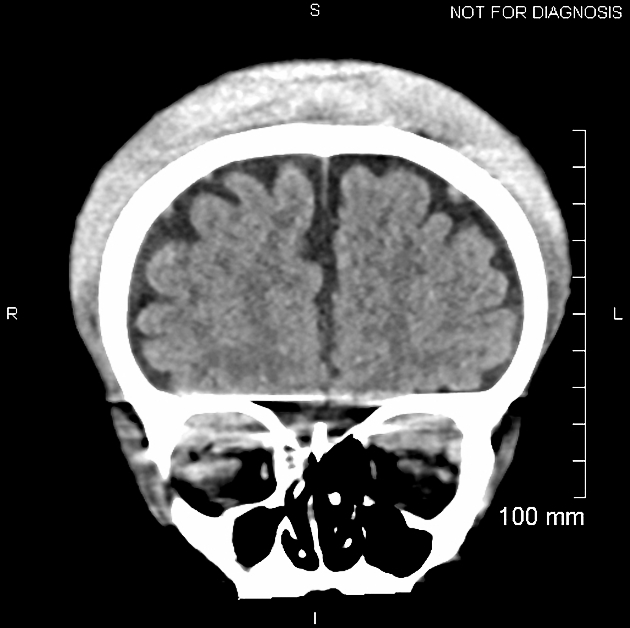
Location
Due to being superficial to the periosteum, subgaleal hematomas are able to cross suture lines and surround the entire skull.
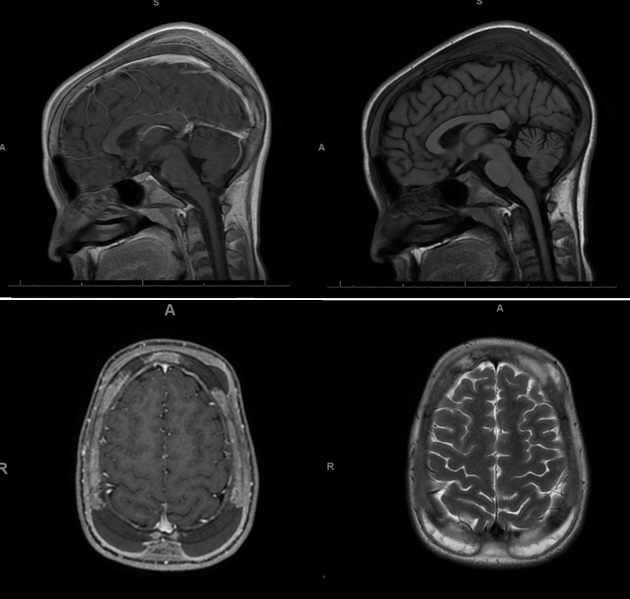
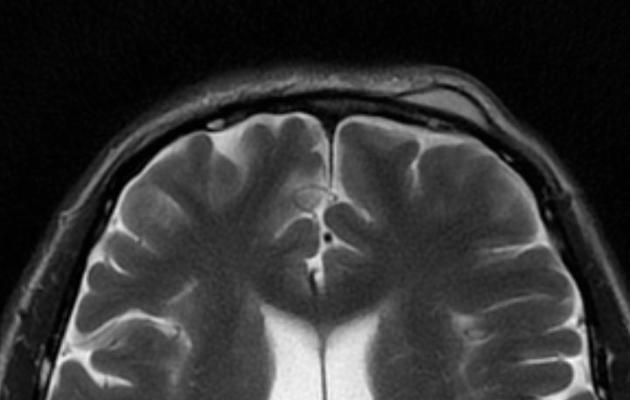
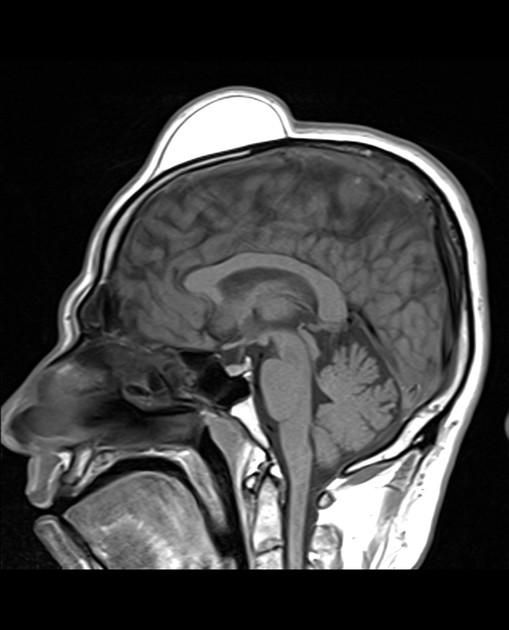
Radiographic features
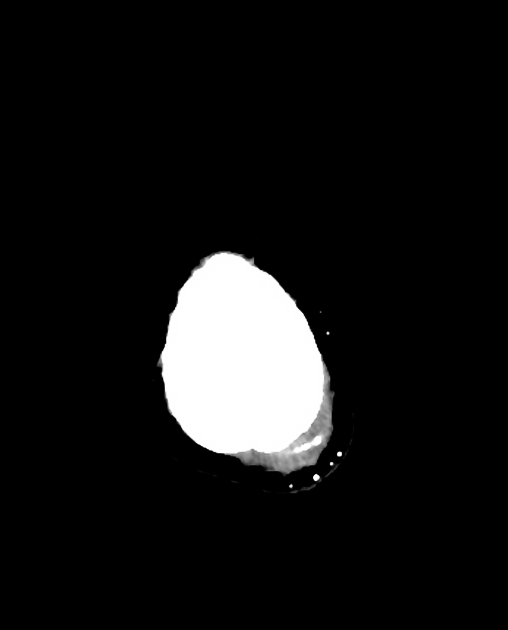
Ultrasound
- blood of moderate echogenicity
- decreasing echogenicity with time
- not bound by periosteum
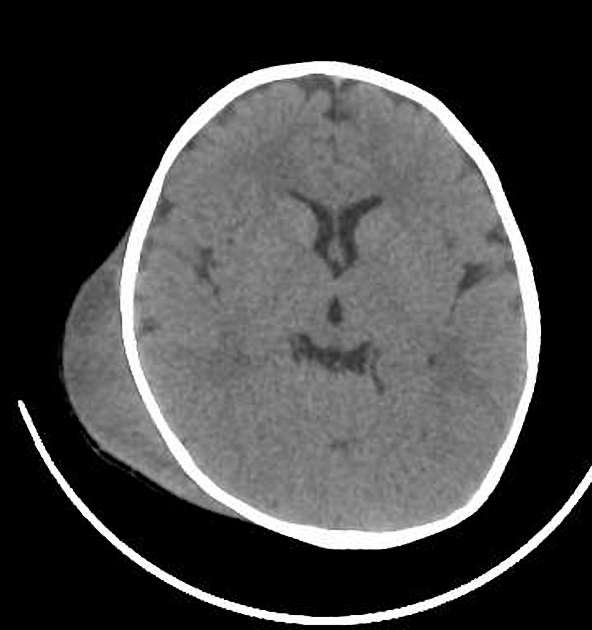
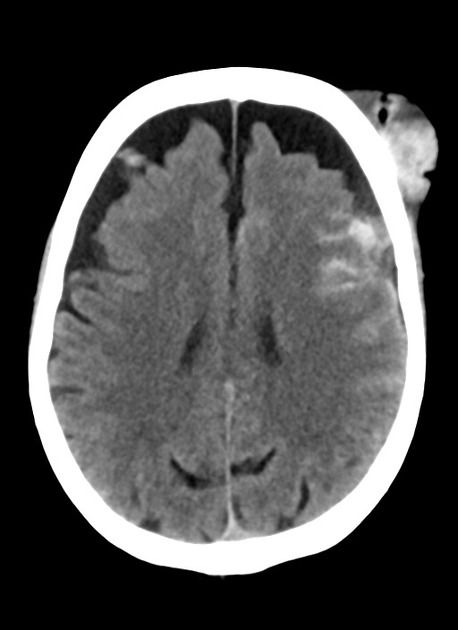
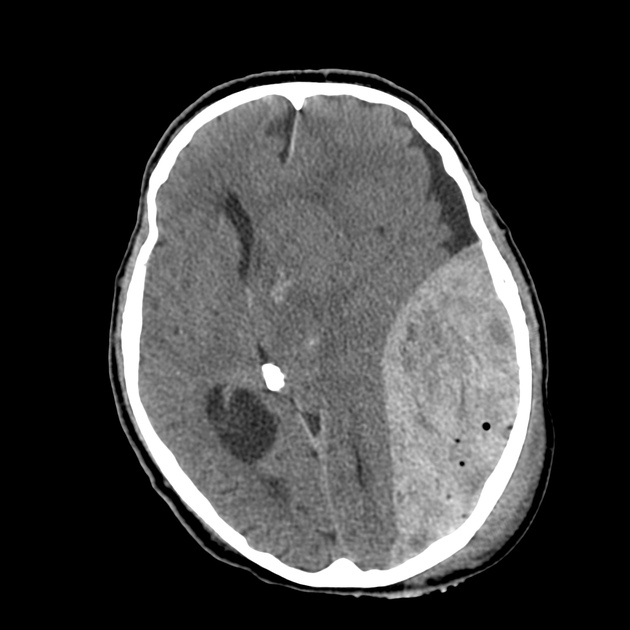
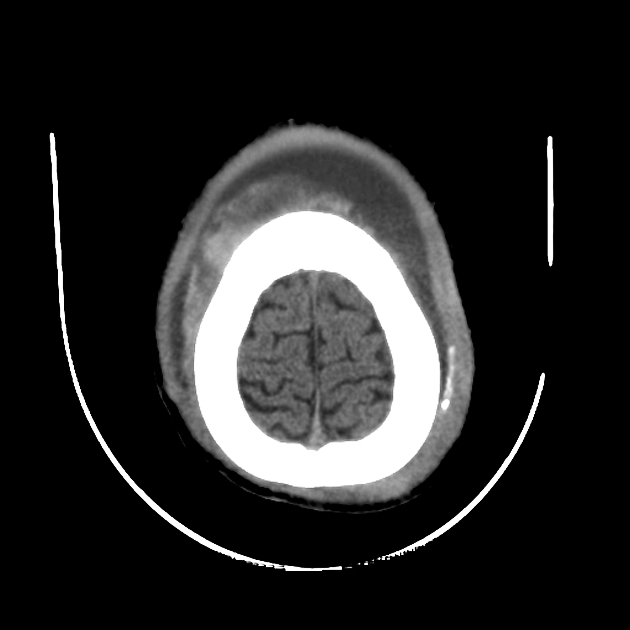
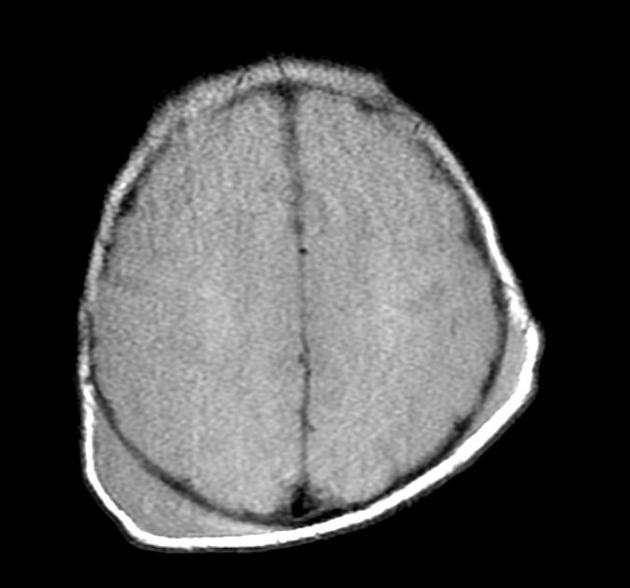
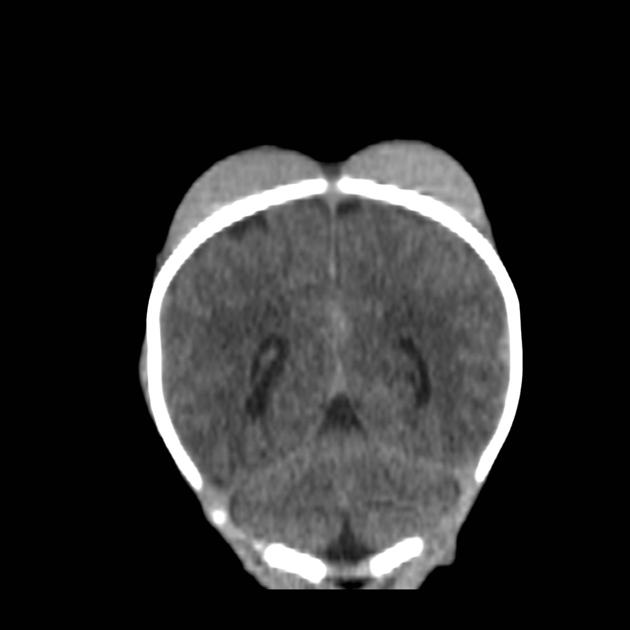
CT
- more objective measurement of hematoma volume
- enables to determine presence of an underlying skull fracture
Radiology report
- size of the hematoma
- content of the fluid collection
- presence of an associated fracture
Differential diagnosis
General imaging differential considerations include:
On certain MRI sequences also consider:



















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.