Contrast media extravasation refers to the leakage of intravenously administered contrast media from the normal intravascular compartment into surrounding soft tissues.
It is a known complication of contrast-enhanced CT. It can also occur in MRI, but the complications are rare given the low volumes and injection rates that are used.
Occasionally extravasation also happens in fluoroscopy, but due to the combination of a slow manual injection, small boluses and the visualization in real-time of the contrast passing into the blood vessel, it is rarely an issue.
On this page:
Terminology
Strictly speaking, 'extravasation' should be used for leakage of contrast from blood vessels only. However, it is widely used in a more general sense when contrast escapes from any normal anatomical structure into the surrounding soft tissues, e.g. leak of contrast medium from the renal tract after iatrogenic ureteric injury.
Epidemiology
CT contrast media extravasation occurs relatively infrequently, in ~0.5% (range 0.13-0.68%) of cases, but can have severe side effects associated with skin changes and possible skin necrosis 7.
Risk factors
-
increased incidence with automated power injection because large volumes can extravasate in a short period of time 2,3
with manual injection, extravasation is thought less likely, as there is direct supervision of contrast administration
-
patient-related factors
-
the site of venous access
higher percentage of leakage from venous access in the back of the hand, wrist, foot and ankle
likely related to a smaller amount of subcutaneous tissue and the fact that veins are more fragile in these regions
the gauge of intravenous catheter: only if smaller caliber access (over 22G) is used; risk of leakage is the same for 18G and 20G 1
-
high-osmolar contrast medium 2
prewarming of high-osmolar (370 mg/mL) contrast to 37°C lowers the viscosity and has been proven to lower the probability of extravasation 5
patients undergoing CT are at higher risk of developing extravasation than MRI patients 3
-
at MRI, contrast media extravasation is more likely in patients 3:
older than 60 years
using automated power injections
Clinical presentation
Contrast media extravasation is usually recognized at the time it happens.
Patients complain of local symptoms at, and close to, the site of injection:
pain and tenderness
swelling
itching
tightness of the skin
redness
Pathology
Non-ionic low-osmolar contrast media are known to reduce the risk of severe soft tissue injury, but the potential for soft tissue injury is often related to the volume of contrast media that extravasates 1.
Treatment and prognosis
The conduct after an episode of contrast media extravasation will vary according to the protocol of each radiology department and might include:
discontinue the contrast infusion and notify the radiologist immediately
attempted aspiration of the extravasation is not effective
apply an ice pack to the affected area and elevate the affected extremity to reduce swelling
keep the patient under observation for at least two hours
at some institutions, the policy is to require plastic surgery consultation for all patients whose extravasations involve 100 mL or more of contrast medium
make contact with the doctor requesting the examination
it is suggested to follow up with the patient in the next few days until the resolution of local edema; this can be accomplished with a phone call to evaluate the regression of the signs and symptoms
-
instruct the patient to notify staff if there is:
increasing swelling or pain over time
blistering, ulceration, induration or other skin changes
altered tissue perfusion and/or changes in sensation
Complications
Most contrast media extravasation results in minimal swelling or erythema and is not associated with any long-term sequelae 2. A large study found that >97% of patients with contrast extravasation had minimal or no injury and reported that 79% of patients had localized swelling after extravasation, 24% had pain, and 8% were asymptomatic 4.
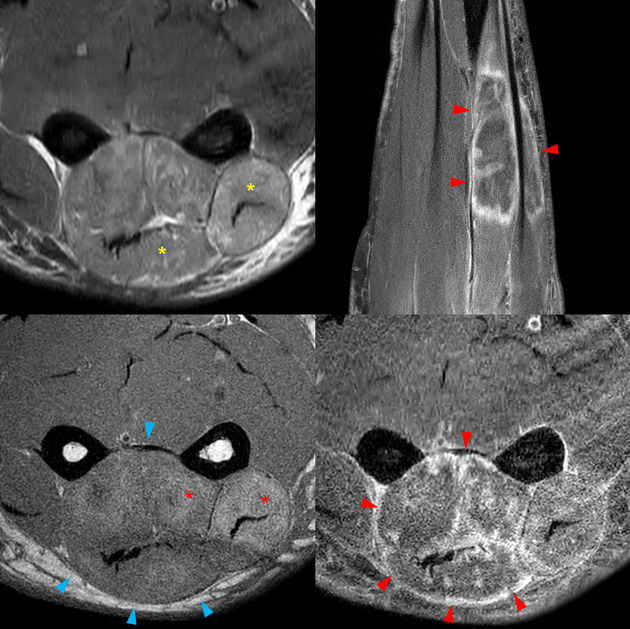
Large volumes (>50 mL) of high-osmolar contrast media are known to induce significant tissue damage although this is rare 6:
skin ulceration
soft tissue necrosis













 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.