Langerhans cell histiocytosis (LCH) is a rare multisystem disease with a wide and heterogeneous clinical spectrum and variable extent of involvement.
On this page:
Terminology
Langerhans cell histiocytosis was previously known as histiocytosis X. The newer term is preferred as it is more descriptive of its cellular background, and removes the ambiguity of the connotation "X".
Historically, the condition was also subdivided into three distinct entities, Letterer-Siwe disease, Hand-Schüller-Christian disease and eosinophilic granuloma, see below.
Epidemiology
The disease is more common in the pediatric population, with a peak incidence between one and three years of age 5. Incidence is estimated at ~5 per million children, and 1-2 cases per million adults 8. There is also a male predilection (M:F ~1.5:1) 5.
Clinical presentation
Essentially any part of the body can be affected and as such, clinical presentation will depend on specific involvement. The course of the disease ranges from those that spontaneously regress to those that have a rapidly progressive course (the latter is especially common in young children with multisystem disease).
Historically, three forms (two with eponymous names) have been recognized, although there is some confusion as to their definition 1-5:
-
disseminated multiorgan disease
typically young children/infants less than one year old
fulminant course with poor prognosis
-
Hand-Schüller-Christian disease
-
multiple lesions
some authors confine the term to patients with solitary organ involvement 4
other authors accept multiorgan involvement (e.g. bone and spleen) 6
confined to the one location (usually bone)
typically children
intermediate prognosis
-
-
-
lesions are confined to one organ system
some authors confine the term to patients with a solitary lesion 4
other authors accept multiple lesions 6
70% of cases affect bone
typically children
best prognosis
-
A more useful and less controversial classification, which roughly correlates to the eponymous diseases above, is as follows:
multiple organ systems, multiple sites involved
single organ system, multiple sites involved
single lesion
Additionally, in 2008 the WHO recommended distinguishing Langerhans cell histiocytosis from a more pleomorphic variant known as Langerhans cell sarcoma 3.
As well as systemic disease, individual organ systems may be involved, which will be discussed separately:
The remainder of this article concerns a general overview of Langerhans cell histiocytosis.
Pathology
Langerhans cell histiocytosis is due to uncontrolled monoclonal proliferation of Langerhans cells (distinctive cells of monocyte-macrophage lineage) and should be considered a malignancy although its biological behavior is very variable 1,3. An immune-mediated mechanism has been postulated. This proliferation is accompanied by inflammation and granuloma formation. Electron microscopy may reveal characteristic Birbeck granules. Immunohistochemistry reveals expression of the following antigens:
HLA-DR
CD1a
CD207 (langerin)
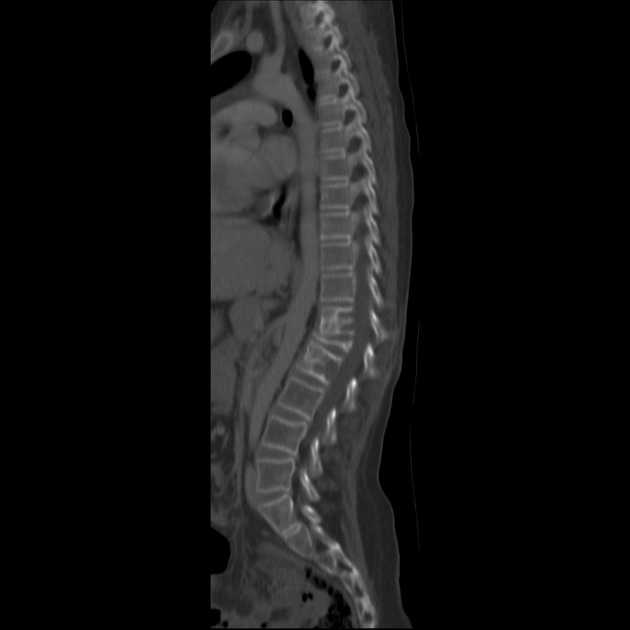
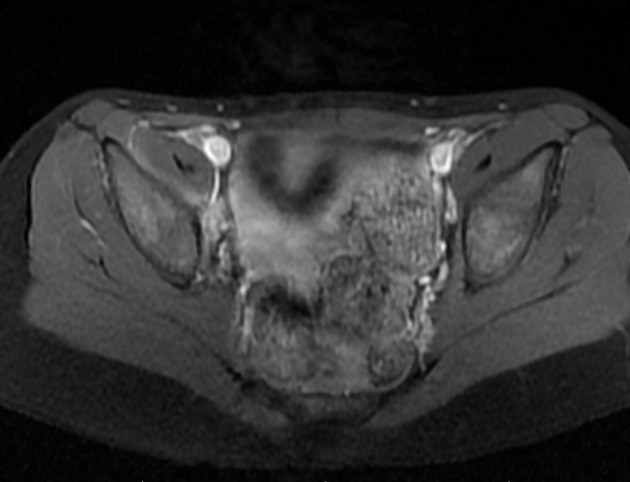
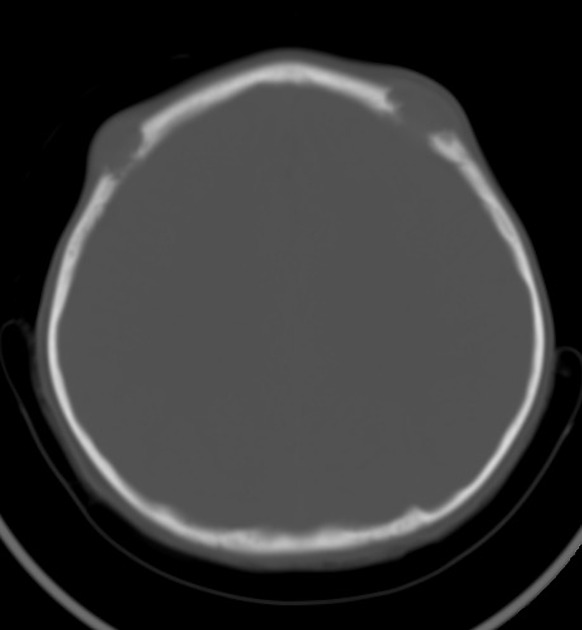
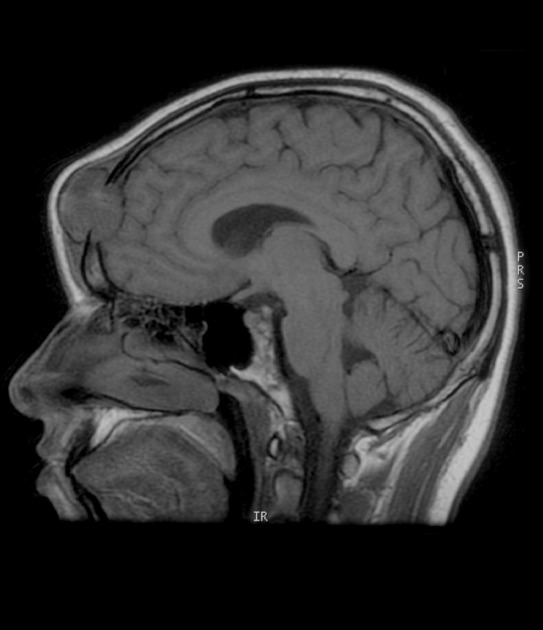
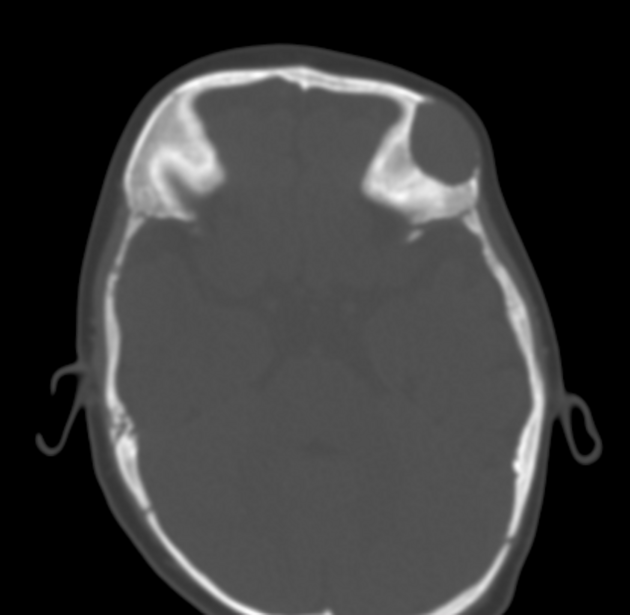
Radiographic features
Imaging features are often not pathognomonic and tissue diagnosis is usually required for definitive diagnosis. As Langerhans cell histiocytosis can affect most organ systems, radiographic appearances are discussed separately (see above).
Treatment and prognosis
The prognosis can be extremely variable with eosinophilic granuloma limited to bone carrying the best and Letterer-Siwe disease carrying the worst prognosis, respectively. The prognosis is more closely related to the disease burden rather than histological features, although frankly malignant features (Langerhans cell sarcoma) do also have an impact on survival 3,4:
unifocal disease (eosinophilic granuloma): >95% survival
two organ involvement: 75% survival
Langerhans cell sarcoma: 50% survival
History and etymology
The Langerhans cell was discovered within the epidermis by German physician Paul Langerhans (1847-1888) in 1865 when he was a medical student and working under the famed Professor Rudolf Virchow (1821-1902) 9,10.
See also
Erdheim-Chester Disease: a non-Langerhans cell histiocytosis
Rosai-Dorfman disease: sinus histiocytosis











 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.