Congestive cardiac failure
Updates to Synonym Attributes
Updates to Article Attributes
Congestive cardiac failure (CCF), also known as congestive heart failure (CHF), refers to the clinical syndrome caused by inherited or acquired abnormalities of heart structure and function, causing a constellation of symptoms and signs that lead to decreased quality and quantity of life.
Epidemiology
CCF is common, affecting 2% of all adults in developed nations, and up to 10% of adults over 65 years old 1. The condition is thought to affect up to 20 million people worldwide 1.
Clinical presentation
Clinical presentation varies considerably depending on the severity and aetiology of CCF 1,2. Traditionally, symptoms can be clustered into either being attributed to left ventricular dysfunction or right ventricular dysfunction, although in reality, most patients will have manifestations from both clusters 1,2.
- left-predominant symptoms and signs
- exertional dyspnoea and fatigue 1,2
- orthopnoea: dyspnoea in the recumbent position, may use multiple pillows at night 1,2
- paroxysmal nocturnal dyspnoea: dyspnoea that awakens the patient from sleep, usually only after 1-2 hours, and may have a chronic nocturnal cough and cardiac asthma 1,2
- bendopnoea: dyspnoea while bending forward 3
- angina 1,2
- syncope and cerebral dysfunction 1,2
- cyanosis 1,2
- other organ dysfunction 1,2
- added heart sounds 1,2
- S3 ‘ventricular gallop’ (occurs after S2 and is due to blood slushing around in a large dilated ventricle) 1,2
- S4 ‘atrial gallop’ (occurs before S1 and is due to blood entering the ventricle during atrial systole hitting the stiff hypertrophied ventricular wall 1,2
- pulsus alternans 1,2
- exertional dyspnoea and fatigue 1,2
- right-predominant symptoms and signs
- nocturia 1,2
- sacral and scrotal oedema, especially if bed bound 1,2
- peripheral (ankle) oedema 1,2
- ascites 1,2
- hepatomegaly, may have a tender edge and gastrointestinal symptoms 1,2
- raised
JVPjugular venous pressure 1,2
The severity of clinical presentation is classified according to the New York Heart Association, which is graded according to how much physical activity is decreased 1,2. Patients with severe CCF may have limitations in performing activities of daily living, Cheyne-Stokes respiration, hypotension, tachycardia, features of valvulopathies, and cardiac cachexia 1,2.
Depending on the underlying aetiology, additional clinical features may also be present 1,2.
Pathology
It may be precipitated by intrinsic cardiac or extrinsic factors. It may also be acute (acute decompensated cardiac failure) or chronic (chronic congestive cardiac failure) 1,2. Up to 40-50% of patients have diastolic heart failure with preserved left ventricular function 4.
Classification and aetiology
There are numerous ways of classifying CCF, the most commonly utilised being a functional classification that is based on cardiac output and ejection fraction 1,2. In this classification, there are often overlapping aetiologies and patients can move from one classification to the other over time 1,2.
- low-output heart failure
- heart failure with reduced ejection failure (HFrEF), previously termed 'systolic heart failure'
- ischaemic dilated cardiomyopathy 1,2
- non-ishcaemic dilated cardiomyopathy (e.g. idiopathic, alcoholism, tachycardia-mediated cardiomyopathy, Chagas disease, Duchenne muscular dystrophy, hypothyroidism, cocaine use, infection, etc.) 1,2
- chronic hypertension 1,2
- obstructive valve disease (e.g. in the setting of aortic valve stenosis) 1,2
- regurgitant valve disease (e.g. in the setting of aortic valve regurgitation) 1,2
- left-to-right shunts (e.g. atrial septal defect, ventricular septal defect, patent ductus arteriosus, Gerbode defect, atrioventricular septal defect, etc.) 1,2
- heart failure with preserved ejection praction (HPpEF), previously termed 'diastolic heart failure'
- hypertrophic cardiomyopathy (e.g. hypertrophic obstructive cardiomyopathy, Yamaguchi syndrome, chronic hypertension, obstructive valve disease, left-to-right shunts, athlete's heart, etc.) 1,2
- restrictive cardiomyopathy (e.g. cardiac amyloidosis, cardiac sarcoidosis, endomyocardial fibrosis, haemochromatosis, etc.) 1,2
- constrictive pericarditis 1,2
- heart failure with reduced ejection failure (HFrEF), previously termed 'systolic heart failure'
-
high-output heart failure
- morbid obesity 1,2
- systemic arteriovenous shunts (e.g. hereditary haemorrhagic telangiectasia, hepatopulmonary syndrome, haemodialysis fistula) 1,2
- chronic lung disease 1,2
- sepsis 1,2
- myeloproliferative neoplasm 1,2
- anaemia 1,2
- hyperthyroidism 1,2
- wet beriberi 1,2
- carcinoid syndrome 1,2
Radiographic features
Plain radiograph
The accuracy of interpreting chest radiographs regarding congestive cardiac failure was only around 70% according to one study 5.
With left-sided congestive cardiac failure, the features are that of pulmonary oedema which includes 1,2,4-8:
- central pulmonary venous congestion
- cephalisation of pulmonary veins
- pulmonary interstitial oedema
- pulmonary alveolar oedema
- cardiomegaly (may or may not be present depending on aetiology)
Ultrasound: echocardiography
Echocardiography is the most common imaging modality used to evaluate patients with CCF 1,2. It is able to provide a semi-quantitative assessment of left ventricular size and function, and determine the presence of valvular or wall abnormalities 1,2.
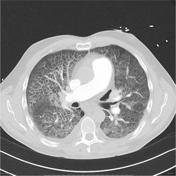
CT
CT chest may demonstrate the same features as the plain radiograph, but in greater detail and clarity 6,7,9. Furthermore, electrocardiograph-gated CT and cardiac CT angiography may provide estimates of cardiac function and detailed visualisation of various cardiac structures 9.
MRI
Cardiac MRI (CMR) is able to provide highly accurate ejection fraction estimates and determine presence of any structural abnormalities, and is considered by many to be the gold standard imaging modality 2,9,10-11. Patterns of late gadolinium enhancement can distinguish between many aetiologies of CCF, although this is beyond the scope of this general article on CCF 9,1010,11.
Treatment and prognosis
Treatment involves a multidisciplinary team and incorporates lifestyle, allied health, pharmacological, and even surgical therapies, often specific to the underlying aetiology 1,2. An in-depth review of the treatment of CCF is beyond the scope of this article, however general principles include:
- treatment of comorbidities and complications (e.g. obesity, hypertension, depression, etc.) 1,2
- lifestyle interventions: education, cessation of smoking and alcohol consumption, increase in isotonic exercise, improve diet, daily home weights 1,2
- pharmacotherapy:
- mortality benefit: angiotensin-converting-enzyme inhibitors, angiotensin II receptor blockers, combination angiotensin receptor-neprilysin inhibitors, beta-blockers (only carvedilol, bisoprolol, metoprolol succinate, nebivolol), spironolactone 1,2
,11,12- these medications only have a benefit in patients with HFrEF, there are no medications with a mortality benefit in HFpEF (as of December 2017) 1,2
- symptomatic benefit with no mortality benefit: other diuretics, nitrates, digoxin, hydralazine 1,2
- mortality benefit: angiotensin-converting-enzyme inhibitors, angiotensin II receptor blockers, combination angiotensin receptor-neprilysin inhibitors, beta-blockers (only carvedilol, bisoprolol, metoprolol succinate, nebivolol), spironolactone 1,2
- surgery: considering implantable cardioverter-defibrillators,
pacemakerscardiac resynchronisation therapy, ventricular assist devices, and even cardiac transplant, depending on severity and aetiology 1,2
Despite advances in management in recent decades, prognosis remains poor with 30-40% of patients dying within 1 year, and up to 70% dying within 5 years 1.
Complications
- acute decompensated heart failure and acute pulmonary oedema
See also
-<p><strong>Congestive cardiac failure (CCF)</strong> refers to the clinical syndrome caused by inherited or acquired abnormalities of heart structure and function, causing a constellation of symptoms and signs that lead to decreased quality and quantity of life.</p><h4>Epidemiology</h4><p>CCF is common, affecting 2% of all adults in developed nations, and up to 10% of adults over 65 years old <sup>1</sup>. The condition is thought to affect up to 20 million people worldwide <sup>1</sup>.</p><h4>Clinical presentation</h4><p>Clinical presentation varies considerably depending on the severity and aetiology of CCF <sup>1,2</sup>. Traditionally, symptoms can be clustered into either being attributed to left ventricular dysfunction or right ventricular dysfunction, although in reality, most patients will have manifestations from both clusters <sup>1,2</sup>.</p><ul>- +<p><strong>Congestive cardiac failure (CCF)</strong>, also known as <strong>congestive heart failure (CHF)</strong>, refers to the clinical syndrome caused by inherited or acquired abnormalities of heart structure and function, causing a constellation of symptoms and signs that lead to decreased quality and quantity of life.</p><h4>Epidemiology</h4><p>CCF is common, affecting 2% of all adults in developed nations, and up to 10% of adults over 65 years old <sup>1</sup>. The condition is thought to affect up to 20 million people worldwide <sup>1</sup>.</p><h4>Clinical presentation</h4><p>Clinical presentation varies considerably depending on the severity and aetiology of CCF <sup>1,2</sup>. Traditionally, symptoms can be clustered into either being attributed to left ventricular dysfunction or right ventricular dysfunction, although in reality, most patients will have manifestations from both clusters <sup>1,2</sup>.</p><ul>
- +<li>cyanosis <sup>1,2</sup>
- +</li>
-<li>ascites <sup>1,2</sup>- +<li>
- +<a href="/articles/ascites">ascites</a> <sup>1,2</sup>
-<li>hepatomegaly, may have a tender edge and gastrointestinal symptoms <sup>1,2</sup>- +<li>
- +<a href="/articles/hepatomegaly">hepatomegaly</a>, may have a tender edge and gastrointestinal symptoms <sup>1,2</sup>
-<li>raised JVP <sup>1,2</sup>- +<li>raised jugular venous pressure <sup>1,2</sup>
-</ul><p>Patients with severe CCF may have limitations in performing activities of daily living, Cheyne-Stokes respiration, and cardiac cachexia <sup>1,2</sup>. Depending on the underlying aetiology, additional clinical features may also be present <sup>1,2</sup>. </p><h4>Pathology</h4><p>It may be precipitated by intrinsic cardiac or extrinsic factors. It may also be acute (acute decompensated cardiac failure) or chronic (chronic congestive cardiac failure) <sup>1,2</sup>. Up to 40-50% of patients have diastolic heart failure with preserved left ventricular function<sup> <span style="font-size:10.8333px">4</span></sup>. </p><h5>Classification and aetiology</h5><p>There are numerous ways of classifying CCF, the most commonly utilised being a functional classification that is based on cardiac output and ejection fraction <sup>1,2</sup>. In this classification, there are often overlapping aetiologies and patients can move from one classification to the other over time <sup>1,2</sup>.</p><ul>- +</ul><p>The severity of clinical presentation is classified according to the New York Heart Association, which is graded according to how much physical activity is decreased <sup>1,2</sup>. Patients with severe CCF may have limitations in performing activities of daily living, Cheyne-Stokes respiration, hypotension, tachycardia, features of valvulopathies, and cardiac cachexia <sup>1,2</sup>. </p><p>Depending on the underlying aetiology, additional clinical features may also be present <sup>1,2</sup>. </p><h4>Pathology</h4><p>It may be precipitated by intrinsic cardiac or extrinsic factors. It may also be acute (acute decompensated cardiac failure) or chronic (chronic congestive cardiac failure) <sup>1,2</sup>. Up to 40-50% of patients have diastolic heart failure with preserved left ventricular function<sup> 4</sup>. </p><h5>Classification and aetiology</h5><p>There are numerous ways of classifying CCF, the most commonly utilised being a functional classification that is based on cardiac output and ejection fraction <sup>1,2</sup>. In this classification, there are often overlapping aetiologies and patients can move from one classification to the other over time <sup>1,2</sup>.</p><ul>
-<li>ischaemic <a title="Dilated cardiomyopathy" href="/articles/dilated-cardiomyopathy">dilated cardiomyopathy</a> <sup>1,2</sup>- +<li>ischaemic <a href="/articles/dilated-cardiomyopathy">dilated cardiomyopathy</a> <sup>1,2</sup>
-<li>non-ishcaemic <a title="Dilated cardiomyopathy" href="/articles/dilated-cardiomyopathy">dilated cardiomyopathy</a> (e.g. <a title="Idiopathic dilated cardiomyopathy" href="/articles/idiopathic-dilated-cardiomyopathy">idiopathic</a>, alcoholism, <a title="Tachycardia induced cardiomyopathy" href="/articles/tachycardia-induced-cardiomyopathy">tachycardia-mediated cardiomyopathy</a>, <a title="Chagas disease" href="/articles/chagas-disease">Chagas disease</a>, <a title="Duchenne muscular dystrophy" href="/articles/duchenne-muscular-dystrophy">Duchenne muscular dystrophy</a>, <a title="hypothyroidism" href="/articles/hypothyroidism">hypothyroidism</a>, cocaine use, infection, etc.) <sup>1,2</sup>- +<li>non-ishcaemic <a href="/articles/dilated-cardiomyopathy">dilated cardiomyopathy</a> (e.g. <a href="/articles/idiopathic-dilated-cardiomyopathy">idiopathic</a>, alcoholism, <a href="/articles/tachycardia-induced-cardiomyopathy">tachycardia-mediated cardiomyopathy</a>, <a href="/articles/chagas-disease">Chagas disease</a>, <a href="/articles/duchenne-muscular-dystrophy">Duchenne muscular dystrophy</a>, <a href="/articles/hypothyroidism">hypothyroidism</a>, cocaine use, infection, etc.) <sup>1,2</sup>
-<li>chronic <a title="Hypertension" href="/articles/hypertension">hypertension</a> <sup>1,2</sup>- +<li>chronic <a href="/articles/hypertension">hypertension</a> <sup>1,2</sup>
-<li>obstructive valve disease (e.g. in the setting of <a title="Aortic valve stenosis" href="/articles/aortic-valve-stenosis">aortic valve stenosis</a>) <sup>1,2</sup>- +<li>obstructive valve disease (e.g. in the setting of <a href="/articles/aortic-valve-stenosis">aortic valve stenosis</a>) <sup>1,2</sup>
-<li>regurgitant valve disease (e.g. in the setting of <a title="aortic valve regurgitation" href="/articles/aortic-valve-regurgitation">aortic valve regurgitation</a>) <sup>1,2</sup>- +<li>regurgitant valve disease (e.g. in the setting of <a href="/articles/aortic-valve-regurgitation">aortic valve regurgitation</a>) <sup>1,2</sup>
-<li>left-to-right shunts (e.g. <a title="Atrial septal defect" href="/articles/atrial-septal-defect-2">atrial septal defect</a>, <a title="Ventricular septal defect" href="/articles/ventricular-septal-defect-1">ventricular septal defect</a>, <a title="Patent ductus arteriosus" href="/articles/patent-ductus-arteriosus">patent ductus arteriosus</a>, <a title="Gerbode defect" href="/articles/gerbode-defect">Gerbode defect</a>, <a title="Atrioventricular septal defect" href="/articles/atrioventricular-septal-defect">atrioventricular septal defect</a>, etc.) <sup>1,2</sup>- +<li>left-to-right shunts (e.g. <a href="/articles/atrial-septal-defect-2">atrial septal defect</a>, <a href="/articles/ventricular-septal-defect-1">ventricular septal defect</a>, <a href="/articles/patent-ductus-arteriosus">patent ductus arteriosus</a>, <a href="/articles/gerbode-defect">Gerbode defect</a>, <a href="/articles/atrioventricular-septal-defect">atrioventricular septal defect</a>, etc.) <sup>1,2</sup>
-<a title="Hypertrophic cardiomyopathy" href="/articles/hypertrophic-cardiomyopathy">hypertrophic cardiomyopathy</a> (e.g. <a title="Hypertrophic obstructive cardiomyopathy (HOCM)" href="/articles/hypertrophic-cardiomyopathy">hypertrophic obstructive cardiomyopathy</a>, <a title="Yamaguchi syndrome" href="/articles/apical-hypertrophic-cardiomyopathy">Yamaguchi syndrome</a>, chronic <a title="Hypertension" href="/articles/hypertension">hypertension</a>, obstructive valve disease, left-to-right shunts, <a title="athlete's heart" href="/articles/athlete-s-heart">athlete's heart</a>, etc.) <sup>1,2</sup>- +<a href="/articles/hypertrophic-cardiomyopathy">hypertrophic cardiomyopathy</a> (e.g. <a href="/articles/hypertrophic-cardiomyopathy">hypertrophic obstructive cardiomyopathy</a>, <a href="/articles/apical-hypertrophic-cardiomyopathy">Yamaguchi syndrome</a>, chronic <a href="/articles/hypertension">hypertension</a>, obstructive valve disease, left-to-right shunts, <a href="/articles/athlete-s-heart">athlete's heart</a>, etc.) <sup>1,2</sup>
-<li>restrictive cardiomyopathy (e.g. <a title="Cardiac amyloidosis" href="/articles/cardiac-amyloidosis">cardiac amyloidosis</a>, <a title="Cardiac sarcoidosis" href="/articles/sarcoidosis-cardiac-manifestations-1">cardiac sarcoidosis</a>, <a title="Endomyocardial fibrosis" href="/articles/endomyocardial-fibrosis">endomyocardial fibrosis</a>, <a title="Haemochromatosis (cardiac manifestations)" href="/articles/haemochromatosis-cardiac-manifestations-1">haemochromatosis</a>, etc.) <sup>1,2</sup>- +<li>restrictive cardiomyopathy (e.g. <a href="/articles/cardiac-amyloidosis">cardiac amyloidosis</a>, <a href="/articles/sarcoidosis-cardiac-manifestations-1">cardiac sarcoidosis</a>, <a href="/articles/endomyocardial-fibrosis">endomyocardial fibrosis</a>, <a href="/articles/haemochromatosis-cardiac-manifestations-1">haemochromatosis</a>, etc.) <sup>1,2</sup>
-<a title="Constrictive pericarditis" href="/articles/constrictive-pericarditis">constrictive pericarditis</a> <sup>1,2</sup>- +<a href="/articles/constrictive-pericarditis">constrictive pericarditis</a> <sup>1,2</sup>
-<a title="High output heart failure" href="/articles/high-output-cardiac-failure">high-output heart failure</a><ul>-<li>morbid <a title="Obesity" href="/articles/obesity">obesity</a> <sup>1,2</sup>- +<a href="/articles/high-output-cardiac-failure">high-output heart failure</a><ul>
- +<li>morbid <a href="/articles/obesity">obesity</a> <sup>1,2</sup>
-<li>systemic arteriovenous shunts (e.g. <a title="Hereditary haemorrhagic telangiectasia" href="/articles/hereditary-haemorrhagic-telangiectasia">hereditary haemorrhagic telangiectasia</a>, <a title="Hepatopulmonary syndrome" href="/articles/hepatopulmonary-syndrome">hepatopulmonary syndrome</a>, <a title="Haemodialysis fistula" href="/articles/haemodialysis-arteriovenous-fistula">haemodialysis fistula</a>) <sup>1,2</sup>- +<li>systemic arteriovenous shunts (e.g. <a href="/articles/hereditary-haemorrhagic-telangiectasia">hereditary haemorrhagic telangiectasia</a>, <a href="/articles/hepatopulmonary-syndrome">hepatopulmonary syndrome</a>, <a href="/articles/haemodialysis-arteriovenous-fistula">haemodialysis fistula</a>) <sup>1,2</sup>
-<a title="sepsis" href="/articles/sepsis">sepsis</a> <sup>1,2</sup>- +<a href="/articles/sepsis">sepsis</a> <sup>1,2</sup>
-<a title="Myeloproliferative neoplasm" href="/articles/myeloproliferative-disorder">myeloproliferative neoplasm</a> <sup>1,2</sup>- +<a href="/articles/myeloproliferative-disorder">myeloproliferative neoplasm</a> <sup>1,2</sup>
-<a title="anaemia" href="/articles/anaemia">anaemia</a> <sup>1,2</sup>- +<a href="/articles/anaemia">anaemia</a> <sup>1,2</sup>
-<a title="hyperthyroidism" href="/articles/hyperthyroidism">hyperthyroidism</a> <sup>1,2</sup>- +<a href="/articles/hyperthyroidism">hyperthyroidism</a> <sup>1,2</sup>
-<li>wet <a title="beriberi" href="/articles/beriberi">beriberi</a> <sup>1,2</sup>- +<li>wet <a href="/articles/beriberi">beriberi</a> <sup>1,2</sup>
-<a title="Carcinoid syndrome" href="/articles/carcinoid-syndrome">carcinoid syndrome</a> <sup>1,2</sup>- +<a href="/articles/carcinoid-syndrome">carcinoid syndrome</a> <sup>1,2</sup>
-</ul><h4>Ultrasound: echocardiography</h4><p>Echocardiography is the most common imaging modality used to evaluate patients with CCF <sup>1,2</sup>. It is able to provide a semi-quantitative assessment of left ventricular size and function, and determine the presence of valvular or wall abnormalities <sup>1,2</sup>. </p><h4>MRI</h4><p>Cardiac MRI (CMR) is able to provide highly accurate ejection fraction estimates and determine presence of any structural abnormalities <sup>2,9,10</sup>. Patterns of late gadolinium enhancement can distinguish between many aetiologies of CCF, although this is beyond the scope of this general article on CCF <sup>9,10</sup>.</p><h4>Treatment and prognosis</h4><p>Treatment involves a multidisciplinary team and incorporates lifestyle, allied health, pharmacological, and even surgical therapies, often specific to the underlying aetiology <sup>1,2</sup>. An in-depth review of the treatment of CCF is beyond the scope of this article, however general principles include:</p><ul>- +</ul><h4>Ultrasound: echocardiography</h4><p>Echocardiography is the most common imaging modality used to evaluate patients with CCF <sup>1,2</sup>. It is able to provide a semi-quantitative assessment of left ventricular size and function, and determine the presence of valvular or wall abnormalities <sup>1,2</sup>. </p><h4>CT</h4><p>CT chest may demonstrate the same features as the plain radiograph, but in greater detail and clarity <sup>6,7,9</sup>. Furthermore, electrocardiograph-gated CT and cardiac CT angiography may provide estimates of cardiac function and detailed visualisation of various cardiac structures <sup>9</sup>.</p><h4>MRI</h4><p>Cardiac MRI (CMR) is able to provide highly accurate ejection fraction estimates and determine presence of any structural abnormalities, and is considered by many to be the gold standard imaging modality <sup>2,9-11</sup>. Patterns of late gadolinium enhancement can distinguish between many aetiologies of CCF, although this is beyond the scope of this general article on CCF <sup>10,11</sup>.</p><h4>Treatment and prognosis</h4><p>Treatment involves a multidisciplinary team and incorporates lifestyle, allied health, pharmacological, and even surgical therapies, often specific to the underlying aetiology <sup>1,2</sup>. An in-depth review of the treatment of CCF is beyond the scope of this article, however general principles include:</p><ul>
-<li>mortality benefit: angiotensin-converting-enzyme inhibitors, angiotensin II receptor blockers, combination angiotensin receptor-neprilysin inhibitors, beta-blockers (only carvedilol, bisoprolol, metoprolol succinate, nebivolol), spironolactone <sup>1,2,11</sup><ul><li>these medications only have a benefit in patients with HFrEF, there are no medications with a mortality benefit in HFpEF (as of December 2017) <sup>1,2</sup>- +<li>mortality benefit: angiotensin-converting-enzyme inhibitors, angiotensin II receptor blockers, combination angiotensin receptor-neprilysin inhibitors, beta-blockers (only carvedilol, bisoprolol, metoprolol succinate, nebivolol), spironolactone <sup>1,2,12</sup><ul><li>these medications only have a benefit in patients with HFrEF, there are no medications with a mortality benefit in HFpEF (as of December 2017) <sup>1,2</sup>
-<li>surgery: considering implantable cardioverter-defibrillators, pacemakers, ventricular assist devices, and even cardiac transplant, depending on severity and aetiology <sup>1,2</sup>- +<li>surgery: considering implantable cardioverter-defibrillators, cardiac resynchronisation therapy, ventricular assist devices, and even cardiac transplant, depending on severity and aetiology <sup>1,2</sup>
-</ul><p>Despite advances in management in recent decades, prognosis remains poor with 30-40% of patients dying within 1 year, and up to 70% dying within 5 years <sup>1</sup>.</p><h5>Complications</h5><ul><li>acute decompensated heart failure and <a title="Acute pulmonary oedema" href="/articles/pulmonary-oedema">acute pulmonary oedema</a>- +</ul><p>Despite advances in management in recent decades, prognosis remains poor with 30-40% of patients dying within 1 year, and up to 70% dying within 5 years <sup>1</sup>.</p><h5>Complications</h5><ul><li>acute decompensated heart failure and <a href="/articles/pulmonary-oedema">acute pulmonary oedema</a>
References changed:
- 9. Mangalat D, Kalogeropoulos A, Georgiopoulou V, Stillman A, Butler J. Value of Cardiac CT in Patients With Heart Failure. Curr Cardiovasc Imaging Rep. 2009;2(6):410-7. <a href="https://doi.org/10.1007/s12410-009-0052-3">doi:10.1007/s12410-009-0052-3</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/20369033">Pubmed</a>
- 10. Captur G, Manisty C, Moon J. Cardiac MRI Evaluation of Myocardial Disease. Heart. 2016;102(18):1429-35. <a href="https://doi.org/10.1136/heartjnl-2015-309077">doi:10.1136/heartjnl-2015-309077</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/27354273">Pubmed</a>
- 11. Peterzan M, Rider O, Anderson L. The Role of Cardiovascular Magnetic Resonance Imaging in Heart Failure. Card Fail Rev. 2016;2(2):115-22. <a href="https://doi.org/10.15420/cfr.2016.2.2.115">doi:10.15420/cfr.2016.2.2.115</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/28785465">Pubmed</a>
- 12. Jhund P & McMurray J. The Neprilysin Pathway in Heart Failure: A Review and Guide on the Use of Sacubitril/Valsartan. Heart. 2016;102(17):1342-7. <a href="https://doi.org/10.1136/heartjnl-2014-306775">doi:10.1136/heartjnl-2014-306775</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/27207980">Pubmed</a>
- 9. Captur G, Manisty C, Moon JC. Cardiac MRI evaluation of myocardial disease. Heart. <a href="https://doi.org/10.1136/heartjnl-2015-309077">doi:10.1136/heartjnl-2015-309077</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/27354273">Pubmed</a> <span class="ref_v4"></span>
- 10. Peterzan MA, Rider OJ, Anderson LJ. The Role of Cardiovascular Magnetic Resonance Imaging in Heart Failure. Cardiac failure review. 2 (2): 115-122. <a href="https://doi.org/10.15420/cfr.2016.2.2.115">doi:10.15420/cfr.2016.2.2.115</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/28785465">Pubmed</a> <span class="ref_v4"></span>
- 11. Jhund PS, McMurray JJV. The neprilysin pathway in heart failure: a review and guide on the use of sacubitril/valsartan. Heart. <a href="https://doi.org/10.1136/heartjnl-2014-306775">doi:10.1136/heartjnl-2014-306775</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/27207980">Pubmed</a> <span class="ref_v4"></span>
Image ( create )
Image ( create )
Image 2 X-ray (Frontal) ( create )

Image 3 X-ray (Frontal) ( create )

Image 4 X-ray (Frontal) ( create )

Image 7 CT (lung window) ( create )






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.