Post-primary tuberculosis is also known as reactivation tuberculosis or secondary tuberculosis. The typical upper zone predominant destructive pneumonia is due to an adaptive immune response in an immunocompetent host 1.
Pathology
Location
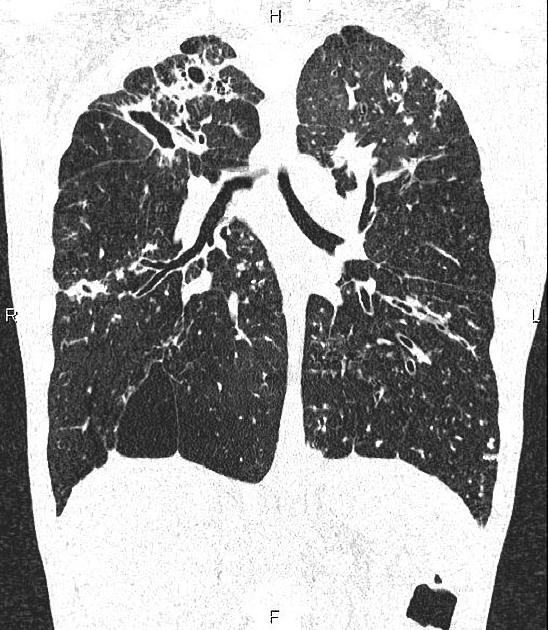
The upper zone predominance of pulmonary cavitation can explained by the relatively high oxygen tension and poor lymphatic drainage. Cavities commonly occur in:
the apical and posterior upper lobe
the superior segment of the lower lobe
The location is puzzlingly different from that of primary TB. TB DNA has been isolated from bone marrow, and it seems possible that bacteria remain dormant in the hypoxic environment of bone marrow mesenchymal cells. These may migrate to the lungs under certain circumstances such as respiratory infection. When the TB bacteria are in an oxygen-rich environment they proliferate.
The immunocompetent host has adaptive immunity from prior infection and the strong immune response results in destructive lung disease with cavitation. Tubercle bacilli proliferate in the cavities which communicate with the bronchial tree thereby facilitating endobronchial spread in the host and droplet spread to close contacts. Anti-tuberculous drugs do not enter the avascular cavities and treatment must be consistent and prolonged to effect cure. Without humans, there would be almost no transmission of TB 6,7.
Radiographic features
CT
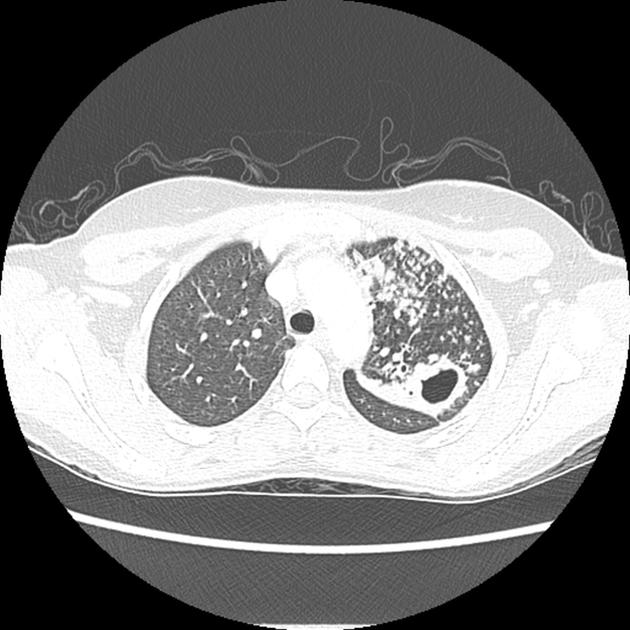
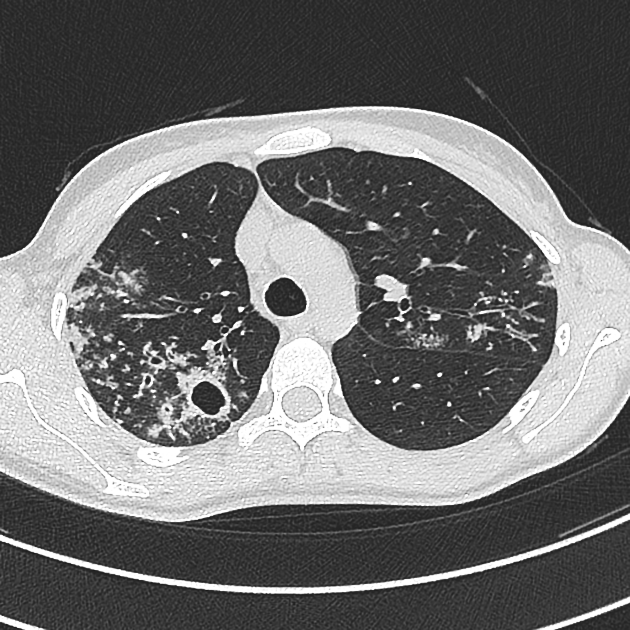
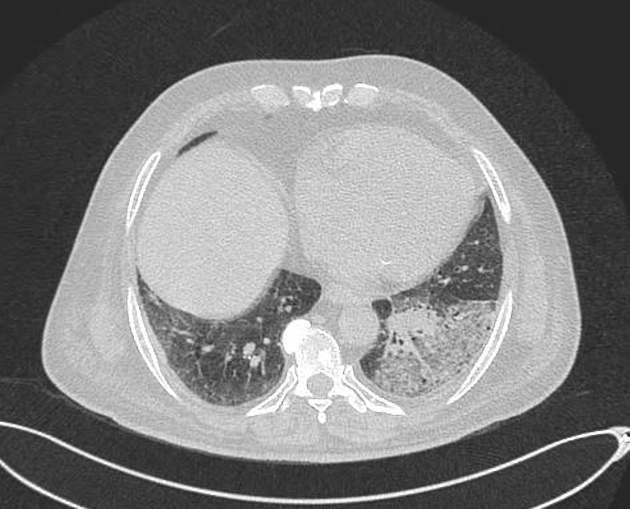
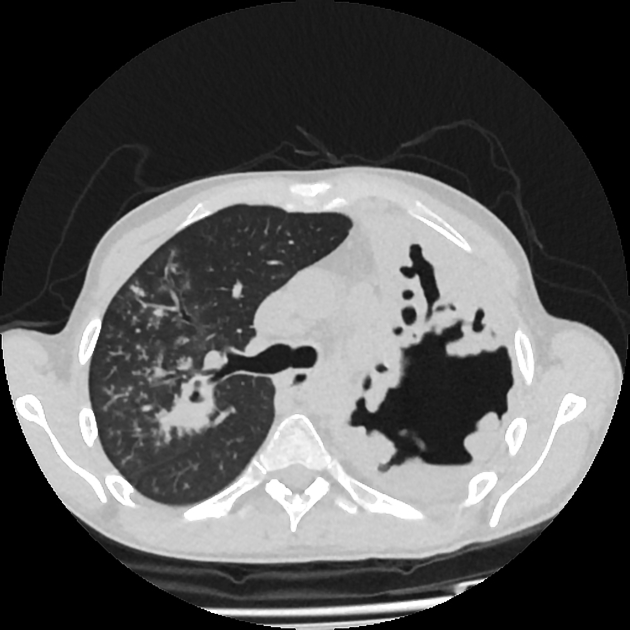
Parenchymal disease
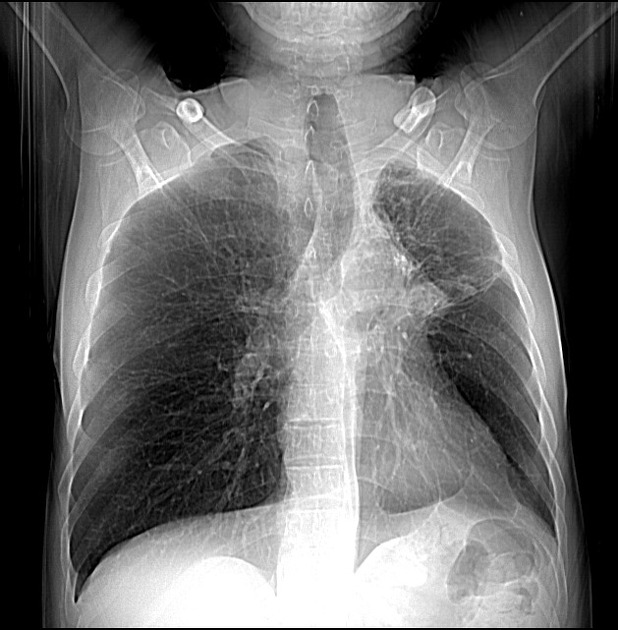
ill-defined patchy consolidation and cavitation with upper zone predominance
endobronchial spread with centrilobular nodules and tree-in-bud opacities
clustered parenchymal opacification with satellites may give rise to a galaxy sign
lymphadenopathy occurs only in 5% cases
healing results in fibro-calcific disease with volume loss and traction bronchiectasis
Airway disease
lobar collapse
Pleural disease
occurs in a minority of cases (18%)
small pleural effusion
empyema is less common
pleural thickening
pleural calcification
Chest wall involvement
Chest wall involvement occurring due to direct extension from pulmonary disease or empyema (empyema necessitans) manifests as bone and/or cartilage destruction and cutaneous fistula formation.









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.