De Quervain tenosynovitis, also known as washerwoman's sprain/strain, is a painful stenosing tenosynovitis involving the first extensor (dorsal) tendon compartment of the wrist (typically at the radial styloid). This compartment contains the abductor pollicis longus (APL) and extensor pollicis brevis (EPB) tendons.
On this page:
Epidemiology
De Quervain tenosynovitis is the second most common entrapment tendinopathy in the hand following trigger finger. It usually occurs in middle-aged individuals and is around 3x more common in women (~80% of cases). Most cases are associated with overuse, however, local trauma can also precipitate the condition. Mothers and childcare workers are particularly afflicted due to lifting of infants, while secretarial and nursing workers are also over-represented 6.
Clinical presentation
Patients present with pain on thumb and wrist movement and with focal tenderness and swelling over the radial styloid. There is usually a positive Finkelstein test (pain on passive ulnar deviation) although this is not pathognomonic. Triggering or crepitus may also be elicited 3.
Pathology
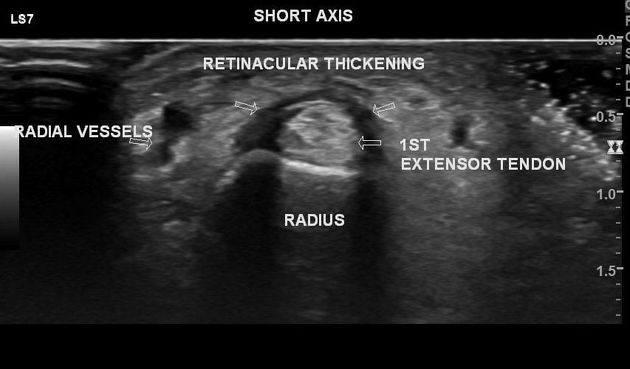
The APL and EPB tendons are tightly secured against the radial styloid by the overlying extensor retinaculum which creates a fibro-osseous tunnel approximately 1 cm in length 1. Thickening of the retinaculum and tendons from acute or repetitive trauma restrains normal gliding within the sheath. This causes inflammation and further edematous thickening of the tendon exacerbating the local stenosing effect. Microscopically there are inflammatory cells found within the tendon sheath 3.
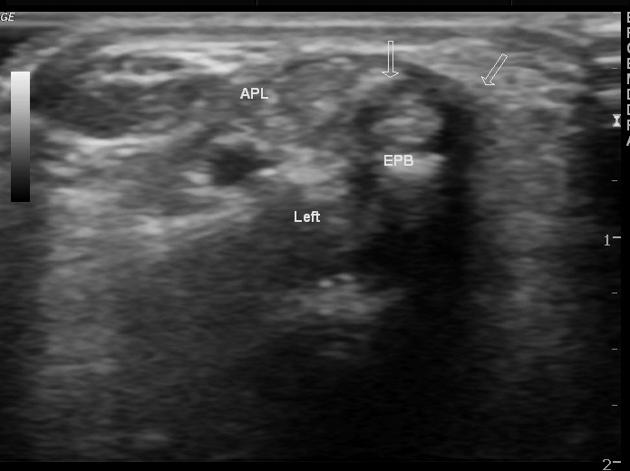
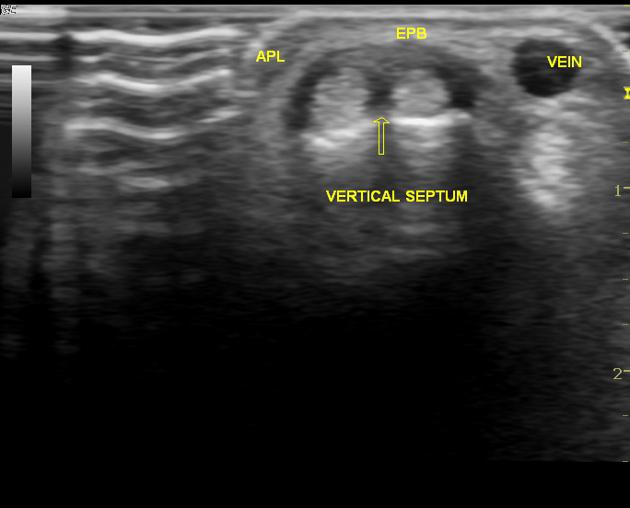
In ~10% of patients, there is an intertendinous septum between APL and EPB. The absence of a septum is associated with very high rates (almost 100%) of complete symptom resolution with conservative management. Presence of a septum increases the likelihood that surgical management will be required.
Radiographic features
Plain radiograph
Plain radiographs are non-diagnostic of the condition but may show non-specific signs and can help exclude other causes of pain such as fracture, carpometacarpal arthritis and osteomyelitis. Signs include:
soft-tissue swelling over the radial styloid
focal abnormalities of the radial styloid including cortical erosion, sclerosis or periosteal reaction 6
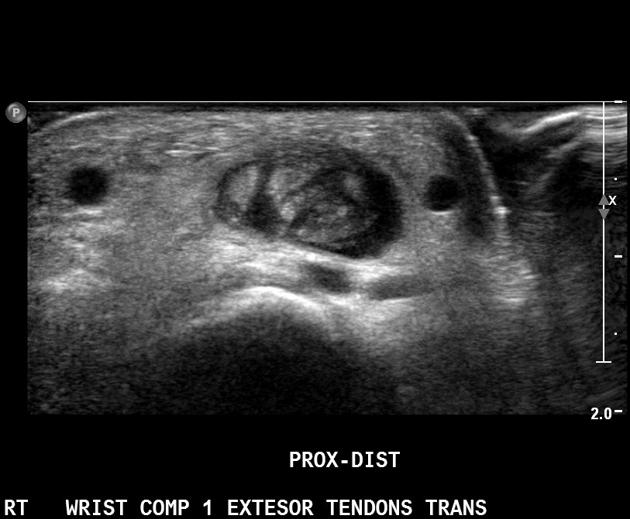
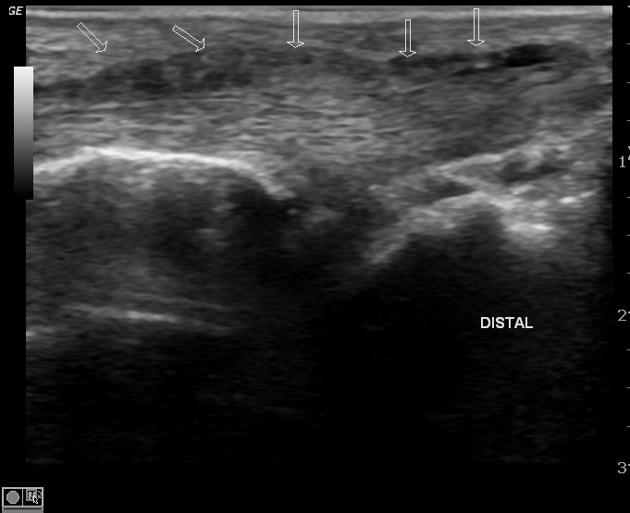
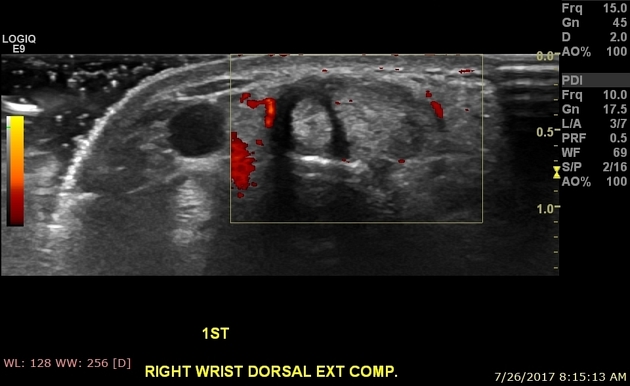
Ultrasound
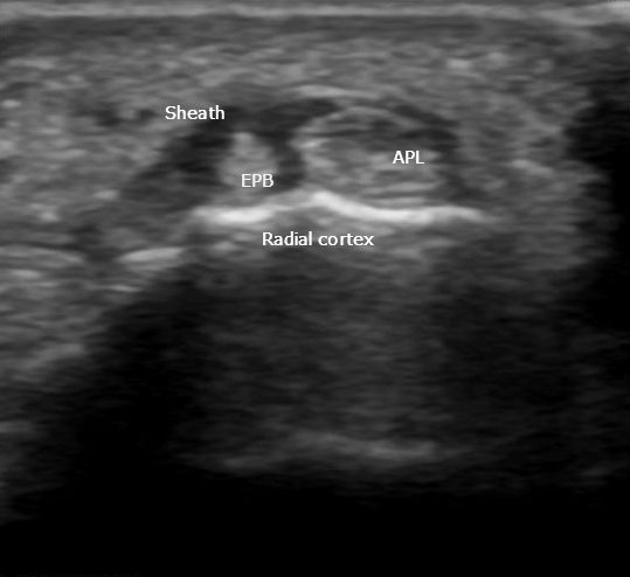
Ultrasound is very often diagnostic. Findings include 5:
edematous tendon thickening of APL and EPB at the level of the radial styloid (compare with the contralateral side)
increased fluid within the first extensor tendon compartment tendon sheath
thickening of overlying retinaculum and the synovial sheath
peritendinous subcutaneous edema resulting in a hypoechoic halo sign
peritendinous subcutaneous hyperemia on Doppler imaging
It is important to assess for an intertendinous septum which can usually be identified if present. Ultrasound is often used to guide corticosteroid injections into the tendon compartment to treat the condition.
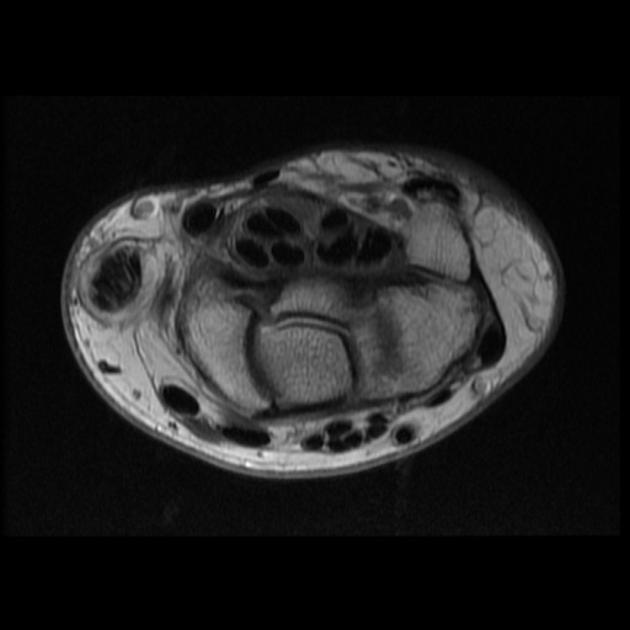
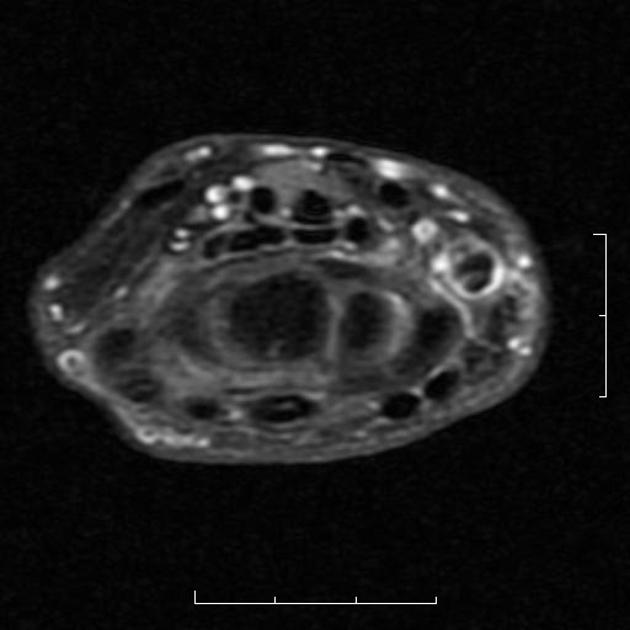
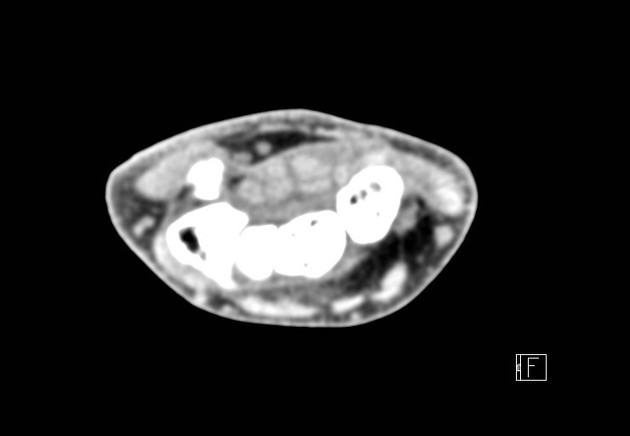
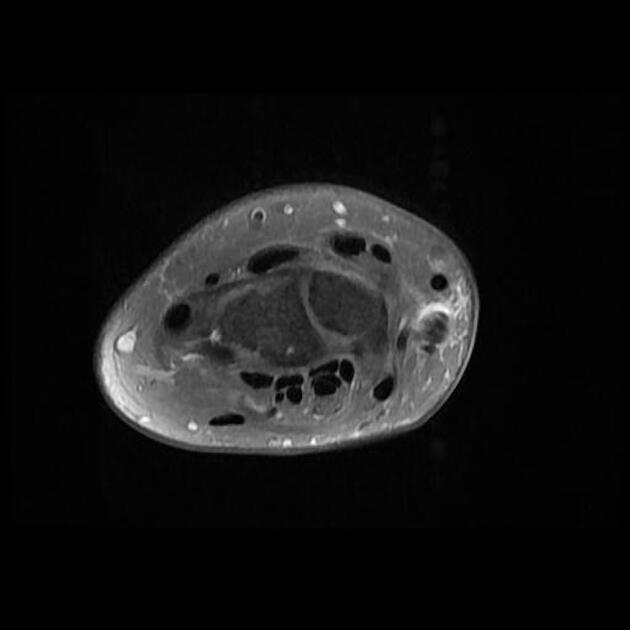
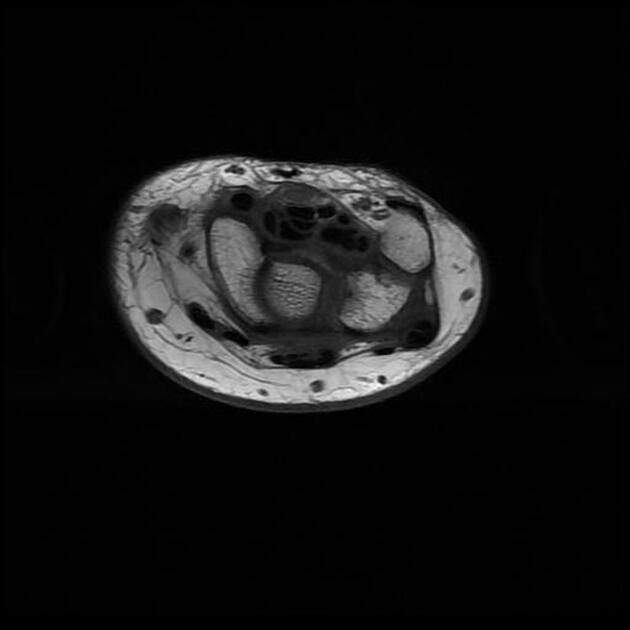
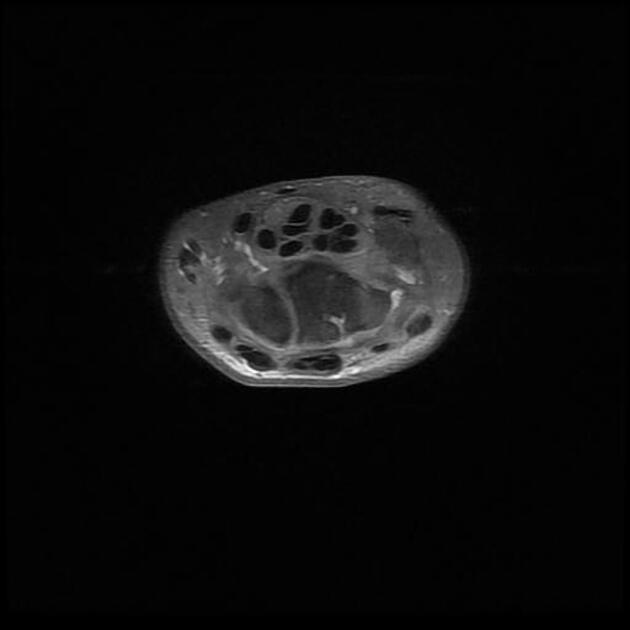
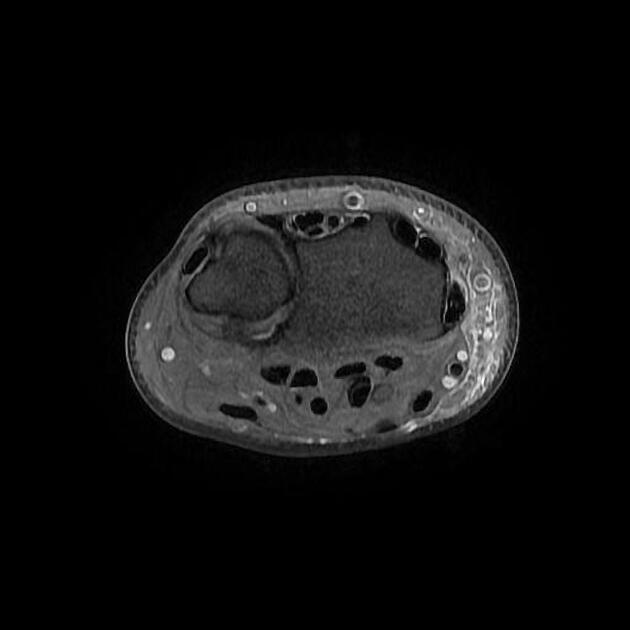
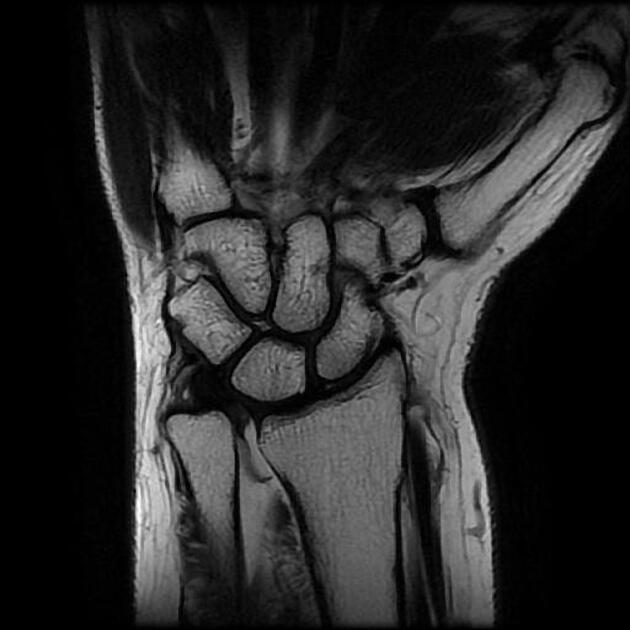
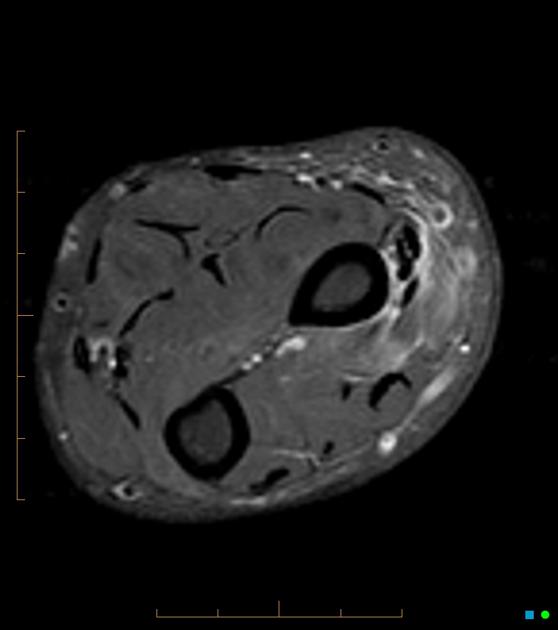
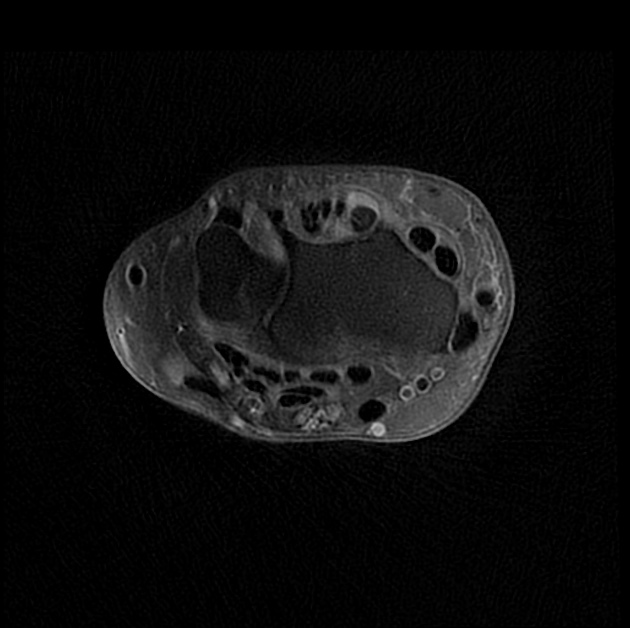
MRI
MRI is very sensitive and specific and useful for detecting mild disease where ultrasound may be equivocal. Presence or absence of intertendinous septum can be assessed. Findings include 3:
-
tenosynovitis
increased fluid within tendon sheath (high T2, low-intermediate T1)
debris within sheath (intermediate T1 signal)
thickened edematous retinaculum
peritendinous subcutaneous edema
peritendinous subcutaneous contrast enhancement
surrounding subcutaneous edema and increased intratendinous signal may be present as an ancillary feature 8
-
tendinosis
tendon enlargement maximal at radial styloid and often greater at the medial aspect of the tendon
slightly increased intratendinous T1 and T2 signal compared to other tendons
striated appearance of tendons due to multiple enlarged slips
-
longitudinal tendon tear
linear high T2 signal due to fluid within the split
more common in APL
Treatment and prognosis
Conservative treatment with anti-inflammatory medications, rest and splinting can be effective. Corticosteroid injection into the tendon sheath is usually very effective with 50% of patients experiencing symptom resolution after one injection. A second injection given at least a month later permanently relieves symptoms in another 40-45% of patients 4.
Rarely is surgical decompression required even when there is an intertendinous septum although this does increase the likelihood. Long-term complications are rare but can include perineural fibrosis of the superficial radial nerve and tendon instability after surgery 3.
History and etymology
The condition was first described by Fritz de Quervain (Swiss surgeon) in 1895 2. He is responsible for introducing iodinised table salt in order to help prevent goiter.
Differential diagnosis
On imaging consider:
tenosynovitis related to inflammatory arthropathies such as rheumatoid arthritis
-
occurs more proximally
peritendinitis of first and second extensor compartment tendons where they cross over each other ~4 cm proximal to Lister's tubercle







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.