Dural metastases, also known as pachymeningeal metastases, are a relatively common cause of dural masses, although they are less common than brain metastases and meningiomas. They can occur both within the spine and intracranially - this article is focused on intracranial dural masses.
On this page:
Clinical presentation
Patients may present with headache, fatigue, confusion and focal neurology such as contralateral motor and sensory changes or cranial nerve involvement 4. A significant number of dural metastases (~20%) may be clinically occult.
Pathology
There are four mechanisms by which intracranial dural metastases are thought to occur 2:
direct extension from skull metastases
retrograde seeding through the vertebral venous plexus
hematogenous seeding
lymphatic seeding
The primary malignancies that may cause dural metastases include (in descending order of frequency) 1,2:
head and neck cancers
hematological cancers
uterine leiomyosarcoma (very rare) 13
esophageal squamous cell carcinoma (very rare) 12
malignant carcinoid tumor (rare) 16
Radiographic features
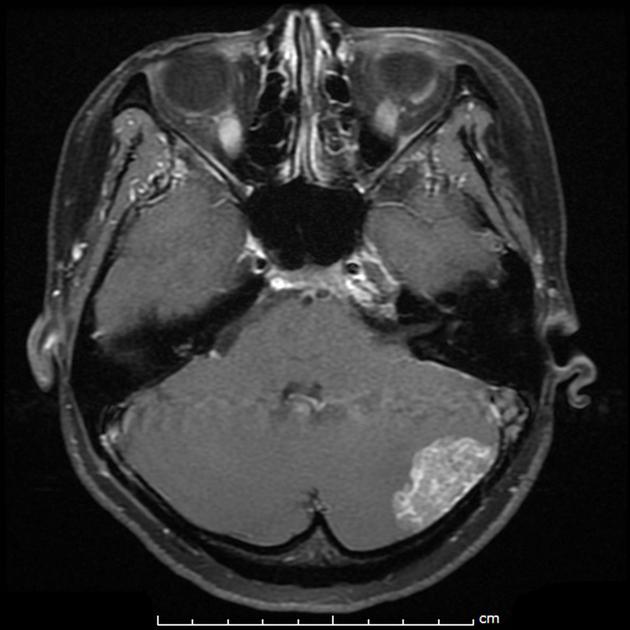
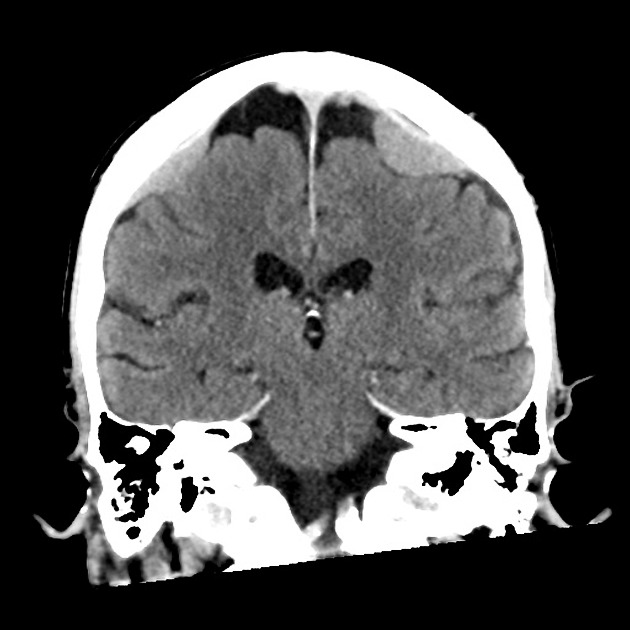
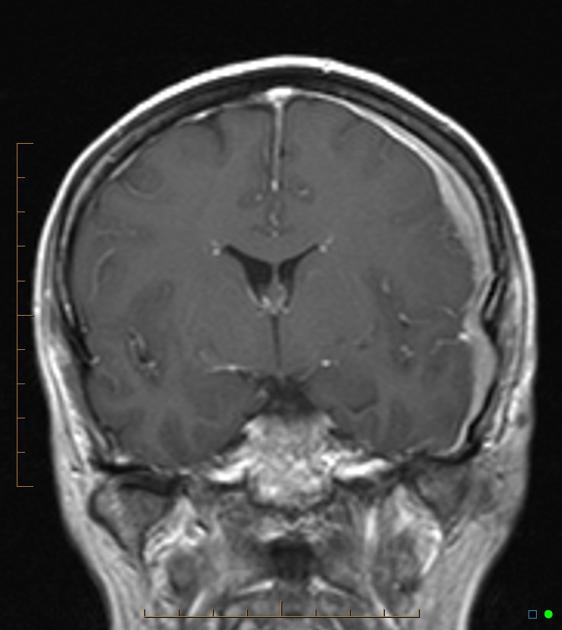
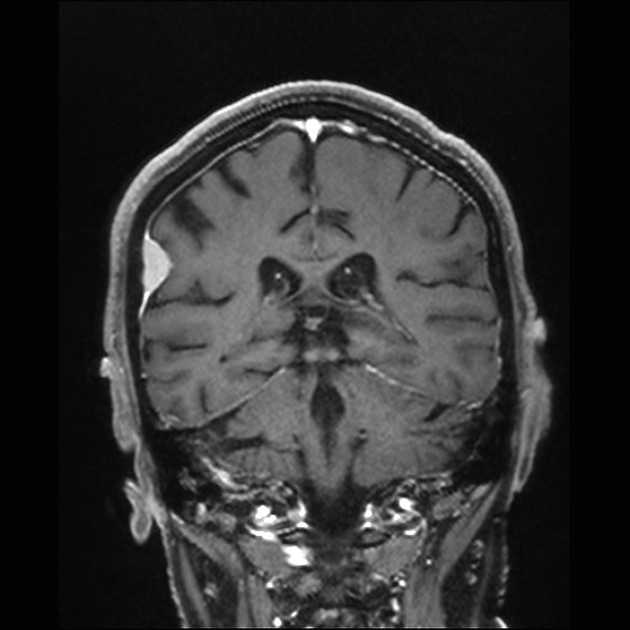
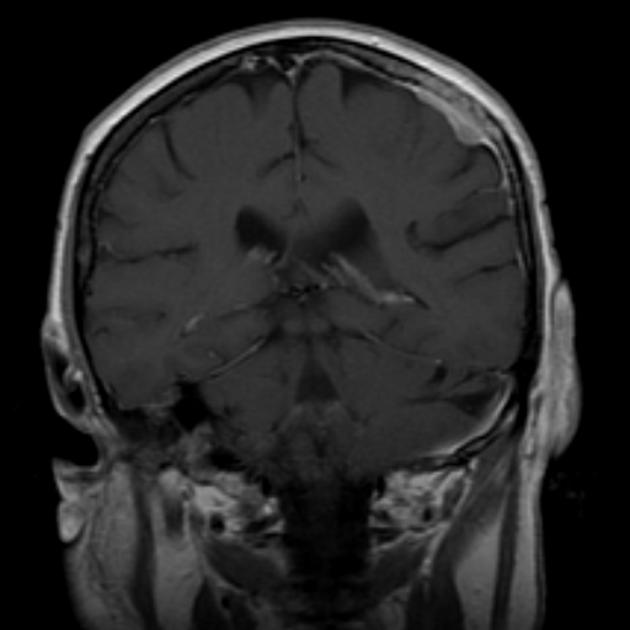
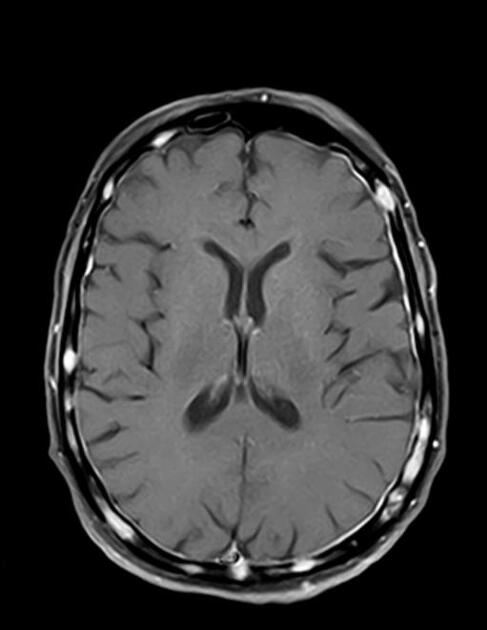
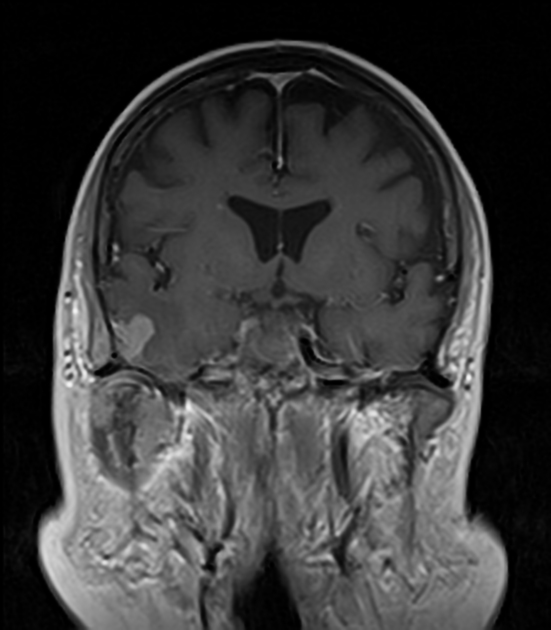
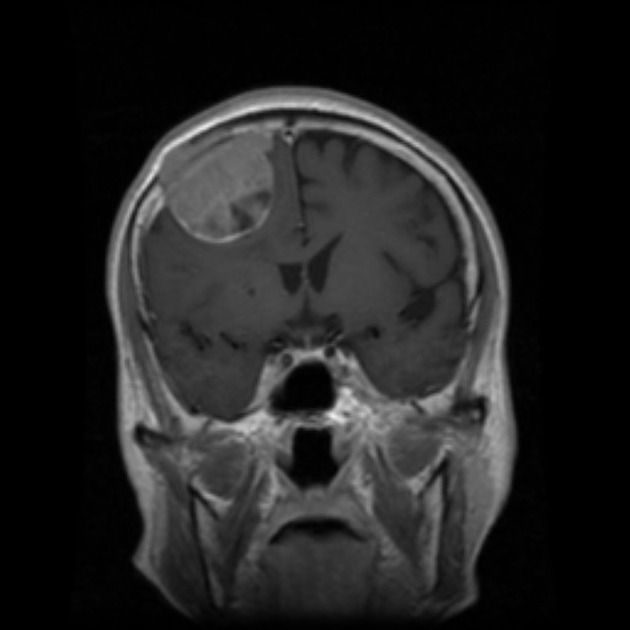
MRI
Dural metastases present as a focal mass, although there are typically multiple lesions. Signal characteristics include:
T1: typically iso/hypointense to adjacent cortex
T2: iso/hyperintense to adjacent cortex
T1 C+ (Gd): vivid enhancement 4
-
MR spectroscopy:
increased choline/creatine ratio 5
prominent lipid peak 5
occasional lactate peak 5
absence of NAA peak 5
Differential diagnosis
When mass like the differential diagnosis is essentially that of other dural masses particularly:
meningiomas: can look indistinguishable; dural based mass with "dural tail", hyperostosis and calcification; MRS: increased alanine peak and no lipid/lactate peak
hemangiopericytoma: can look identical; often has prominent T2 flow voids
CNS lymphoma dural involvement: diffusely enhancing dural mass, often multifocal, T2 low signal due to hypercellularity, no calvarial invasion
gliosarcoma: rare; often with dural involvement; heterogeneously enhancing parenchymal mass
CNS tuberculosis: strong dural thickening and enhancement with basilar predominance; usually abnormal chest x-ray; more common endemic areas and in immunocompromised patients
neurosarcoidosis: multifocal dural based masses; leptomeningeal enhancement; no skull involvement; abnormal chest x-ray and serum markers
chronic subdural hemorrhage: trauma history, fluid-fluid levels; varying density/intensity
extramedullary hematopoiesis: chronically anemic patients; smooth homogeneous dural based masses with strong homogeneous enhancement
When more diffuse the differential also includes other causes of dural enhancement, and sometimes if thin or irregular, it may be difficult to distinguish pachymeningeal metastases from leptomeningeal metastases or other leptomeningeal processes.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.