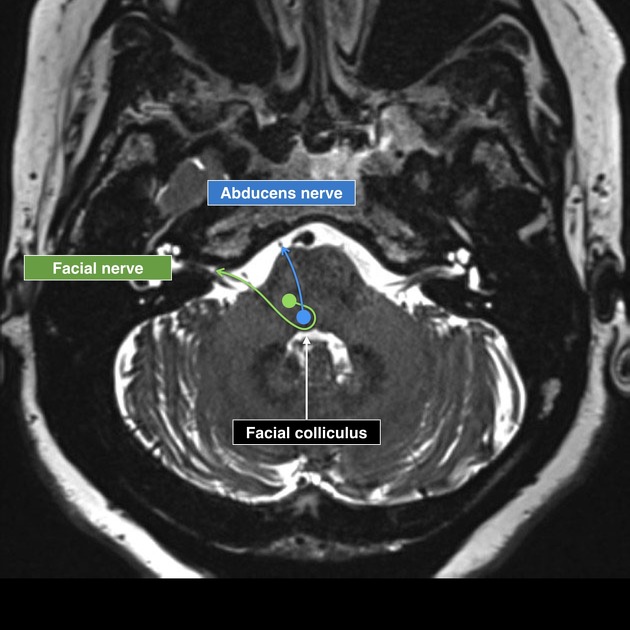
Facial colliculus syndrome refers to a constellation of neurological signs due to a lesion at the facial colliculus, involving:
abducens nerve (CN VI) nucleus
facial nerve (CN VII) fibers at the genu
On this page:
Clinical presentation
The presentation is varied and not all typical symptoms are necessarily present in every patient, depending on the size of the lesion:
-
facial nerve palsy: ipsilateral lower motor neuron pattern
sparing taste fibers and parasympathetic fibers which have their origins in the nucleus solitarius and superior salivatory nucleus, respectively and are, therefore, caudal
-
diplopia due to ipsilateral horizontal conjugate gaze palsy, which may accompany an internuclear ophthalmoplegia (known as one-and-a-half syndrome)
the combination of a one-and-a-half syndrome with a facial nerve palsy may be known as an eight-and-a-half syndrome
Pathology
The facial palsy is due to interruption of the ipsilateral facial nerve fibers at the genu as they arch behind the abducens nerve (CN VI) nucleus (thus forming the colliculus).
The conjugate gaze palsy is due to involvement of innervation not only to the ipsilateral abducens nerve to lateral rectus but also to the interneurons projecting into the medial longitudinal fasciculus which contribute innervation of the contralateral medial rectus. Because the medial longitudinal fasciculus can be involved in the lesion as well, a concurrent internuclear ophthalmoplegia may be present. However, this is not always the case.
Etiology
Causes of facial colliculus syndrome vary by age:
-
younger patients
tumor
demyelination (e.g. multiple sclerosis)
viral infection (e.g. rhombencephalitis)
-
older patients
vascular (e.g. stroke)
Radiographic findings
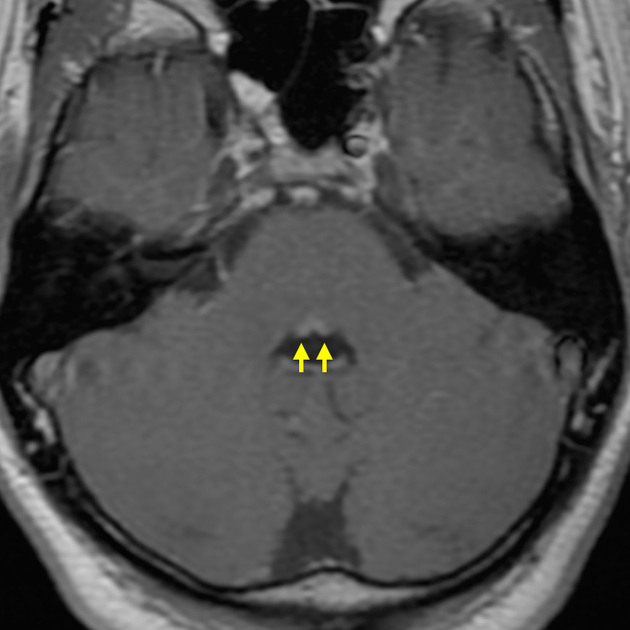
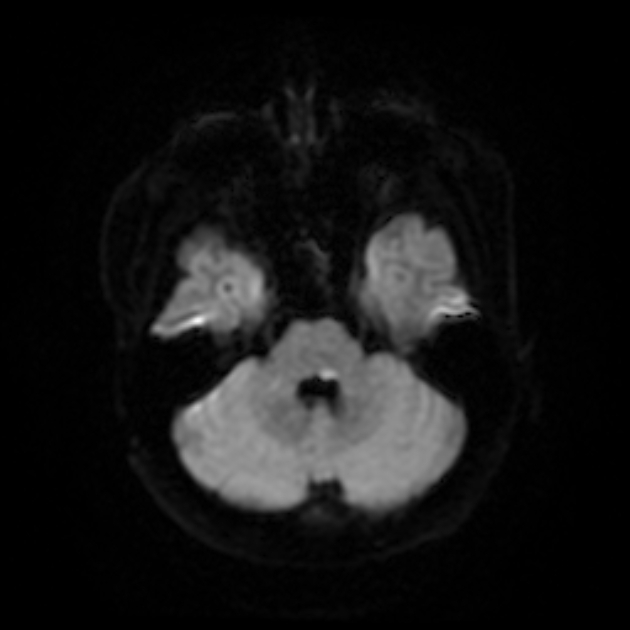
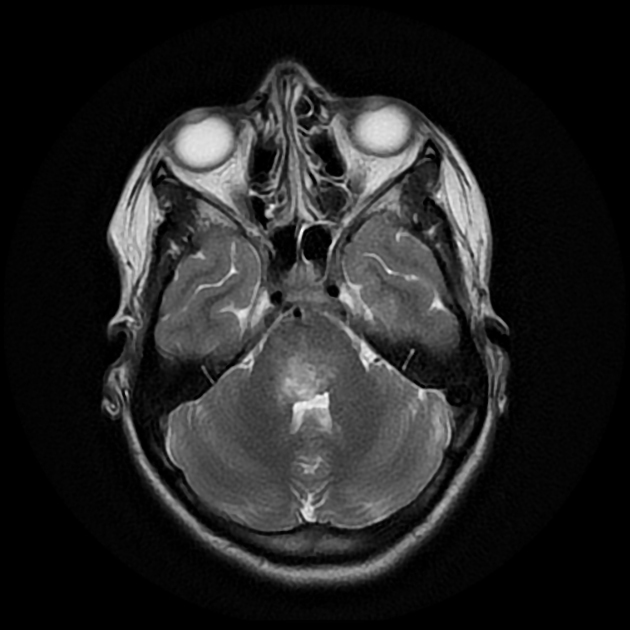
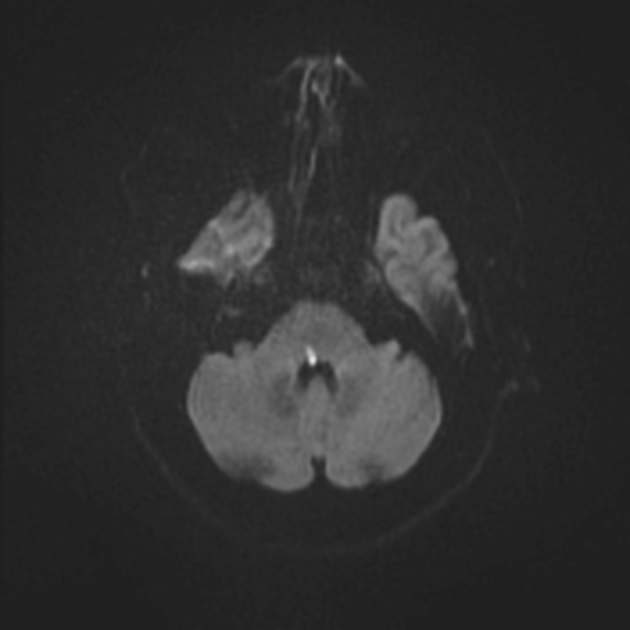
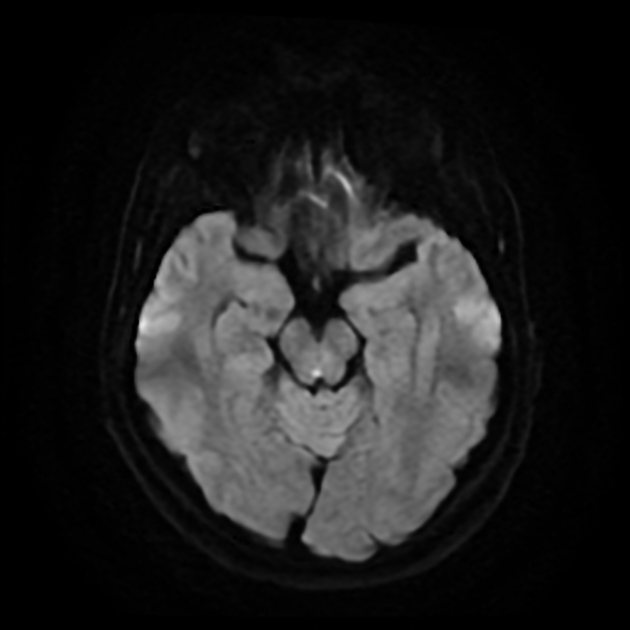
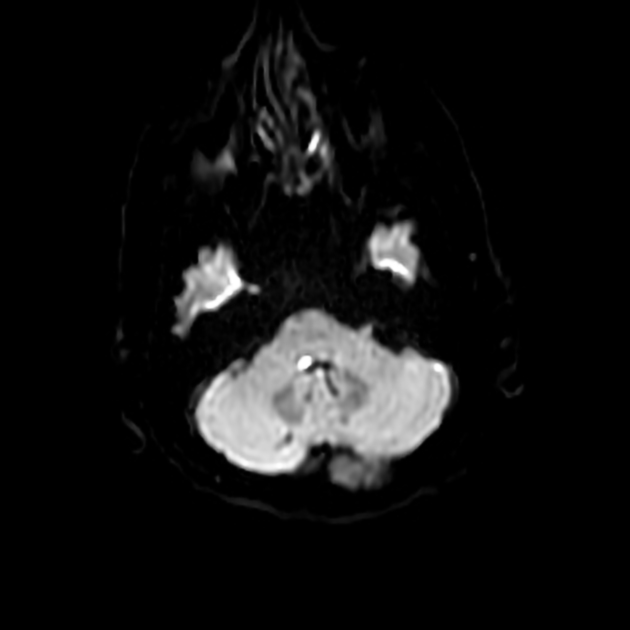
In cases of infarction, the lesion is usually only detected on MRI as a small focus of high signal in facial colliculus at the floor of fourth ventricle on DWI and/or T2/FLAIR sequences.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.