A patent foramen ovale (PFO) is a normal fetal interatrial connection which can persist into adult life. This can cause stroke due to paradoxical embolus.
On this page:
Terminology
Patent foramen ovale is an anatomical variant due to persistence of a normal fetal structure rather than a malformation, in contradistinction to atrial septal defects 21. Right to left shunting may occur through a patent foramen ovale at times of increased right atrial pressure such as sneezing, coughing, straining or Valsalva maneuver.
Epidemiology
The ultimate diagnosis of patent foramen ovale is at autopsy by testing for probe patency. One study found that 34% of adults had PFO by this measure. Individual variation is marked and affects size, shape and length. The majority do not cause clinical disease.
Clinical presentation
Patent foramen ovale can be an etiological factor in 22:
acute ischemic stroke (“cryptogenic” stroke), consider PFO in younger populations without conventional historical risk factors
systemic embolism to coronary arteries, gut, limbs, etc.
chronic migrainous headaches with aura - related to the size of the PFO and thought to be due to vasoactive substances which would normally be filtered by the lungs
platypnea-orthodeoxia - shunting typically occurs in the erect position and may occur following thoracic surgery which distorts the atrial septum 26
dysbarism in divers due to systemic gas embolism - nitrogen bubbles expand during ascent causing tissue damage and vascular occlusion 23
complications of carcinoid heart disease - circulating serotonin in metastatic carcinoid causes thickening, retraction and immobility of the right heart valves. Severe tricuspid regurgitation (TR) causes volume and pressure overload in the right atrium with increased incidence of PFO (60%). The right to left shunt means that active serotonin can then damage the left heart valves. Also, severe TR and pulmonary regurgitation (PR) can drastically reduce left ventricular preload. Closure of the PFO in this situation can cause circulatory collapse and this can be assessed by temporary balloon occlusion 28
Pathology
Patent foramen ovale is the name given to persistence of the vital fetal channel between the atria which allows blood to bypass the lungs until birth. With the onset of neonatal respiration, left atrial pressure rises and coapts the walls of the channel. Over the ensuing months the walls commonly adhere ensuring permanent closure. At autopsy, up to 34% of adults have probe patency of the PFO which may never have been clinically significant. Long-term elevation of right atrial pressure increases the patency rate (see carcinoid heart disease above). The width, length and shape of the tunnel show marked individual variation which can affect patency. The septum primum forms a flap valve at the fossa ovalis which may be seen on imaging. PFO flow is intermittent whereas an ASD is permanently open, and is due to failed overlap of the septum primum and septum secundum.
The foramen has been named for the entry point in the right atrium, the fossa ovalis. This is the area of the true atrial septum, devoid of septum secundum, where the atria are directly contiguous. The floor of the fossa ovalis is derived from the septum primum and the PFO exit is the ostium secundum, the secondary hole that develops in the septum primum to allow the fetal circulation to continue when the ostium primum closes.
Classification
One method of classifying PFOs uses binary division into simple or complex, with the latter characterized by one or more of the following characteristics 10:
-
defect anatomy
length exceeding 8 mm ("long tunnel")
wide atrial orifice
-
degree of shunting
shunting present at rest
complete left atrial opacification with agitated saline administration
-
associated features
atrial septal aneurysm
increased thickness of the septum secundum
prominent Eustachian ridge
Radiographic features
Ultrasound
Transthoracic echocardiography may suggest the presence of a patent foramen ovale by demonstrating right-to-left shunting not explained by a structural anomaly (e.g. atrial septal defect). As shunting may be intermittent and the interatrial pressure gradient insufficiently large to result in reliable detection with color flow Doppler, provocative maneuvers (e.g. Valsalva) and contrast enhancement are utilized to optimize detection 12. Transesophageal echocardiography is superior in its ability to diagnose the presence of a PFO and fully delineate atrial septal anatomy and the presence of associated defects . Other modalities which have been variably utilized include:
intracardiac echocardiography 27
Transthoracic echocardiography
Subcostal 16 or apical windows are commonly utilized, with the apical 4-chamber view typically considered optimal. The atrial septum is examined using 2D and color flow Doppler, and the presence of shunting assessed;
-
following the opacification of the right atrium with a positive contrast medium (commonly an intravenous admixture of saline and air, referred to as "agitated saline") a right-to-left shunt is diagnosed when any of the echogenic contrast bubbles appear in the left heart 15
prompt appearance (e.g. within fewer than three to six cardiac cycles) may favor intracardiac over intrapulmonary shunting 23,24
amount of contrast present sometimes used to semi-quantify size 19
-
shunting is dependent upon the interatrial pressure gradient, which may be augmented by maneuvers such as:
alteration of intrathoracic pressure by performing a Valsalva maneuver or alteration of mechanical ventilator settings 18
manual abdominal compression, patient repositioning
alteration of this gradient is dynamically confirmed by a shift of the convexity of the atrial septum toward the lower pressure chamber 20
bubbles crossing the mitral valve may result in high intensity transient signals deforming the velocity envelope visualized with pulsed wave Doppler (PWD) 17
Transesophageal echocardiography
-
commonly used imaging planes/views and salient features include:
-
mid esophageal aortic valve short axis
allows visualization of shunting at the superior extent of the atrial septum 13
-
mid esophageal bicaval view
-
visualization of the flaplike interface between the limbus of the septum secundum and the septum primum
measurements (e.g. tunnel/septal length) from this view important for planning closure
-
anatomical variants of structures associated with a higher prevalence of shunting which should be assessed include 14
-
-
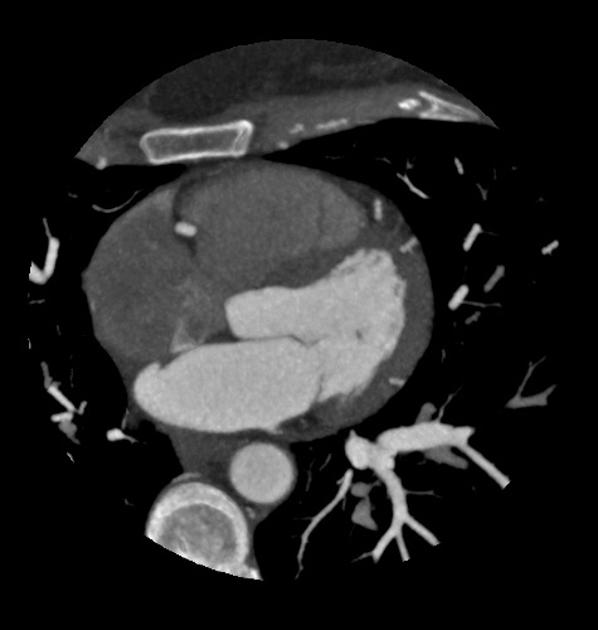
Cardiac CT
abnormal communication of contrast material between the atria through a channel-like tunnel in the interatrial septum
a channel-like tunnel alone is a normal variant of the fossa ovalis, and is not diagnostic
On ECG gated CT four types interatrial septum have been described 6
type 1: an interatrial septum (IAS) with no visible channel: no visible septal flap
type 2: a closed channel
type 3: an open channel with no visible jet flow of contrast material between the two atria
type 4: an open channel with a visible jet flow of contrast material between the atria
Types 3 and 4 comprised of PFOs.
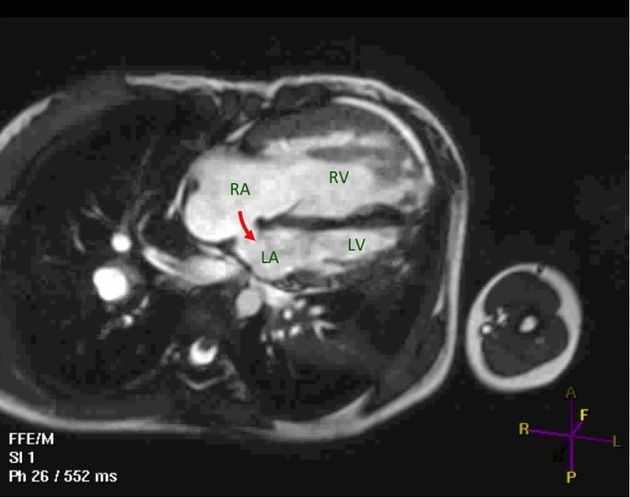
Cardiac MRI
not a first-line study, but may be diagnosed by visual assessment or computation of signal–time curves in the pulmonary vein and the left atrium 3
A patent foramen ovale can be differentiated from an atrial septal defect because a PFO takes a tunneled intraseptal course, or with the presence of a flap valve on the left atrial side of the foramen 2.
Treatment and prognosis
Closure devices, both surgically open and percutaneous, have been developed and are implemented in some centers for PFO 29.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.