CNS aspergillosis results from angioinvasive infection of the central nervous system by the fungus Aspergillus spp. Along with CNS cryptococcosis, it is one of the most common fungal opportunistic infections of the central nervous system.
On this page:
Epidemiology
The disease predominates in immunocompromised individuals, such as those with:
- AIDS
- prolonged high-dose corticosteroid use
- neutropenia
- graft-vs-host disease after allogeneic bone marrow transplantation 1-4
Clinical presentation
Patients with CNS aspergillosis have a very varied, and often subtle, presentation, making initial diagnosis difficult 1,2. However, the most common presenting features, with or without fever, are 1,2:
- altered mental status
- headache
- focal neurological signs (e.g. hemiparesis, dysarthria)
- lethargy
- seizures
Pathology
There are two mechanisms of spread of Aspergillus spp. to the CNS 1-3. Firstly, as per the pathogenesis of angioinvasive aspergillosis, spores of a variety of Aspergillus spp., most commonly Aspergillus fumigatus, are inhaled and proliferate in the alveoli, where the hyphae invade pulmonary arteries and gain access to the systemic circulation in 25-50% of cases 4. Once in the systemic circulation, spores can hematogenously spread to the CNS 1-4. Aspergillosis can also directly spread to the CNS via the paranasal sinuses, where it may manifest as invasive fungal rhinosinusitis 1-3.
Once in the CNS, the Aspergillus hyphae invade the walls of both small and large blood vessels 1,2. This either results in initial thrombosis leading to infarction, often followed by hemorrhage (in 25%), or development of mycotic aneurysms which can hemorrhage 1-3. This hemorrhage may lead to further parenchymal seeding of Aspergillus, resulting in infectious cerebritis and eventual brain abscess formation, often multiple in nature3.
Radiographic features
The disease can have a variety of radiographic presentations, but the main three findings are:
- brain abscess, often multiple, in a random distribution 1-3
- cerebral infarction(s) with or without associated hematoma(s) in a random distribution, although more likely to affect perforating artery territories 1-3
- invasive paranasal rhinosinusitis, either acute or chronic, with secondary intracranial dural enhancement consistent with intracerebral extension from the sinuses 1-3
CT
CT findings can be often non-specific but in keeping with at least one of the main three aforementioned findings that are characteristic of CNS aspergillosis 1-2. Detecting multiple such lesions in an immunosuppressed patient should prompt further investigation with MRI.
MRI
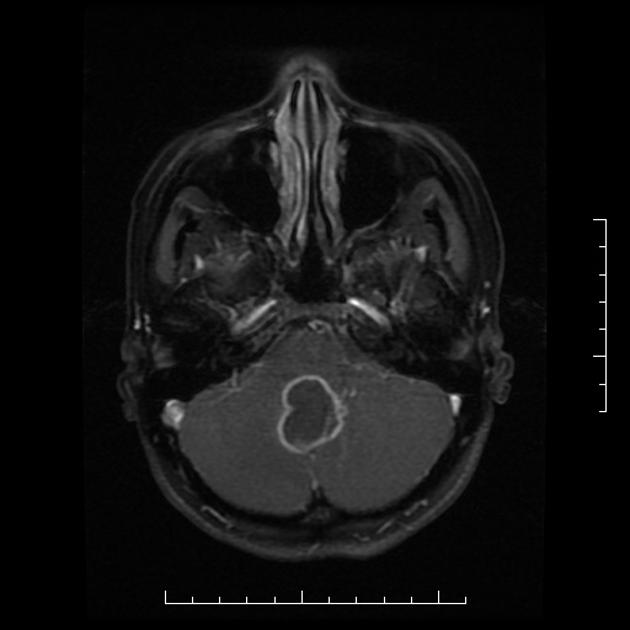
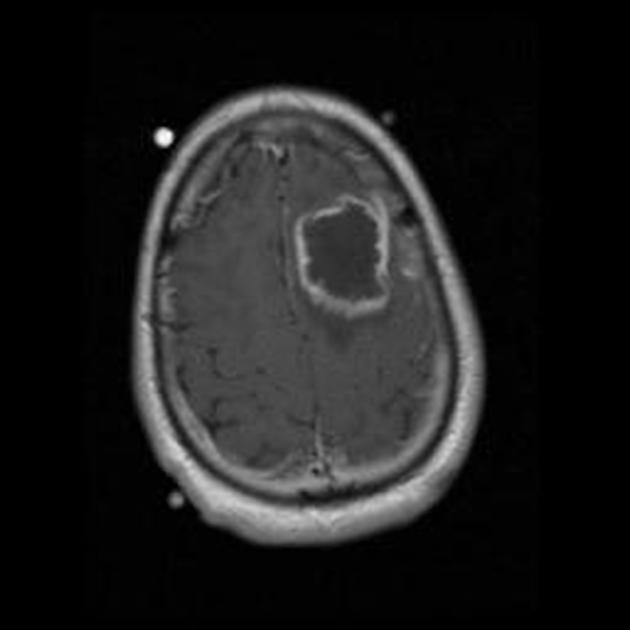
Aspergillus abscess and invasive fungal rhinosinusitis
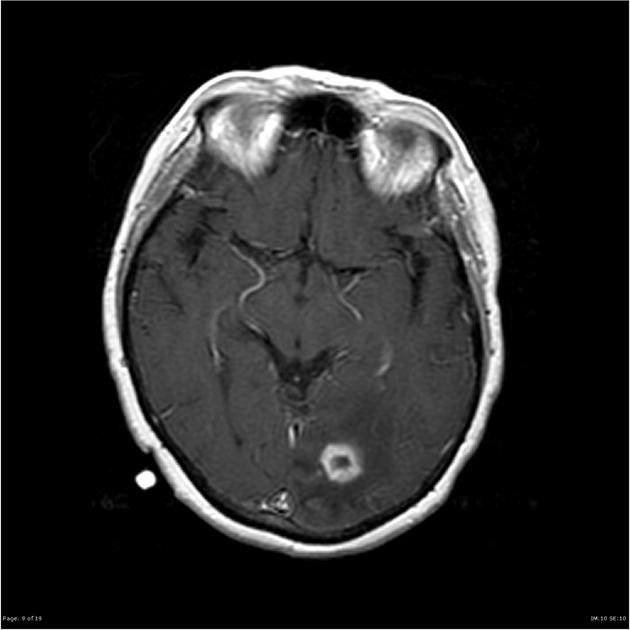
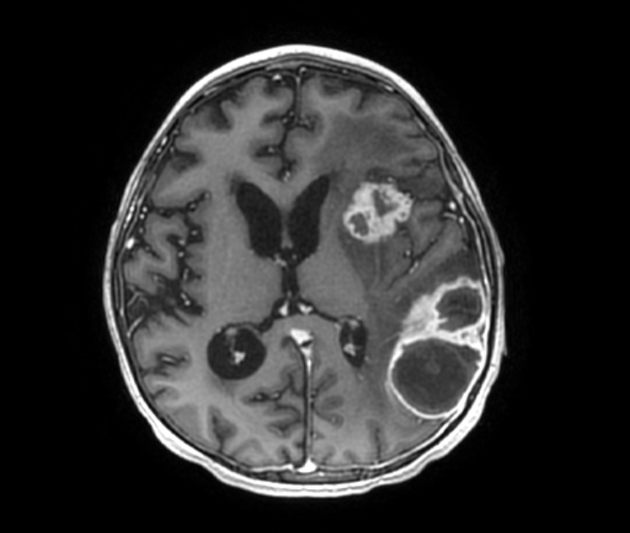
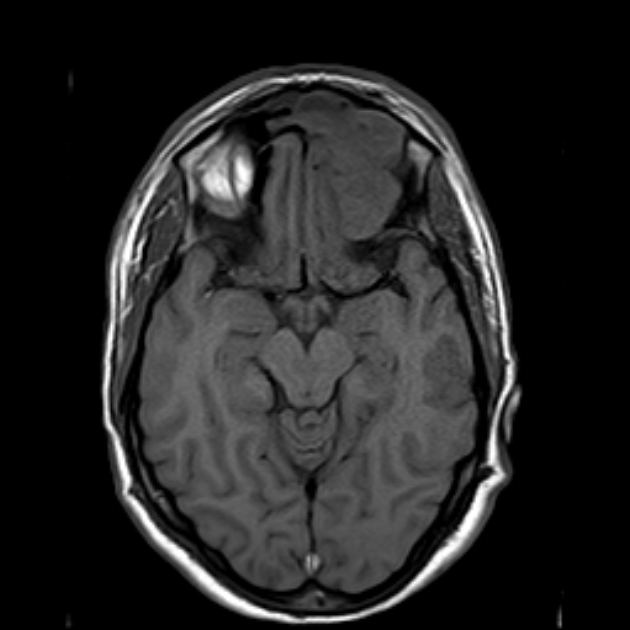
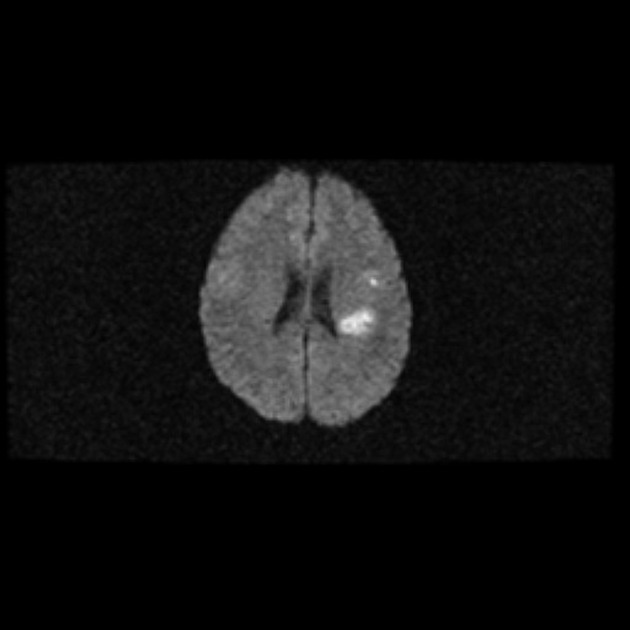
Abscesses (and prior regions of cerebritis) are often multiple, present in a random distribution, and appear radiologically identical to other brain abscesses as classic ring-enhancing lesions with striking high signal intensity on DWI 1-3,5. However, Aspergillus abscesses may also have peripheral low signal intensity on T2-weighted images 2. This is better appreciated on GRE or SWI images, and is likely due to hemorrhage around the abscess 2.
In cases where CNS aspergillosis is secondary to paranasal sinus disease, associated invasive rhinosinusitis (either acute or chronic), osteomyelitis, local dural enhancement and subdural empyema may be present 3.
Aspergillus infarction
Again, infarcts are often multiple, present in a random distribution, and are radiologically identical to other ischemic strokes 1-3,5, especially those of perforating artery territories 3. Hemorrhage is present in up to 25%, and mycotic aneurysms may or may not be identified 1. Infarction and associated hemorrhage have a variety of appearances on MRI depending on their age (see ischemic stroke and aging blood on MRI).
Other features
Rarely, CNS aspergillosis can present with a granulomatous tumor-like mass lesion 6,7. These, as described in case reports, are often hypo-to-isointense on T1-weighted images, hypointense on T2-weighted images, and demonstrate contrast enhancement on post-gadolinium T1-weighted images, but there is thought to be considerable variation 7,8.
Treatment and prognosis
CNS aspergillosis is treated with intravenous voriconazole 1-3,9,10, possibly in combination with caspofungin or liposomal amphotericin B 9. Neurosurgical opinion and intervention may also be sought 9. In immunocompromised hosts, which encompasses nearly all cases, it has a mortality approaching 100% if left untreated 1,2,10.
Differential diagnosis
General imaging differential considerations include:




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.