Iliotibial band (friction) syndrome is a common cause of lateral knee pain related to intense physical activity resulting in chronic inflammation of the fat adjacent to the iliotibial band (ITB). Alternatively, the same pathology can occur over the greater trochanter and is considered the same diagnosis.
On this page:
Epidemiology
Iliotibial band syndrome commonly affects young, physically active patients, most often long-distance runners or cyclists. The exact prevalence is unknown, but one study has found the prevalence among actively training marines to be higher than 20% 5. Iliotibial band syndrome accounts for 12% of running-related overuse injuries 4.
Associations
The following physical factors are reported to be associated with the development of iliotibial band syndrome 4:
limb length discrepancy
overpronation
hip adductor weakness
myofascial restriction
Clinical presentation
Classically, iliotibial band syndrome is diagnosed by history and physical examination. Pain over the greater trochanter or at the lateral knee joint is the presenting symptom with point tenderness 1-2 cm above the lateral joint line. Pain is usually worse with downhill running and increases throughout an episode of activity 4.
Pathology
When the knee flexes, the iliotibial band moves posteriorly over the lateral femoral epicondyle. When the band is excessively tight or stressed, the iliotibial band rubs against the epicondyle irritating the fat and connective tissue as well as an advential bursa in between.
With hip flexion, the iliotibial band slides anteriorly over the greater trochanter and may cause a painful clunking sensation or audible snap.
Microscopic appearance
In iliotibial band syndrome, histologic analysis demonstrates inflammation and hyperplasia in the synovium.
Radiographic features
Ultrasound
Allows visualization of the impingement by assessing the dynamic motion of the iliotibial band through knee flexion and extension.
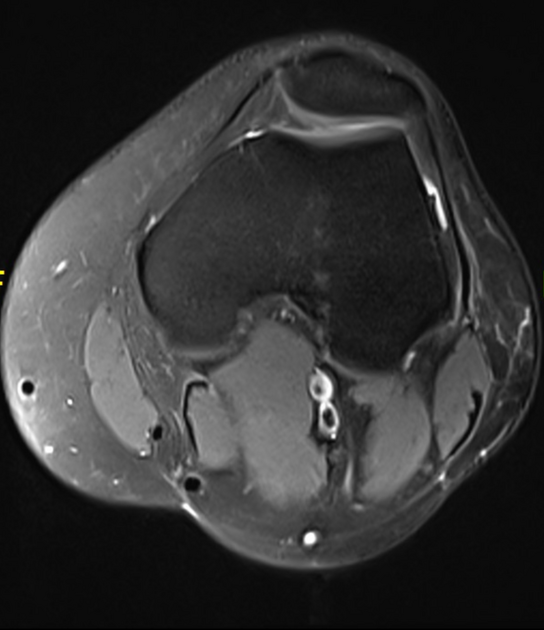
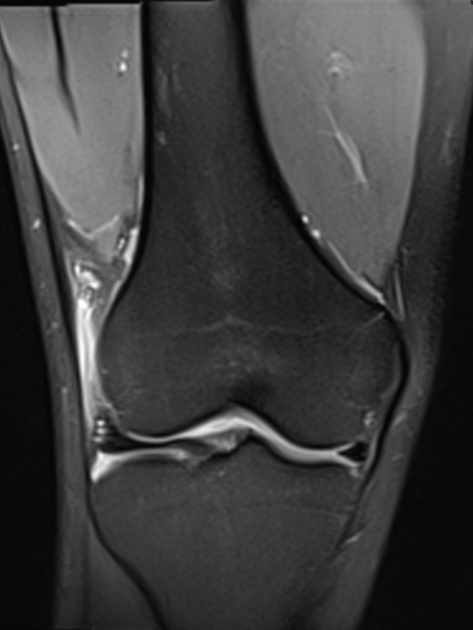
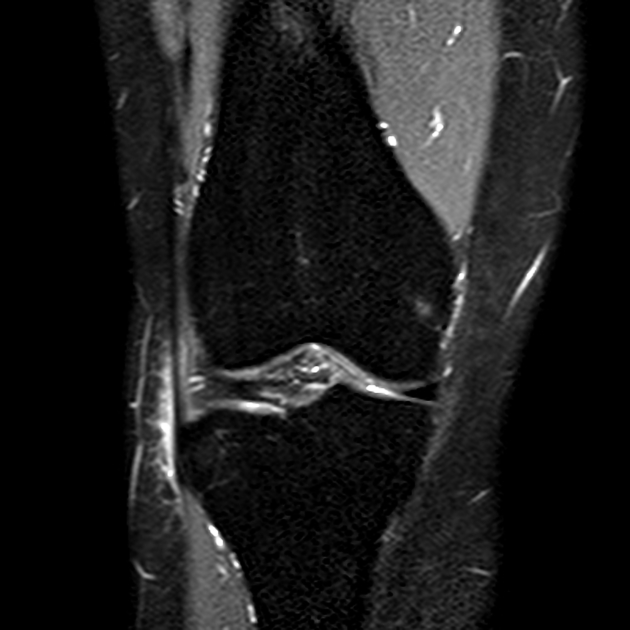
MRI
MRI is reserved for when the diagnosis is unclear and to exclude other etiologies of lateral knee pain such as a meniscal tear or lateral collateral ligament injury.
MR findings of iliotibial band syndrome include ill-defined signal abnormality within the fatty soft tissues interposed between the iliotibial band and bone. In the knee, the soft tissues lateral to the lateral femoral condyle show low T1 and high T2 signal, in keeping with edema/fluid. The signal changes commonly extend over or posterior to the lateral femoral epicondyle. In the hip, similar soft tissue changes are present and there may also be tendinopathy or tear of the gluteus medius or minimus tendons. There may also be marrow edema in the affected bone.
Cystic areas representing primary or secondary (adventitious) bursae may be identified.
Chronic MR findings include thickening of the iliotibial band and increased T2 signal intensity superficial to the iliotibial band are occasionally seen. Soft tissue fibrosis and bony proliferation may be present.
Treatment and prognosis
Initial treatment of iliotibial band syndrome is conservative, consisting of physiotherapy, anti-inflammatory medication, and steroid injections 3.
Surgical treatment is reserved only for those who fail conservative treatment and includes resection of the posterior aspect of the iliotibial band 3.
Differential diagnosis
General imaging differential considerations of lateral knee pain include:













 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.