Medullary thyroid carcinoma is a subtype of thyroid cancer that accounts for 5-10% of all thyroid malignancies. It occurs both sporadically (80%) and as a familial form.
On this page:
Epidemiology
In non-familial cases, it typically peaks in the 3rd to 4th decades.
Associations
When familial, it is seen as a component of multiple endocrine neoplasia type II (MEN2) syndromes (both MEN IIa and MEN IIb). Other associations include:
Diagnosis
The extent of radiologic evaluation is variable, depending on the suspicion of metastatic disease. Evaluation should uniformly begin with a neck ultrasound, to be supplemented by additional imaging if there are findings of extensive neck disease. Additional imaging may consist of a CT neck and thorax, multiphase CT/MRI of the liver, or bone scan. The efficacy of PET imaging for the assessment of metastatic disease is variable, and neither FDG nor fluoro-DOPA imaging is recommended for assessment 8.
Pathology
It is thought to arise from parafollicular C cells of the thyroid 4. Amyloid components may be seen on histology. It is characterized by consistent production of a hormonal marker (calcitonin), calcification of both primary and metastatic sites, and association with other endocrine neoplasms. Metastatic involvement may be seen in up to 50% at the time of presentation 4.
Radiographic features
Ultrasound
Punctate high echogenic foci resembling calcification may be seen both within the primary thyroid lesion as well as metastatic regional lymph nodes 3 and distant metastatic sites. Involved lymph nodes typically calcify.
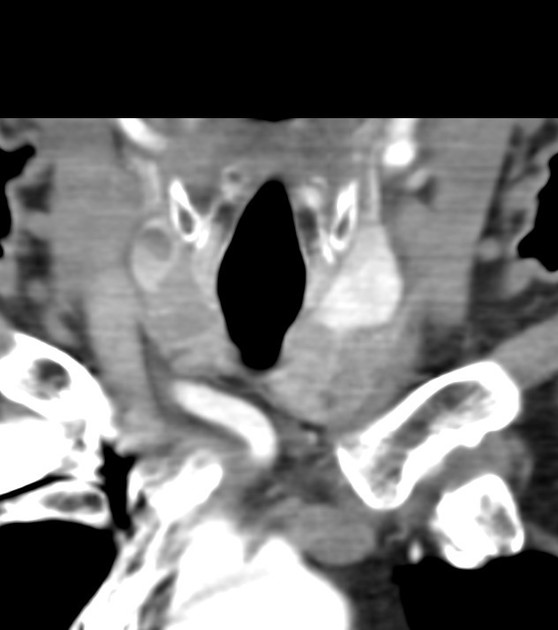
CT
Both primary and metastatic lesions usually have irregular dense calcific foci within 1.
In the chest, bullae formation and pulmonary fibrosis may develop as a result of a desmoplastic reaction.
Nuclear medicine
radioiodine: lesions do not concentrate radioactive iodine since the tumor does not arise from thyroid follicular cells
-
FDG-PET
~75% (range 60-95%) sensitive for metastatic disease 6
Tl-201: has been shown to concentrate thallium-201 5
I-123 MIBG: 30% of medullary thyroid carcinomas show uptake if the thyroid is blocked with Lugol solution prior to the scan
Treatment and prognosis
As with any malignancy, staging of the disease is an important part of management to inform treatment planning and prognosis. Biochemical evaluation in the form of preoperative CEA and calcitonin levels is helpful to assess the functional capacity of the neoplastic cells. Higher levels of these markers roughly correspond to the size of the tumor and extent of nodal metastasis 7.
The standard treatment approach involves surgical resection of all known disease where feasible. This typically consists of a total thyroidectomy and neck dissection 8.
The prognosis of medullary thyroid carcinoma is generally worse than the papillary and follicular thyroid cancer subtypes 1.








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.