Digital breast tomosynthesis (DBT) is an imaging technique that allows a volumetric reconstruction of the whole breast from a finite number of low-dose two-dimensional projections obtained by different X-ray tube angles, with a geometric principle very similar to that applied in stratigraphic technique.
Background
Although direct digital mammography (FFDM - Full Field Digital Mammography) has improved the sensitivity of the method, especially in dense breasts, the number of false negatives (FN) is still high, largely due to the presence of dense tissue that may affect lesions conspicuity: the mammogram is, in fact, a ”summation image" that displays on a single plane a more or less visible representation of any structure crossed by the X-ray beam between input and output surfaces.
The theoretical solutions to the problem exist: the main among them is MRI, but this is not the ideal solution because it is expensive, time-consuming, and in many cases may not be available in the same department.
What is needed instead is a solution that is:
a) affordable (an add-on on the price of a mammogram),
b) fast (the radiologist must be able to perform the complementary examination immediately after evaluating the mammographic images)
c) practical (the examination should be performed in the same physical area by the same operators),
d) simple (a new method would require technicians and radiologists to learn new procedures for examination and assessment).
The phenomena of summation and subtraction, potentially responsible for the production of false-positive findings (FP) and for masking of true positive findings (TP), led in 1930 Alessandro Vallebona to create and implement the “stratigraphy” (hereinafter referred to as “tomography”), that is a complementary radiodiagnostic technique aimed at realizing of analytical images, namely representative just of the structures including in the pre-selected layers of the concerned region. This technique was not without its drawbacks, which include:
limited contrast resolution allowed by the intrinsic shading of the image;
presence of parasitic shadows (i.e. background noise);
high total dose delivered in multiple sequential acquisitions of considered useful layers.
Thanks to the flat-panel technology, a reinterpretation in the digital key of Vallebona’s tomography has been proposed as a tool for early detection: the DBT-Digital Breast Tomosynthesis.
Digital breast tomosynthesis
In DBT the X-ray tube makes an arc, during which a series of images are acquired, each of which is delivered a dose equal to a fraction of that provided in a standard mammogram. During the acquisition, any detector element receives in time sequence-related information on each object volume element. The set of digital projections thus contains complete structural information on all the object layers in the form of raw data. These are sent to a computer, whereby appropriate reconstruction algorithms will reconstruct the order and the correct summation of the projection values which allows, as a final result, to obtain sections comparable to those of conventional tomography, but exempt from the critical previously explained.
Tomosynthesis, therefore, does not provide direct projection images, but reconstructed images of any individual layers through several available algorithms, more or less efficient, each aimed to remove from reconstructed slice the upper and lower layers "structured noise".
Reconstruction algorithms used in the first generation of devices (including FBP-Filtered Back Projection algorithm, ideal for 360° CT acquisitions reconstruction, but not optimal in DBT reconstruction, in which it generates noise and artifacts) were today abandoned for iterative algorithms, such as the SART -Simultaneous Algebraic Reconstruction Technique, and the MLEM - Maximum Likelihood Expectation Maximization, which can improve imaging quality through the final reduction of streaking artifacts, as well the increasing of contrast-to-noise ratio, thus improving the visibility of microcalcifications and skin edge.
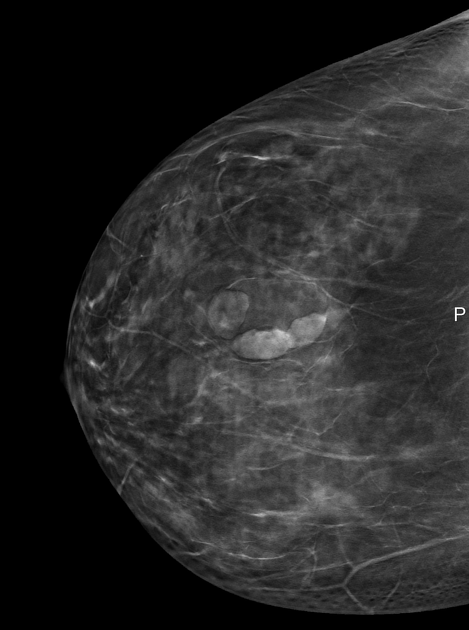
DBT allows the detection of a greater number of expansive lesions and a better morphological analysis of masses and architectural distortions, thanks to the contrast of findings greater than the background, given by the more shade structures belonging to the upper and lower layers, and then to the smaller amount of noise. It is thus exceeded one of the limits of two-dimensional imaging, which is the masking of lesions caused by the superimposition of normal structures.
The possibility of separating different layers suggests a possible reduction of false negatives and false positives due to overlapping.
According to early trial data, DBT is designed to offer the conspicuity of a higher percentage of breast cancers than conventional mammography, reducing false negative (FN) percentage at an estimated value of around 15%. Studies indicate about 30% increased DBT sensitivity and specificity compared to FFDM with a recalls reduction in screening by approximately 40%.
A further advantage of DBT is given by the lack of need for operator training (the breast is positioned just like conventional mammography in MLO and/or CC projection) and for the radiologist (as he continues to perform diagnosis from images with mammograms features).
It’s still ongoing a study comparing the clinical performance of FFDM in two projections (CC + MLO) and those of DBT in a single projection (MLO) in compliance with dose constraint. Until it will be demonstrated at least the clinical “non-inferiority” of DBT compared to FFDM, it is not reasonable a dose increasing in DBT. For this reason, the dose is restrained so as not to exceed the dose of a two-projections FFDM.
Features common to every DBT systems are the execution mode (MLO projection), acquisition time (10-20 sec) and reconstruction time (between 40 and 180 sec), slices thickness (1 mm), display mode (single slice, or slab cine loop), chance to perform standard mammograms and FFDM/DBT real-time selection with breast compression in place.
We can find, instead, great variability in the acquisitions number take-over (between 13 and 25) and the acquisition angle (between 15 ° and 50 °), significant features in image quality that in DBT depends on the dose and the number of projections and acquisition angle as well the number of exposures: so, if a narrow-angle with little exposure allows a fast but low-resolution 3D acquisition, a wide-angle with so many exposures provide a good resolution 3D but at a low-speed acquisition with consequent means of motion artifacts and quality deterioration of reconstructed images.
An interesting alternative is represented by variable geometry (V-DBT), which offers the highest 3D resolution at maximum speed acquisition due to a non-uniform sampling.
In V-DBT 13 images are taken through the 40° tube oscillation movement, the central one with 50% of the total dose delivered (the same as that required for a single mammography projection), and the remaining 50% unevenly split among the twelve remaining acquisitions.
Reconstruction algorithm in V-DBT system takes full advantage of any information provided in the 0° projection, which is basically a standard mammogram characterized by high contrast, which also provides valuable information for the microcalcifications visualization and their identification by 3D CAD, not yet available, but certainly among the future developments related to DBT.
In conclusion, DBT is definitely able to improve dense breasts imaging using a two- projections mammography dose, preserving high spatial resolution and quick workflow typical of FFDM. DBT can improve specificity in screening ruling out overlapping structures, facilitating so small lesions identification.
Iodinated contrast media may add more detailed information about blood supply dynamics of previously identified lesions, even compared to those obtained with CEDM - Contrast-enhanced digital mammography.








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.