Dysphagia refers to subjective awareness of difficulty or obstruction during swallowing. It is a relatively common and increasingly prevalent clinical problem. Odynophagia is the term for painful swallowing.
Fluoroscopy is the mainstay of imaging assessment but manometry can help evaluate the esophageal motor pattern and lower esophageal sphincter function 1.
On this page:
Epidemiology
Dysphagia is common in older age groups. Women are more prone to have dysphagia than men (80% vs 20%) 2.
Pathology
Dysphagia may be classified depending on the location of this sensation as oropharyngeal or substernal.
Dysphagia can be caused by functional or structural abnormalities of the oral cavity, pharynx, esophagus, and/or gastric cardia.
Oropharyngeal dysphagia
Oropharyngeal dysphagia occurs when a patient symptomatically localizes a sensation of blockage in the throat.
Functional causes
laryngeal penetration (when contrast seen entering the larynx at fluoroscopy) or aspiration (when contrast extends inferiorly through the true vocal), which are common with patients who have a history of neurologic disorders including stroke
post-operative: e.g. following thyroidectomy 8
Structural causes
esophageal diverticula, e.g. Zenker, Killian-Jamieson, and epiphrenic diverticula
tumors
-
extrinsic compression, e.g.
anterior osteophytes from cervical spine disease
hypertrophic cartilages e.g. superior thyroid cornu syndrome
occasionally as a complication of anterior cervical spine fusion (~4%) 6
Substernal dysphagia
Substernal dysphagia occurs when a patient symptomatically localizes a sensation of discomfort or blockage between the thoracic inlet and the xiphoid process.
Functional causes
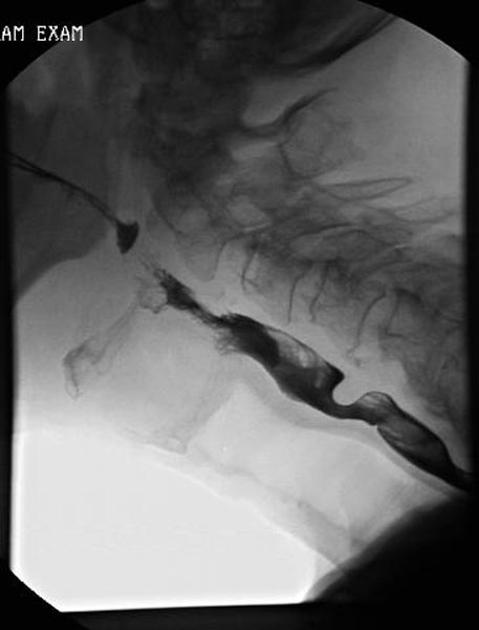
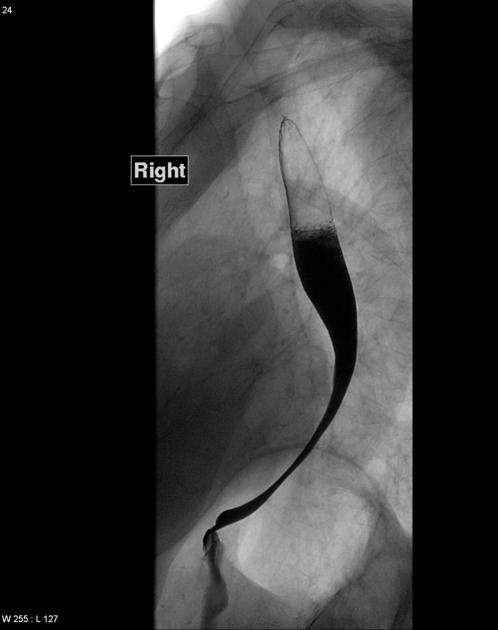
diffuse esophageal spasm (DES): characterized by multiple spontaneous and uncoordinated esophageal contractions which have the classic "corkscrew" appearance at esophagogram
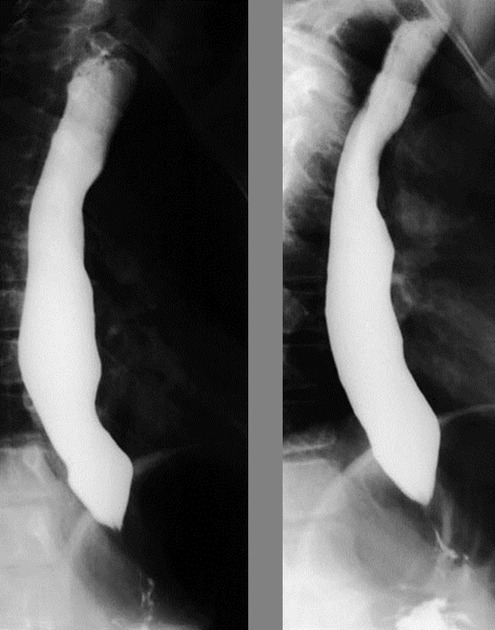
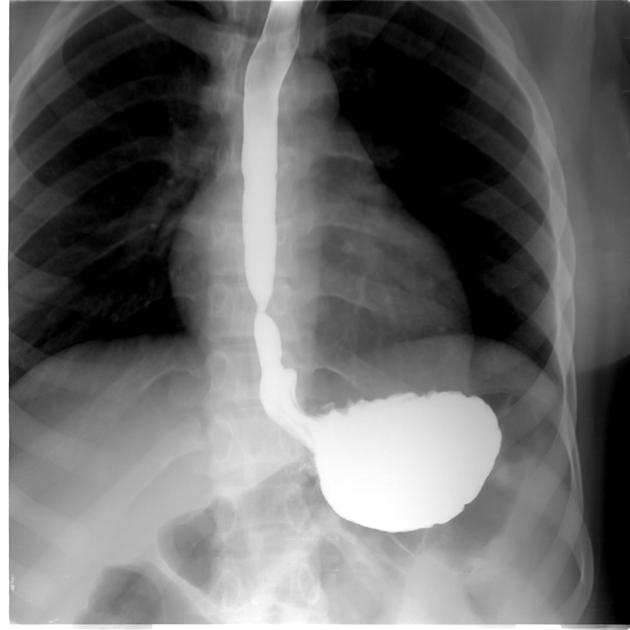
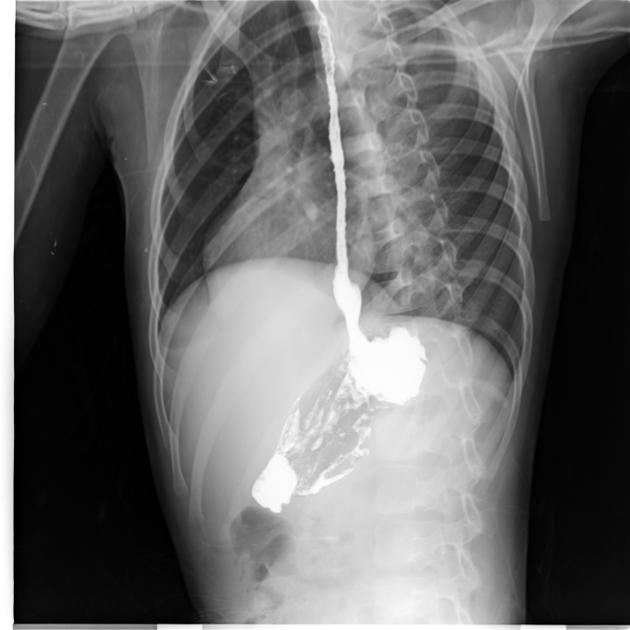
achalasia: characterized by esophageal dilatation with distal tapered beak-like narrowing at the gastro-esophageal junction
scleroderma: characterized by esophageal dilatation with a patulous gastroesophageal junction
Structural causes
-
peptic strictures most often typically appear as smooth, tapered narrowing in the distal esophagus
Barrett esophagus occurs often as a consequence of GERD in the mid-to-upper esophagus
ring stricture: Schatzki ring is the most common type of esophageal ring, associated with hiatus hernias
other less common causes of benign strictures include corrosive esophagitis, Crohn disease, Behçet disease, and eosinophilic esophagitis
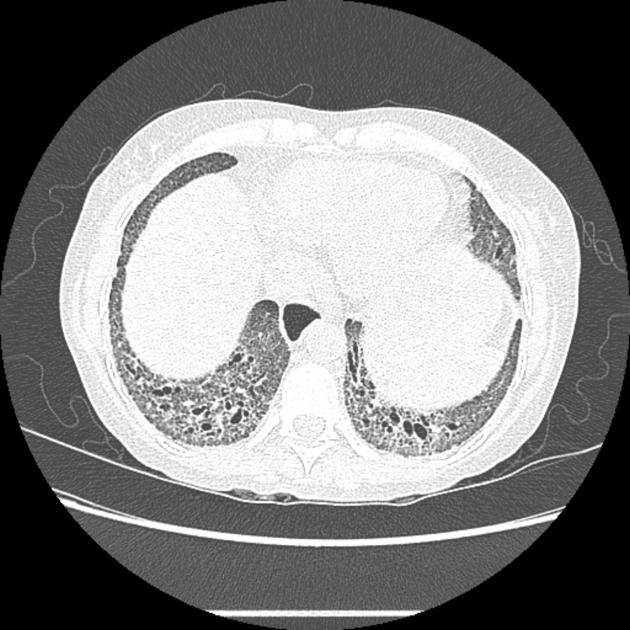
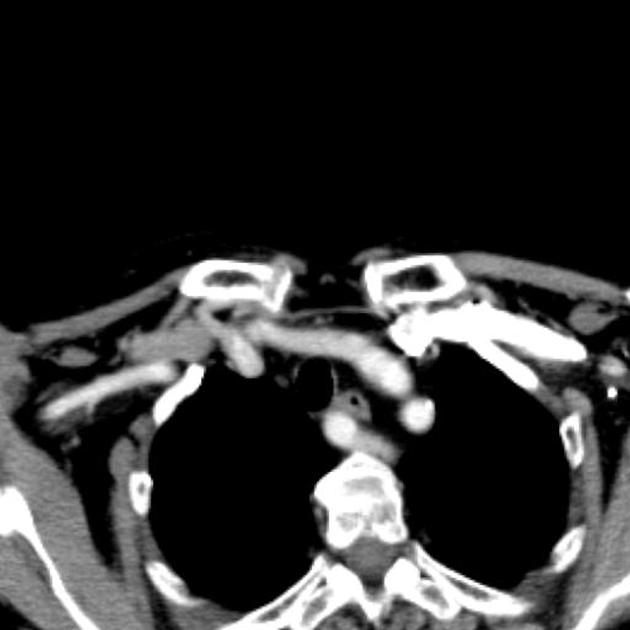
extrinsic mass such as lung cancer or vascular compression, e.g. aberrant right subclavian artery (i.e. dysphagia lusoria) or left atrial enlargement (i.e. dysphagia megalatriensis)
esophageal infections, such as candidiasis, herpes virus, human immunodeficiency virus (HIV), and cytomegalovirus (CMV)
esophageal carcinoma can appear infiltrative, ulcerative, polypoid, and/or varicoid at esophagography
impacted foreign body or food bolus in the esophagus; water-soluble contrast should be used for increased risk of perforation
Radiographic features
Fluoroscopy
modified barium swallow: used for the evaluation of swallowing mechanisms specifically for aspiration or penetration, this exam is usually performed in conjunction with a speech therapist to assess swallowing function and response to therapeutic strategies 4
barium swallow/esophagography: provides anatomic and functional information about the pharynx, esophagus, gastro-esophageal junction, and gastric cardia, including evaluation of esophageal motility and assessment for gastroesophageal reflux
-
barium tablet: may be used to detect subtle areas of esophageal narrowing 5
the tablet (of known 12.5 mm diameter) should be swallowed with a small amount of water and passage is observed at fluoroscopy; if the tablet becomes lodged in a particular location the patient should swallow a small amount of additional water and if the tablet remains lodged, a more detailed assessment should be performed
CT
Cross-sectional imaging may be used especially if there is a mass effect on the esophagus seen at esophagography or for evaluation of esophageal tumors.
Differential diagnosis
globus pharyngeus sometimes turns out to be the cause of the presentation, this is usually a diagnosis of exclusion









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.