Pleomorphic adenomas of the salivary glands, also known as benign mixed tumors (see below), are the most common salivary gland tumors. The salivary glands are the most common site of pleomorphic adenomas.
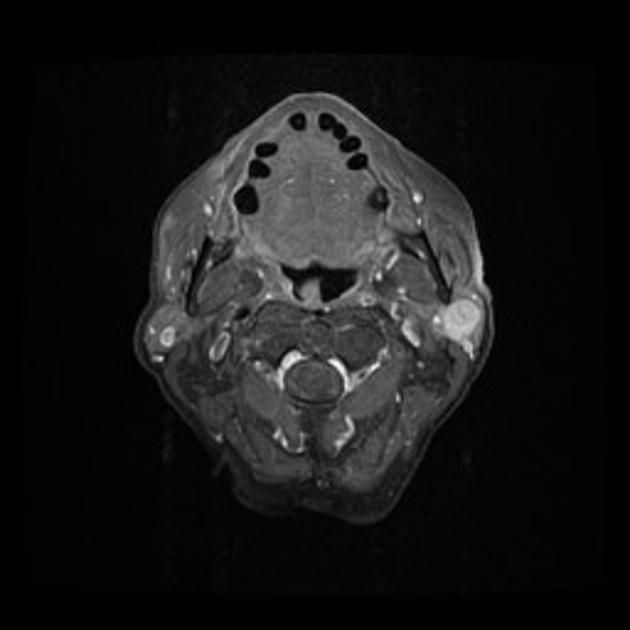
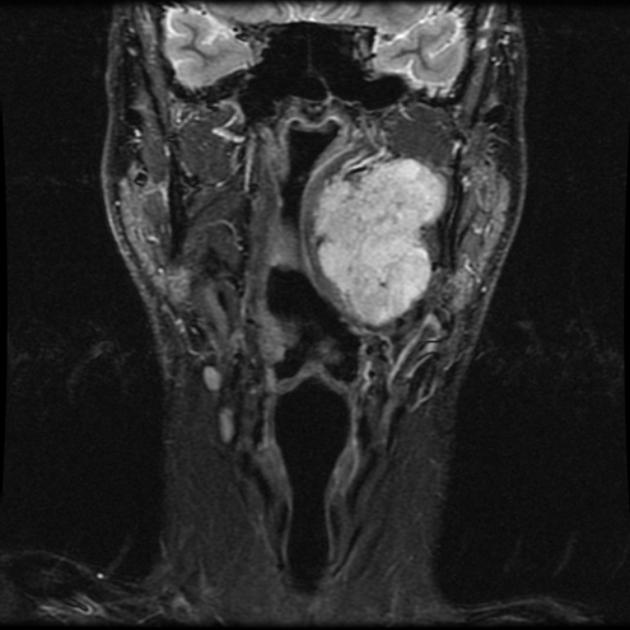
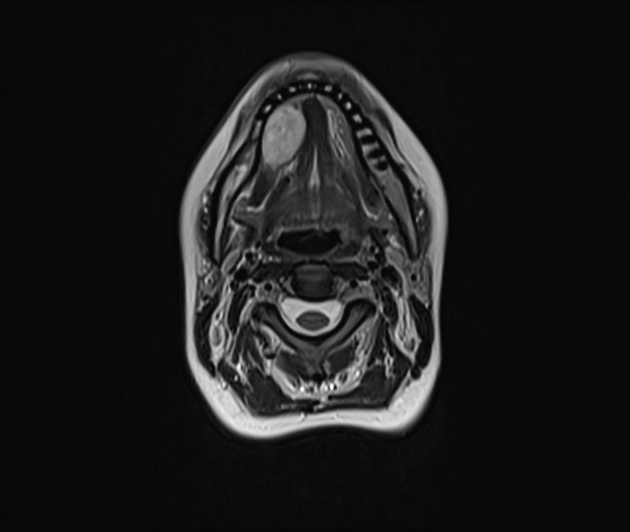
On imaging, they commonly present as well-circumscribed rounded masses, most commonly located within the parotid gland, hypoechoic on ultrasound, and bright on T2WI with homogeneous enhancement on MRI.
On this page:
Terminology
Historically pleomorphic adenomas have also been called benign mixed tumors, however, this name is now discouraged. It was previously thought that these were a form of teratoma, however, it is now clear that the neoplasm forms from a single layer of germ cells and is purely epithelial in nature 15.
Epidemiology
Pleomorphic adenomas account for 70-80% of benign salivary gland tumors and are especially common in the parotid gland, comprising the majority of all parotid gland tumors (see below) 1,6. Patients are typically middle-aged and the incidence is slightly higher in females than males (2:1) 1,13. The oncogenic simian virus (SV40) may play a role in onset or progression and prior head and neck irradiation is a risk factor for the development of these tumors 13,14.
Clinical presentation
Patients typically present with a smooth, painless, enlarging mass.
Pathology
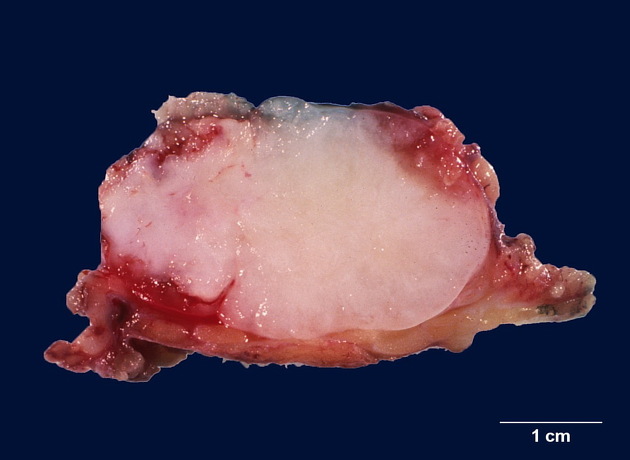
As the name suggests, pleomorphic adenomas are composed of a mixture of variable histology. They contain both epithelial and myoepithelial (mesenchymal) tissues, with mixed histology. They appear encapsulated and well-circumscribed however the pseudocapsule is delicate and incomplete with microscopic extensions reaching beyond it, accounting for the high risk of recurrence when these tumors are enucleated (see below) 5,6.
The gross appearance depends upon the relative proportion of epithelial elements and a stromal component which may range from myxoid to cartilage. Tumors with a prominent cartilaginous matrix have a bluish-grey opalescent appearance.
Three histological types have been described:
myxoid (hypocellular): most common, highest rate of recurrence
cellular
classic
Location
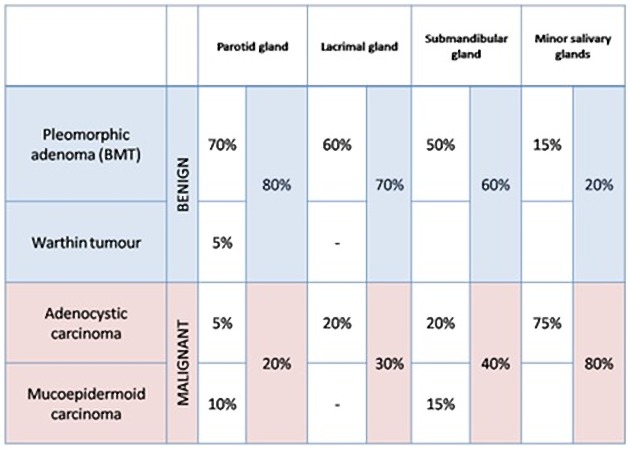
Distribution among the salivary glands is as follows 1:
-
parotid gland: 84% 1
commoner in the superficial lobe
submandibular gland: 8%
-
minor salivary glands: 6.5%
widely distributed including the nasal cavity, pharynx, larynx, trachea 5
sublingual glands: 0.5%
They are less common in salivary glands other than the parotid but remain the most common benign tumor of each gland.
Pleomorphic adenomas are also commonly found in the lacrimal glands where they account for approximately 50% of lacrimal gland tumors 7.
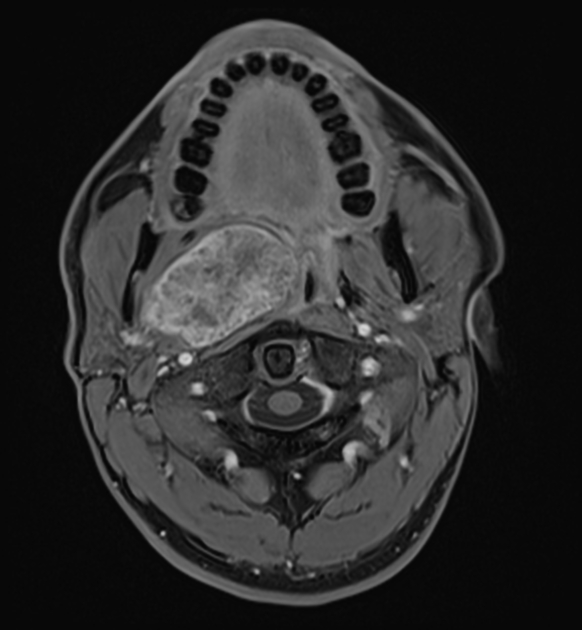
Radiographic features
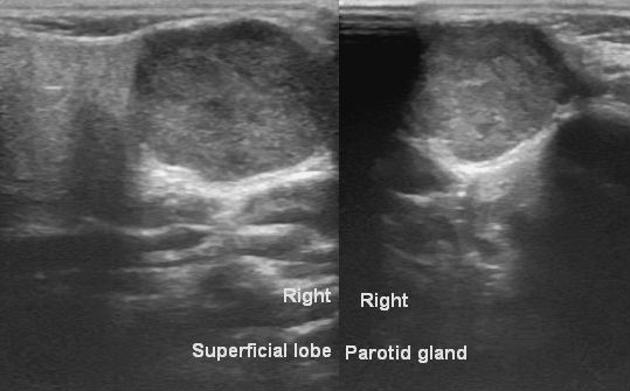
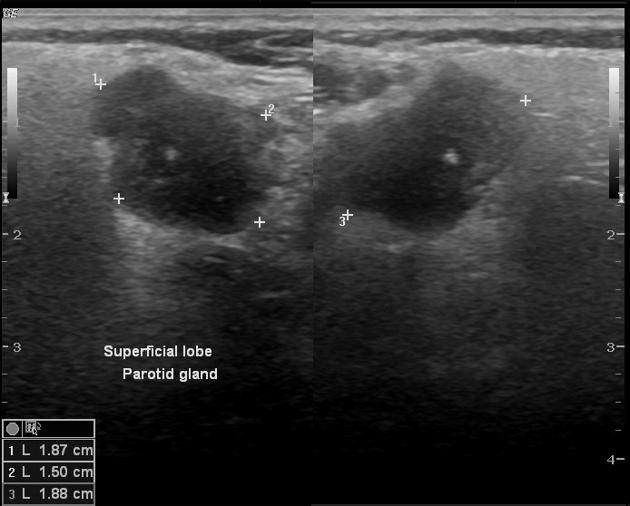
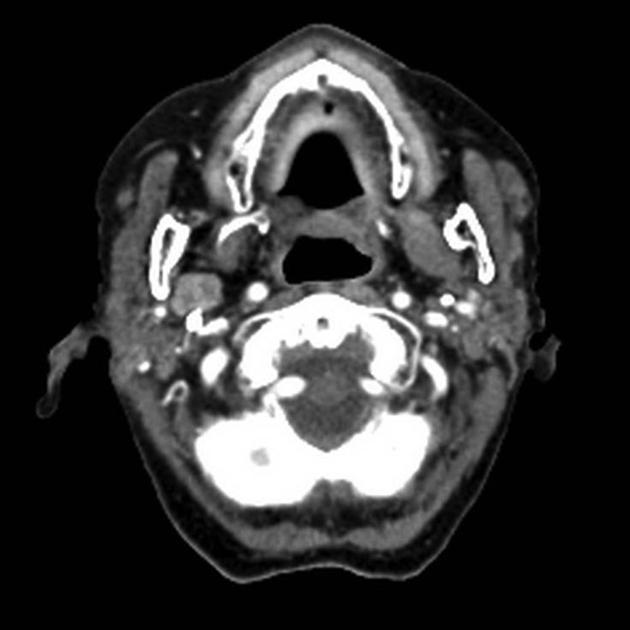
On all modalities, these tumors typically appear as rounded masses with well-defined, "bosselated" or "polylobulated" borders (many small undulations, not truly lobulated). They are most commonly located within the parotid gland, particularly the superficial lobe.
When they arise from the deep lobe of the parotid they can appear entirely extra parotid, seen in the prestyloid parapharyngeal space, without a fat plane between it and the parotid, and widen the stylomandibular tunnel. Pleomorphic adenomas can also arise from salivary rest cells in the parapharyngeal space itself without connection to the parotid gland.
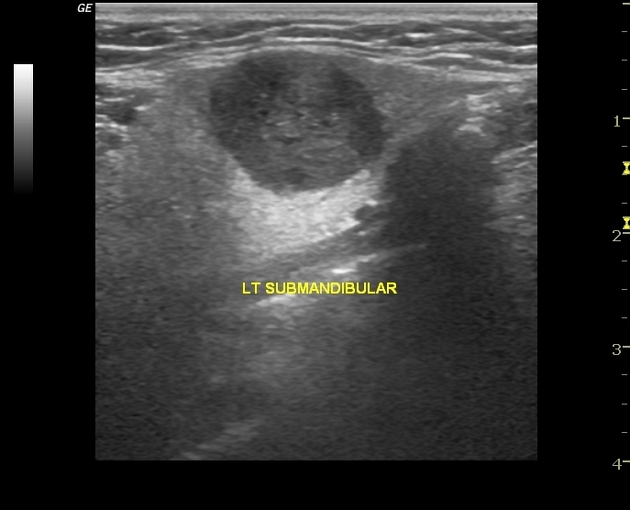
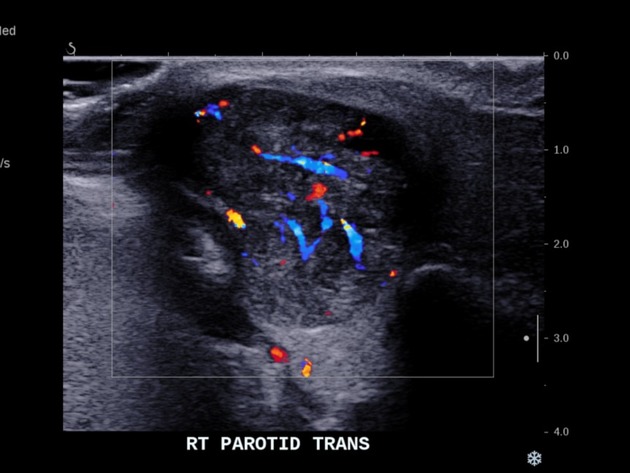
Ultrasound
They are typically hypoechoic and may show posterior acoustic enhancement.
Ultrasound is also useful in guiding a biopsy (both FNAC and core biopsies) but needs to be carried out with care to avoid facial nerve damage 8,9.
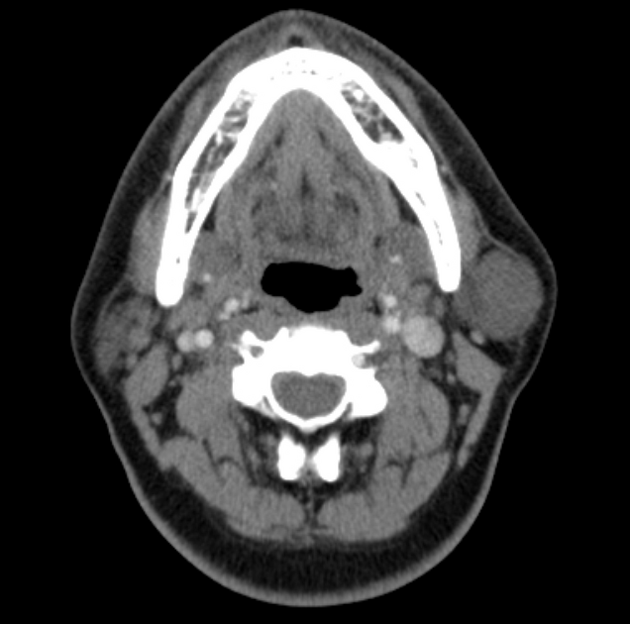
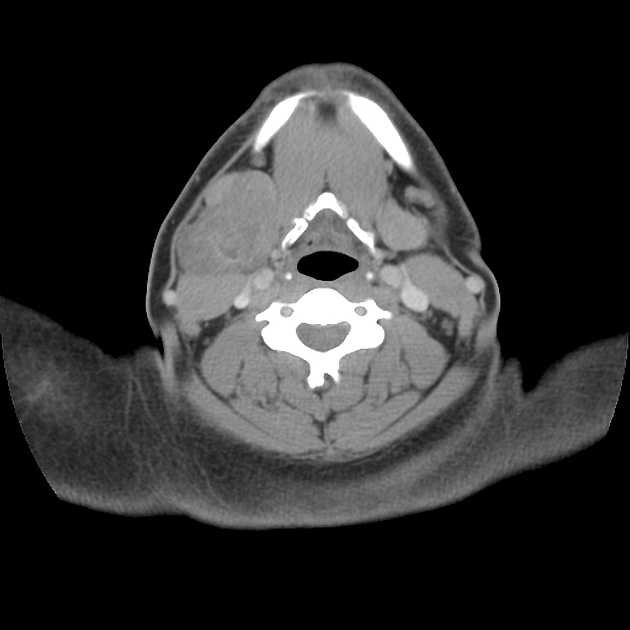
CT
When small, they have homogeneous attenuation and prominent enhancement. When larger, they can be heterogeneous with less prominent enhancement, foci of necrosis, and possible delayed enhancement. Small regions of calcification are common 1,10.
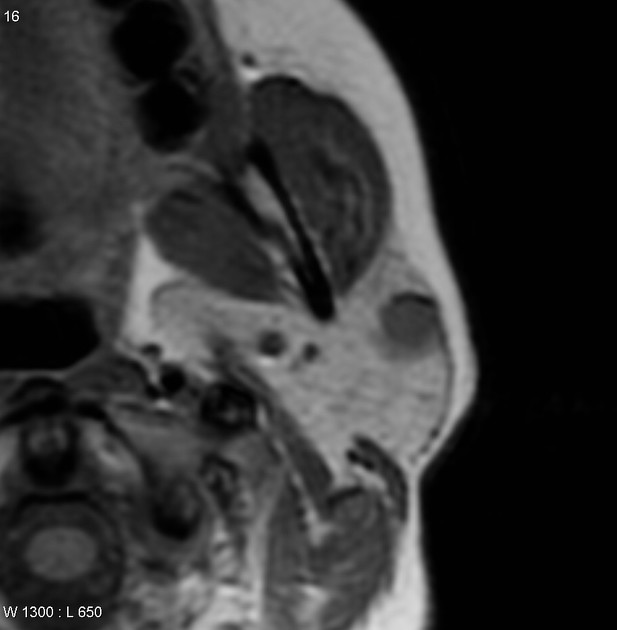
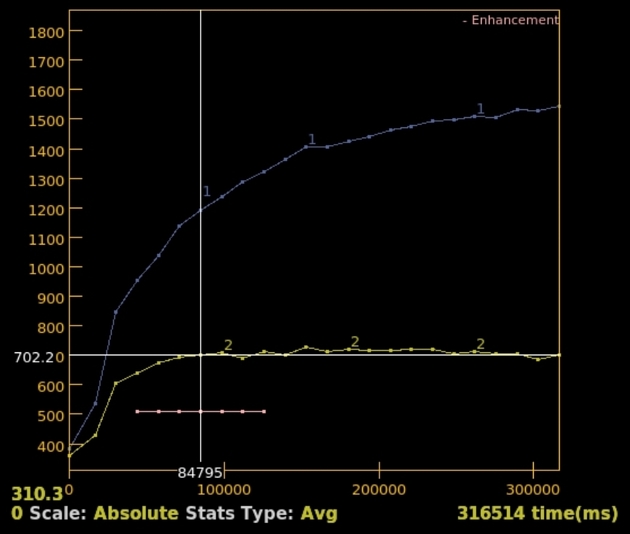
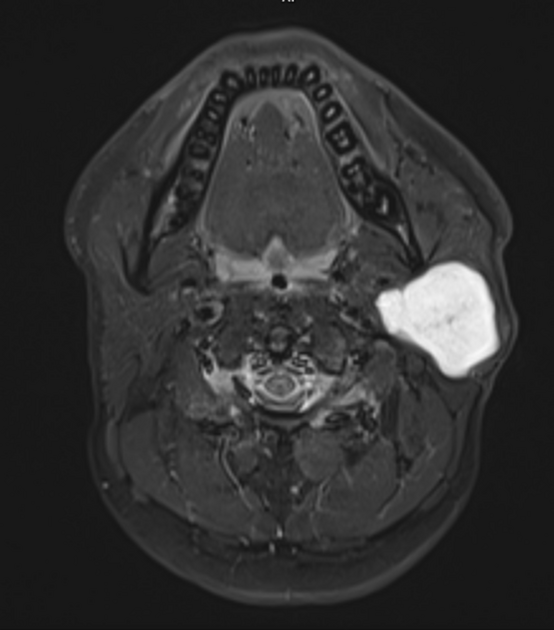
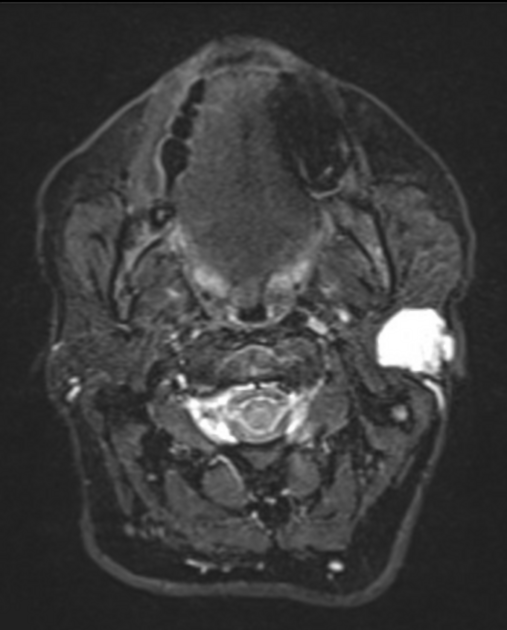
MRI
The signal characteristics are homogeneous when the tumor is small. Larger tumors may be heterogeneous.
T1: usually of low intensity
-
T2
characteristically of very high intensity (especially myxoid type) 6
often have a rim of decreased signal intensity on T2-weighted images representing the surrounding fibrous capsule
T1 C+ (Gd): usually demonstrates homogeneous enhancement
Angiography (DSA)
typically hypovascular
Nuclear medicine
FDG-PET may show some uptake; SUV more than 3 in 25% of cases 11.
Treatment and prognosis
Surgical excision is curative, however, as the tumor is poorly encapsulated (despite imaging suggesting otherwise) there is a significant rate of recurrence in the tumor bed. Exact rates of recurrence vary widely depending on series and surgical technique (1-50%) 1.
Historically these tumors were removed by enucleation, resulting in recurrence rates of 20-45% 6.
To minimize recurrence, open surgical biopsy should not be performed. Rather, a partial (superficial) or total parotidectomy ensures a wide margin. The facial nerve should be spared 4,6. Using this approach, the recurrence rate has reduced dramatically to 1-4% 6.
Percutaneous ultrasound biopsy (both FNAC and core biopsy) can be performed safely and is associated with very low tumor seeding rates and without facial nerve injury provided meticulous technique is used 8,9.
When in the minor salivary glands, a 5 mm margin should be obtained. These tumors do not invade into periosteum, thus bone need not be resected 4.
When tumor bed recurrences occur, they can be extremely difficult to control, with management options including monitoring only, surgery, or radiotherapy.
Complications
There is a small risk of malignant transformation into a carcinoma ex-pleomorphic adenoma which is proportional to the time the lesion is in situ (1.5% in the first 5 years, 9.5% after 15 years), thus excision is recommended in essentially all cases. Additional risk factors for malignancy include advanced age, large size, radiation therapy, and recurrent tumors 2,6. In addition to carcinoma ex-pleomorphic adenoma, true malignant mixed tumors of the salivary glands usually arise from pre-existing pleomorphic adenomas 1,3. Metastasizing pleomorphic adenoma is the third type of malignant mixed tumor of salivary glands and is the rarest. It presents with metastases to lung, bone, and soft tissues despite having 'benign' histology 1.
Differential diagnosis
When in the parotid gland consider:























 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.