Cerebellar hemorrhages are a common form of intracerebral hemorrhage (ICH) and usually occur due to poorly controlled long-standing hypertension, although other causes also exist. When due to chronic hypertension, the stigmata of chronic hypertensive encephalopathy are often present (see: cerebral microhemorrhage).
There are many causes of cerebellar hemorrhage, this article is focused on primary cerebellar hemorrhages.
On this page:
Epidemiology
The demographics of affected patients usually reflect those of patients with long-term poorly controlled hypertension, and as such patients are usually middle-aged to elderly (>5th decade) 6. Cerebellar hemorrhages account for ~10% of all intracerebral hemorrhages and ~15% of cerebellar strokes 3,9.
Clinical presentation
Clinical presentation depends on the size of the hemorrhage. Small cerebellar hemorrhages can present with typical "posterior circulation symptoms" of vertigo, ataxia, nausea, vomiting and headache. These can be sudden onset and occur during exercise or stress situations 6. Larger hemorrhages can present with reduced consciousness 6.
Pathology
Cerebellar hemorrhage can be due to 6:
hypertension (most common): most commonly located deep/centrally at the dentate nuclei
underlying lesion, e.g. tumor, arteriovenous malformation, intracranial aneurysm, dural arteriovenous fistula
cerebral amyloid angiopathy: can be suggested when the hemorrhage is solely located superficially/peripherally at the cerebellar cortex and/or vermis 7
supratentorial surgery (see: remote cerebellar hemorrhage)
Radiographic features
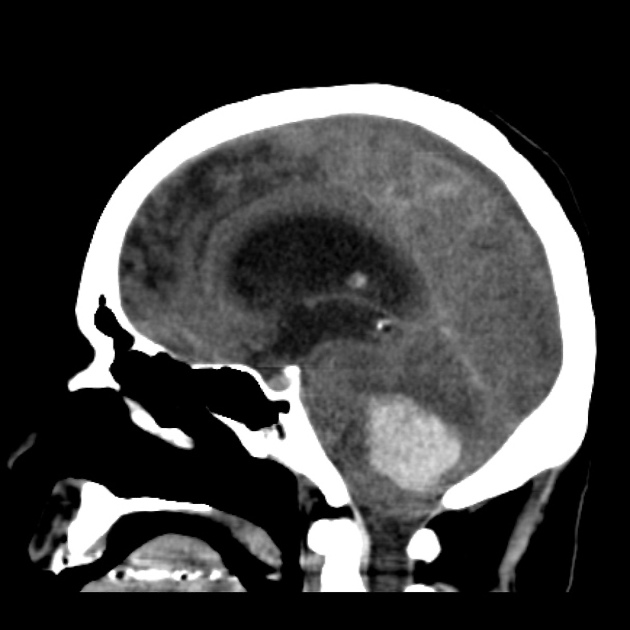
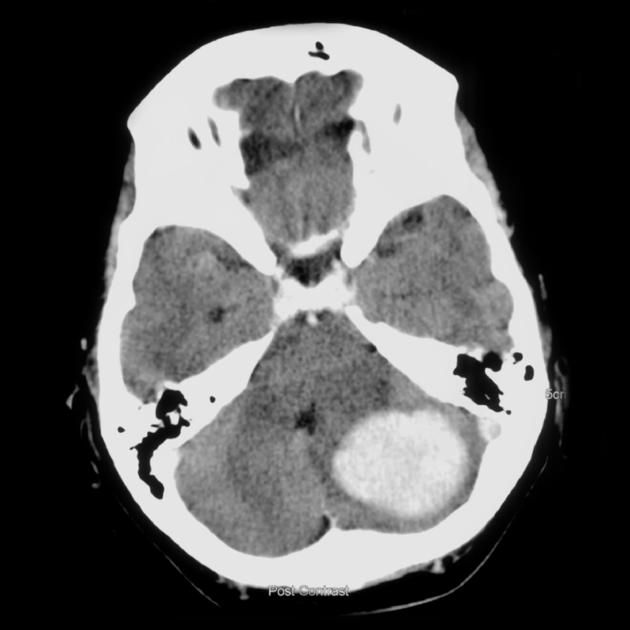
CT is usually the first, and often the only, imaging investigation obtained. Serial imaging may be required to evaluate for hematoma expansion, posterior cranial fossa mass effect and/or the development of hydrocephalus 10.
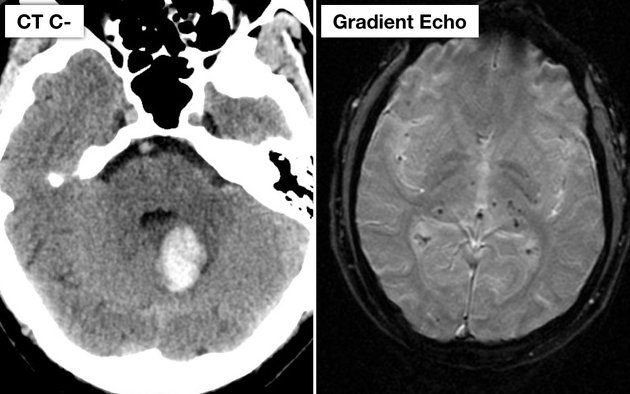
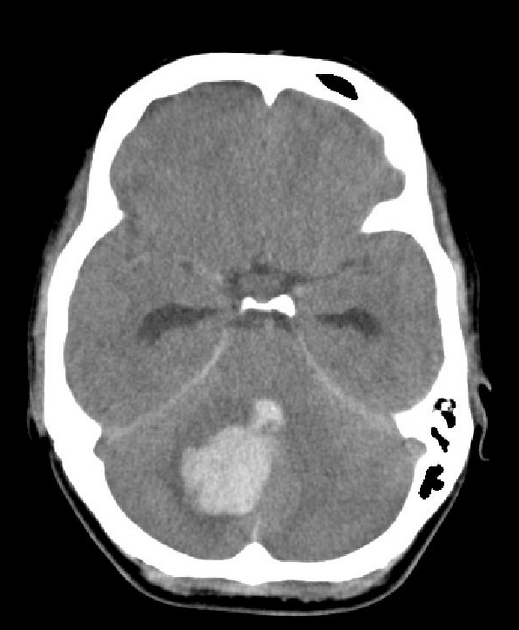
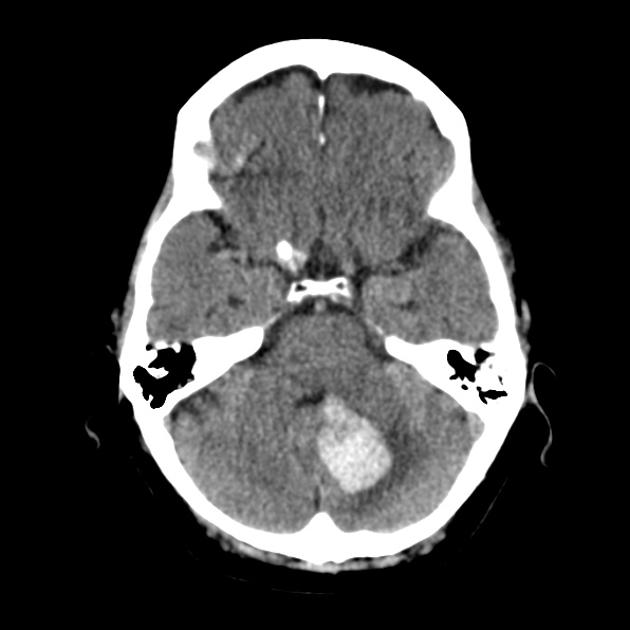
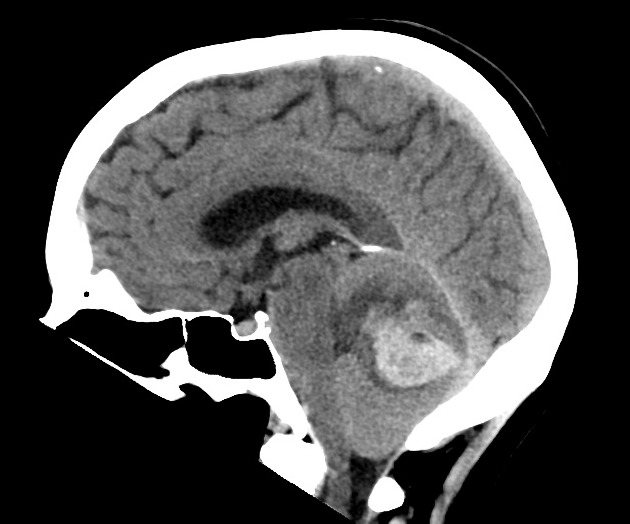
CT
As with other acute intracranial hemorrhages, cerebellar hemorrhages appear as regions of hyperdensity within the cerebellar hemispheres. Extension into the fourth ventricle or subarachnoid space is relatively common 9.
If there is no extension into the ventricular system, the volume of the hemorrhage can be estimated using ABC/2 8, which may have treatment implications.
There are many predictors of hematoma expansion potentially evident on CT, which are discussed in depth in the main intracerebral hemorrhage article.
MRI
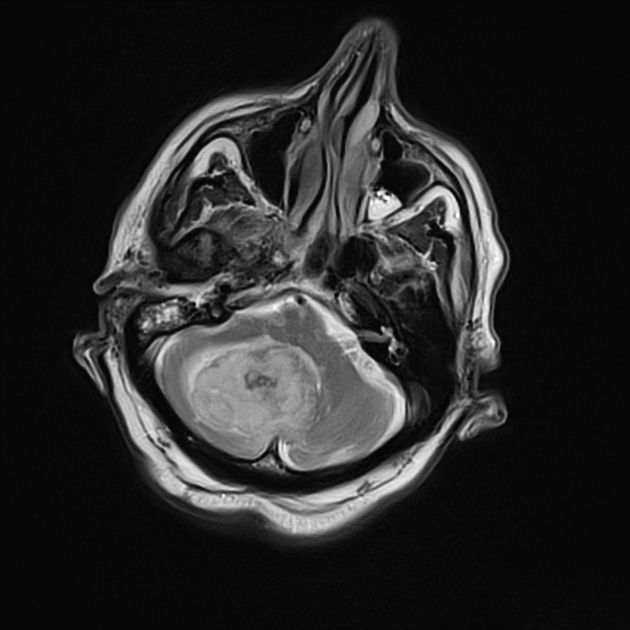
The appearance of hemorrhage on MRI varies with time and to some degree the size of the hematoma (see aging blood on MRI).
Treatment and prognosis
Overall, medical management does not differ for other causes of intracerebral hemorrhage - please see the article on intracerebral hemorrhage for further discussion 11.
In contrast to management of intracerebral hemorrhages in other locations, neurosurgical intervention is more common in cerebellar hemorrhages. Cerebellar hemorrhages are often complicated by hydrocephalus, brainstem compression, and/or cerebellar herniation, and thus surgical hematoma evacuation via craniotomy +/- extraventricular drain (if needed for hydrocephalus) is often recommended despite the absence of high-level evidence 11. These interventions are thought to reduce mortality compared to non-surgical treatment although may not improve functional outcomes 8,11. Indications for evacuation include 8,11:
neurological deterioration
brainstem compression
obstructive hydrocephalus
cerebellar hemorrhage volume ≥15 mL










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.