Endovascular clot retrieval (ECR), also known as mechanical thrombectomy (MT) or endovascular thrombectomy (EVT), is increasingly performed in patients presenting with large vessel occlusion (LVO), especially those with a large ischemic penumbra that is likely to progress to ischemic stroke. To be successful, careful patient selection and dedicated training and equipment are necessary.
On this page:
History
ECR and its efficacy in ischemic stroke have been explored since 2005, initial trials revealed disappointing results. This was attributed to an inability to confirm large vessel occlusions radiologically combined with insufficiently developed devices and treatment delays 18. In 2015, multiple randomized controlled trials were published showing improved clinical outcomes in patients with acute ischemic stroke due to large vessel occlusion undergoing ECR compared to medical (conservative) treatment alone 3-5. As a result of these trials, ECR has now become the standard of care for large vessel occlusion strokes involving the anterior circulation.
Patient selection
-
acute ischemic stroke due to large vessel occlusion in the anterior circulation
robust evidence to support use within 6 hours of symptom onset 24
growing evidence to support use beyond 6 hours 6,13, including up to 24 hours and in patients with large ischemic core volumes 20,21,28
acute ischemic stroke due to large vessel occlusion in the posterior circulation remains an area of uncertainty and selection (c.2024) is dependent on clinician judgment in accordance with local guidelines, although there are several positive randomized clinical trials supporting its use 22,23
acute ischemic stroke due to medium vessel occlusion (MeVO) have had negative trials, such that endovascular clot retrieval was not found to be superior to best medical therapy 30,31, although local institutional practice may vary
Contraindications
intracranial hemorrhage on initial non-contrast CT
-
large infarct core with no significant penumbra (i.e. no salvageable brain)
note that large infarct cores by themselves may not be a contraindication, with two randomized clinical trials utilizing core volumes of >50 mL 20,21
various patient factors (e.g. premorbid functional status, advanced directives, etc.)
Procedure
Preprocedural evaluation
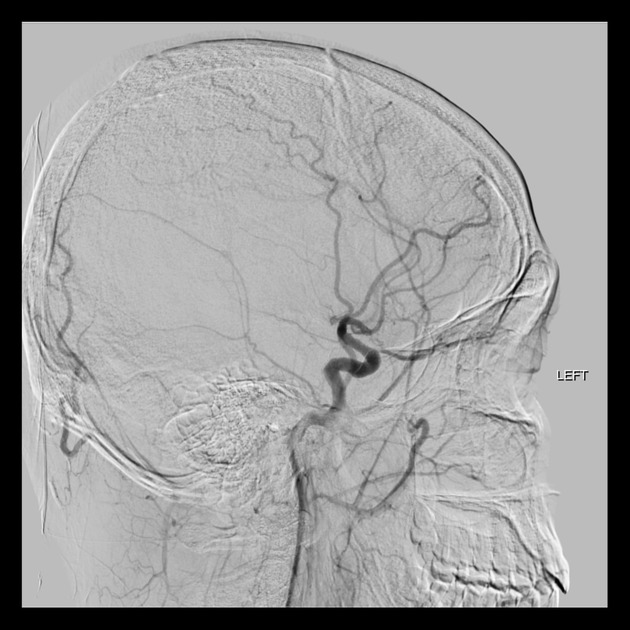
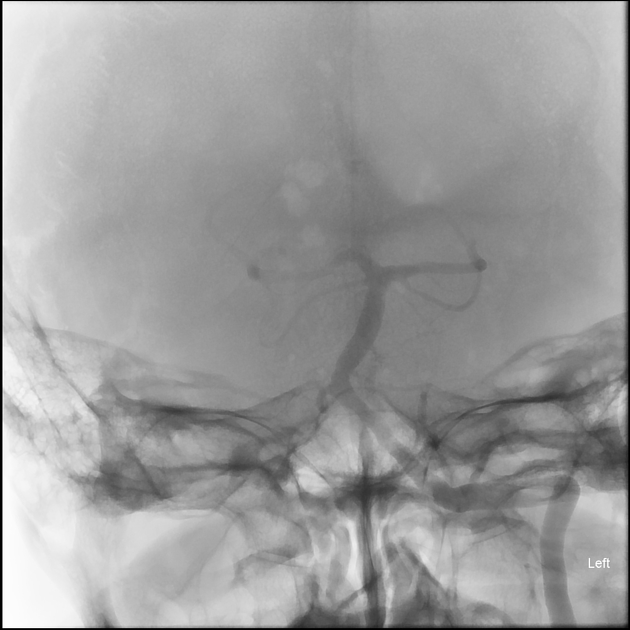
Non-contrast enhanced CT is used to exclude hemorrhage and CT angiography to determine large vessel occlusion. Alternatively, MRI and DSA may also demonstrate the occlusion although the former is less commonly utilized for this due to difficulty with timely access to MRI in most institutions. CT perfusion is also important to determine the infarct core and penumbra size, especially in cases performed beyond 6 hours 6,13,20,21.
Angiographic imaging can also:
assess collateral vessels which contribute to predicting outcome in some settings 8
assess the thrombus occlusion pattern (e.g. presence of the clot meniscus sign, a tapered appearance suggestive of underlying intracranial atherosclerotic disease, a cut-off appearance, a tram-track appearance) 26
Positioning/room set up
Equipment
stent retrievers
aspiration devices
balloon guiding catheter
microcatheters
Technique
Postprocedural care
Although successful technical clot retrieval is essential, appropriate postprocedure care is also critical to avoid complications.
Blood pressure control
Avoiding excessively high blood pressure is important in reducing the risk of secondary hemorrhage. In the acute post-ECR/thrombolysis period a target BP <185/110 mmHg is recommended 14, however, intensive blood pressure lowering (e.g. to <140 mmHg systolic) may be harmful 27.
If critical carotid stenosis (i.e. tandem lesion) has been treated then more aggressive blood pressure control may be warranted to avoid the possibility of cerebral hyperperfusion as well as hemorrhage 16. There are, however, few universally agreed-upon guidelines and chosen targets will vary according to pre-procedure blood pressure, anticoagulation, pre-ECR thrombolysis, size of the expected infarct and a variety of other factors.
Puncture site
Groin site neurovascular observations and bed rest are required as usual. There is an increased move towards radial artery access for lower complication rates 17.
Anticoagulation
In a variety of settings, anticoagulation may need to be restarted shortly after clot retrieval (e.g. antiplatelet agents for stenting, anticoagulation for atrial fibrillation). The timing of this is on a case by case balance and involves balancing the risk of thromboembolic complications from delaying anticoagulation versus the increased risk of a cerebral hemorrhage.
Complications
The overall complication rate is about 15% 1. Complications include 2,9,29:
-
intracranial hemorrhage (<8%)
parenchymal (5%)
emboli to new territories
vessel perforation (1-5%)
vasospasm
-
vascular access site complications
groin hematoma (2-11%)
retroperitoneal hematoma (<6%)
orbital infarction syndrome (1-2%)
mortality
Outcomes
The technical outcome is graded using the mTICI score. ECR is a highly effective treatment for ischemic strokes affecting the anterior circulation, with a number needed to treat (NTT) of 2.6 for an improved functional outcome. In a meta-analysis of anterior circulation ECR performed within 6 hours, 46% of patients treated with ECR achieved functional independence (modified Rankin scale (mRS) 0–2 at 90 days) compared to 27% for best medical treatment 2. Outcomes of ECR in posterior circulation strokes are mixed, with trials demonstrating both positive and negative functional outcomes compared to best medical therapy 19,22,23.








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.