Esophageal carcinoma is globally the 7th most common cancer and 6th most common cause of cancer-related death as per NCCN version 3.2023. It tends to present with increasing dysphagia, initially to solids and progressing to liquids as the tumor increases in size, obstructing the lumen of the esophagus.
On this page:
Epidemiology
Esophageal cancer is responsible for <1% of all cancers and 4-10% of all gastrointestinal malignancies. There is recognized male preponderance with the squamous cell subtype, M:F 4:1.
The incidence of the subtypes has regional variation. The squamous cell subtype has the greatest worldwide incidence (~90%), but the adenocarcinoma subtype is more common in many parts of North America and Europe. In addition, there are certain regions where individuals are at particularly high risk of developing esophageal cancer, e.g. Iran, Malawi, Zimbabwe, Mongolia, Italy, and China.
Predisposing factors include 8:
alcohol and smoking: for squamous cell carcinoma and adenocarcinoma
Barrett esophagus: for adenocarcinoma
caustic stricture/lye stricture
obesity: for adenocarcinoma
history of oral or pharyngeal cancer
human papillomavirus (HPV)
tylosis (Howel–Evans syndrome): a rare autosomal dominant disease with hyperkeratosis of the palms and soles with a high incidence of esophageal squamous cell carcinoma
Bloom syndrome: rare autosomal recessive disorder consisting of hematological malignancies Wilms tumor and solid tumors, including that of the esophagus
Fanconi anemia: a rare autosomal recessive disorder characterized by hematological malignancies, pancytopenia, congenital malformations and solid tumors (such as that of the esophagus)
Clinical presentation
Patients present with progressive dysphagia, weight loss, chronic worsening gastro-esophageal reflux and hoarseness, cough, vocal cord paralysis, or other signs and symptoms of mediastinal invasion.
Pathology
Histological types
squamous cell carcinoma of the esophagus: 81-95% (worldwide)
-
adenocarcinoma of the esophagus: 4-19% (worldwide)
arising from mucosal/submucosal glands, heterotopic gastric mucosa, or columnar-lined epithelium
>90% related to Barrett esophagus
tend to occur at the gastro-esophageal junction
-
other types
* in the western world, adenocarcinoma is as common or even slightly more common than squamous cell carcinoma
Macroscopic appearance
-
polypoid/fungating (most common)
sessile/pedunculated tumor
lobulated surface protruding
irregular, polycyclic, overhanging, step-like "apple core" lesion
ulcerating: large ulcer niche within a bulging mass
infiltrating: gradual narrowing with a smooth transition
superficial spreading carcinoma
Staging
See the separate articles by histology:
esophageal and esophagogastric junction adenocarcinoma (staging)
esophageal and esophagogastric junction squamous cell carcinoma (staging)
esophageal and esophagogastric junction neuroendocrine tumor (staging)
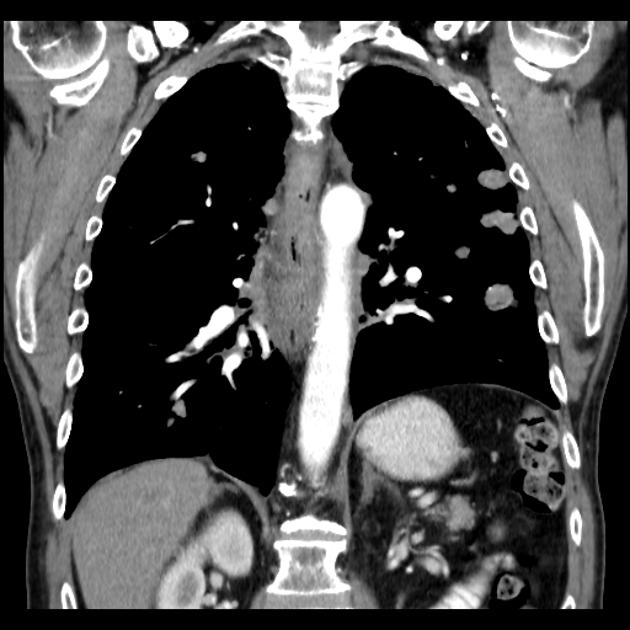
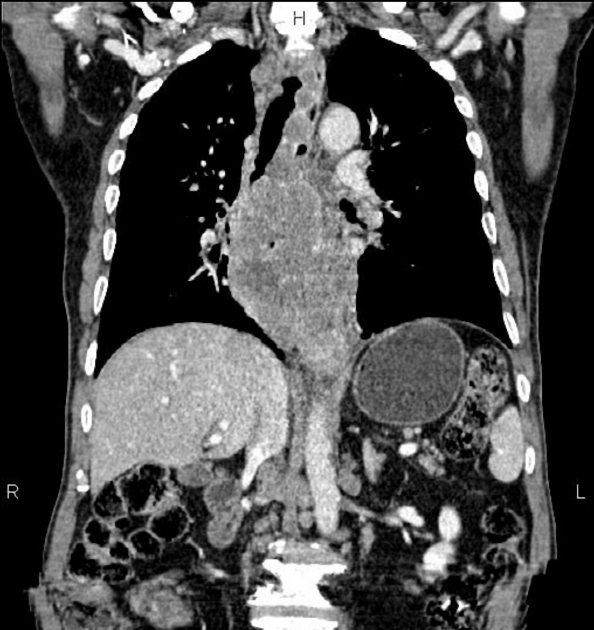
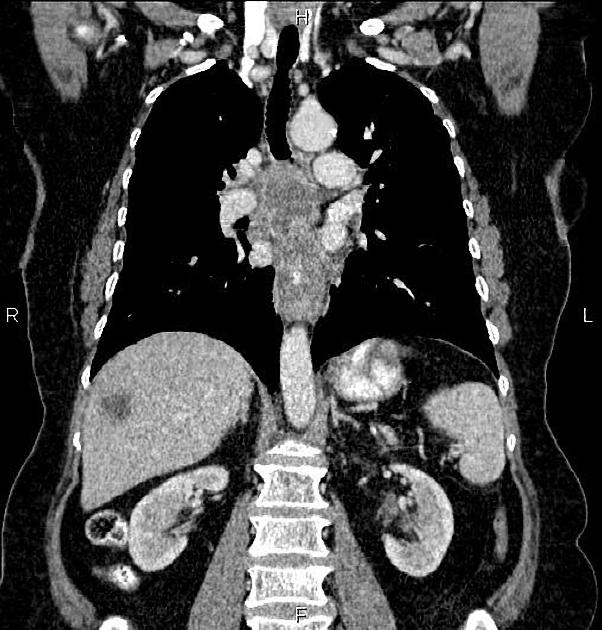
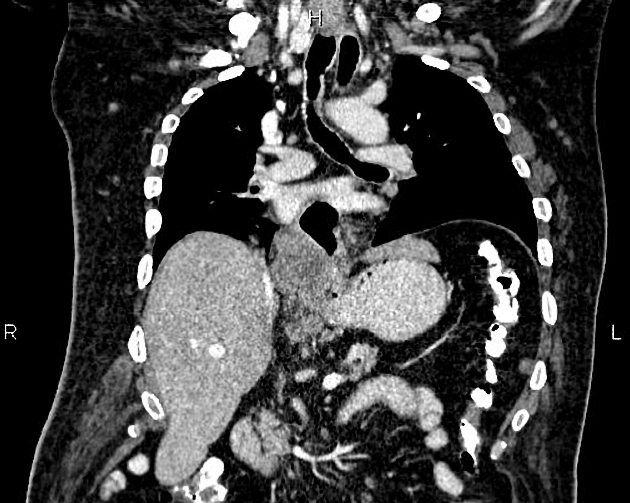
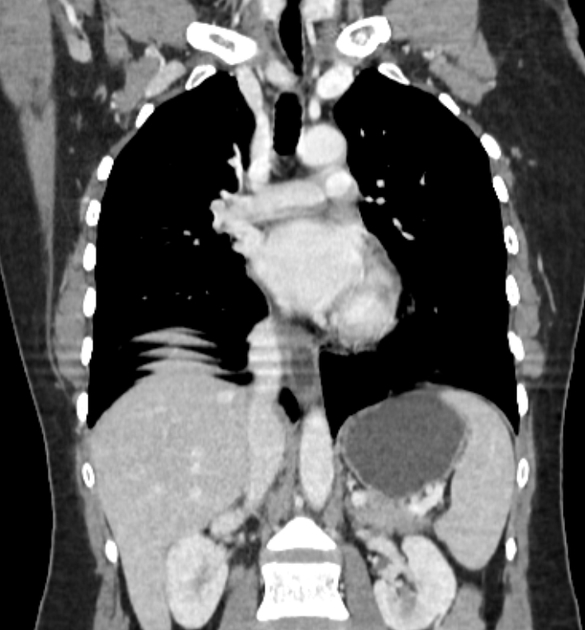
Metastases
-
lymphatic
anterior jugular chain and supraclavicular nodes (primary in upper 1/3)
para-esophageal and subdiaphragmatic nodes (primary in middle 1/3)
mediastinal and paracardiac and celiac trunk nodes (primary in lower 1/3)
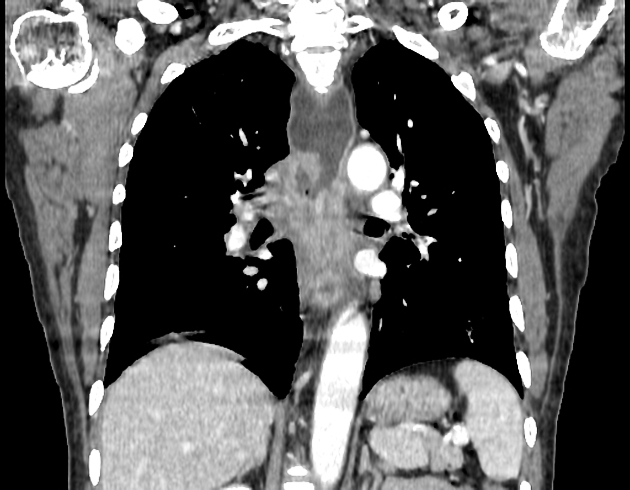
hematogenous: lung, liver, adrenal glands
Radiographic features
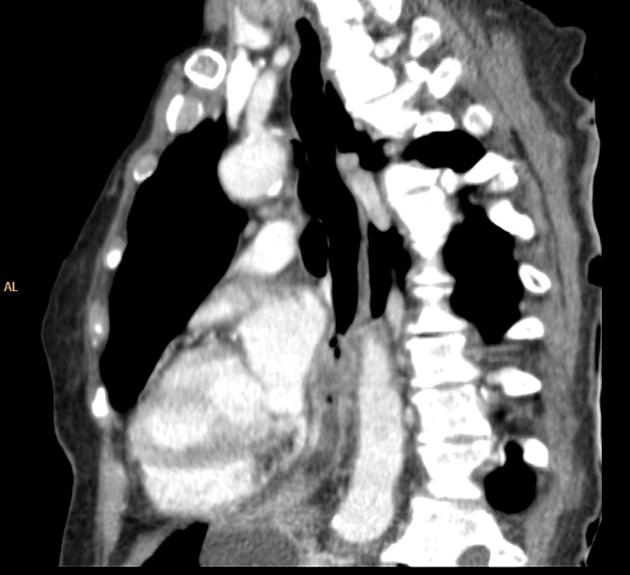
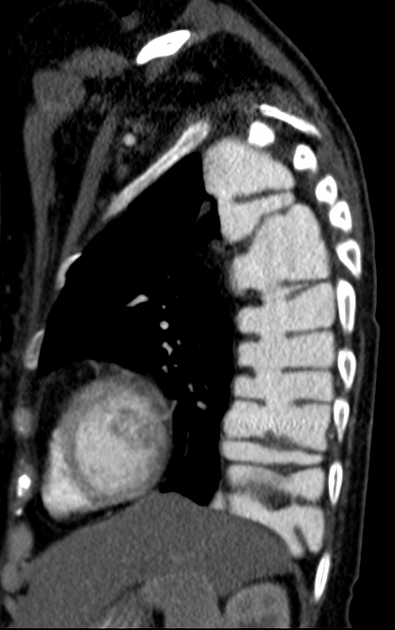
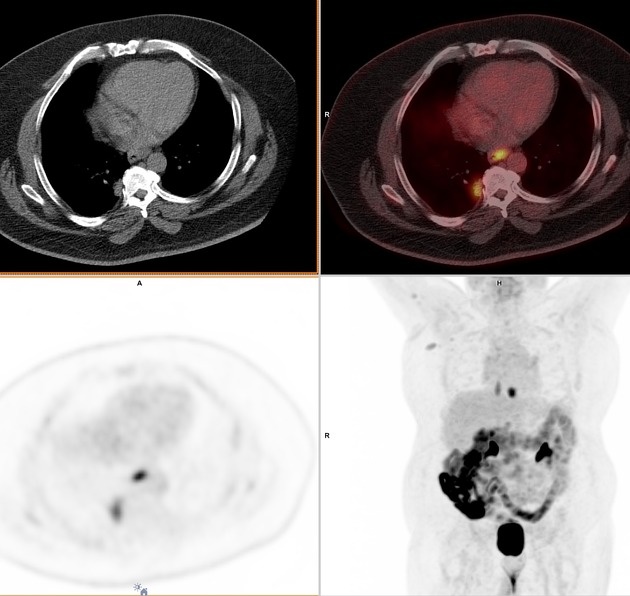
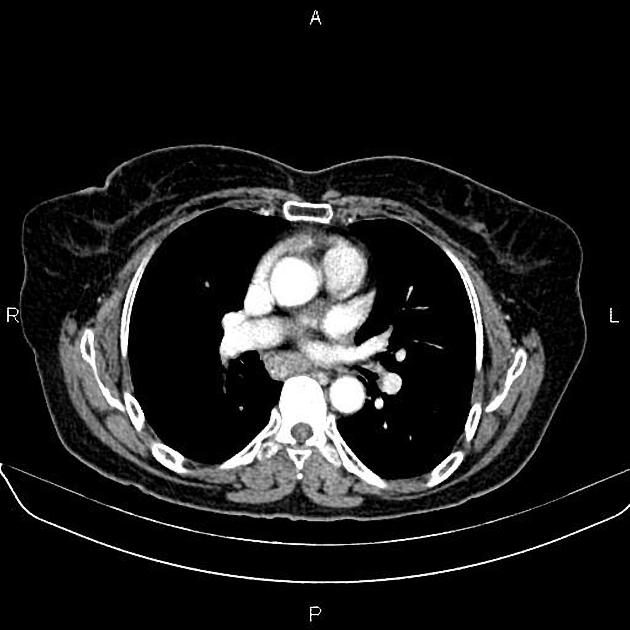
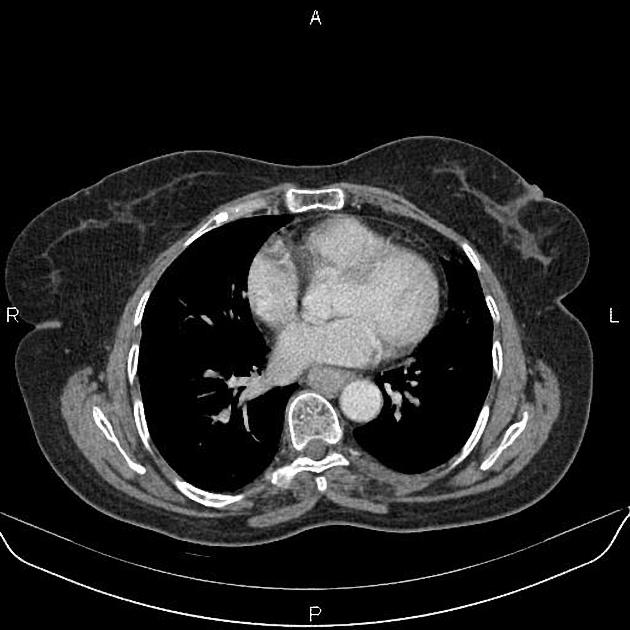
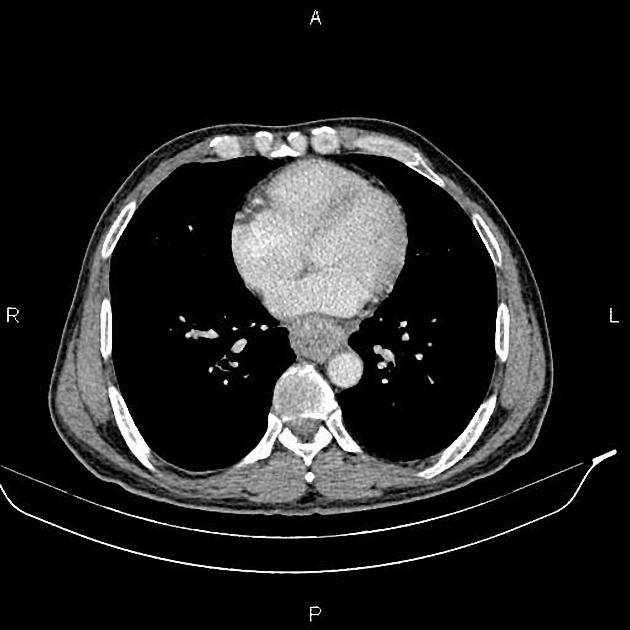
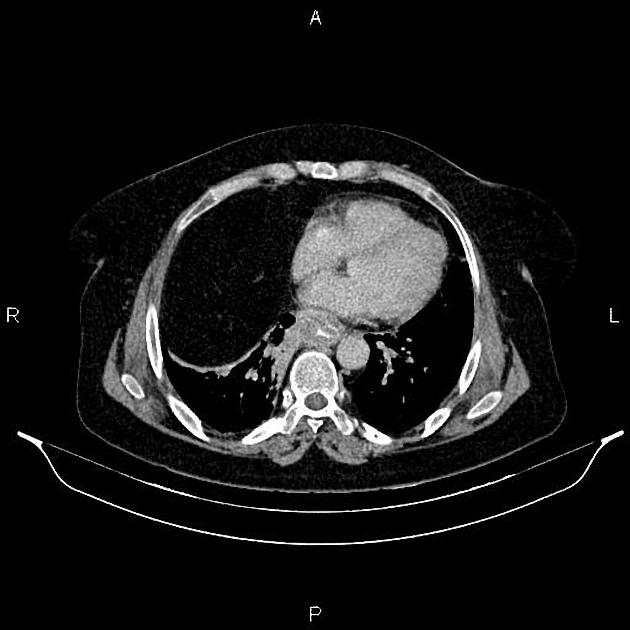
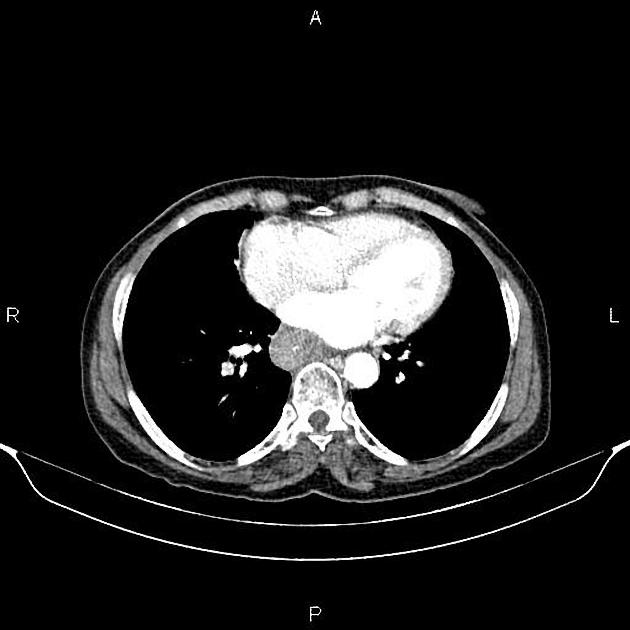
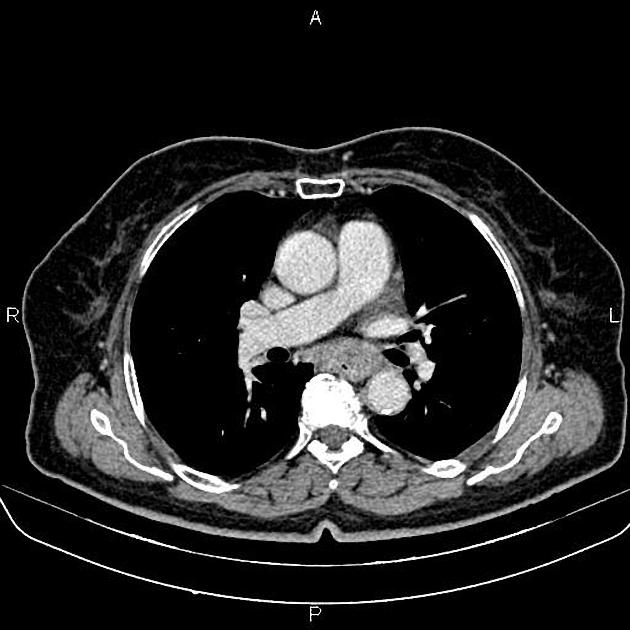
A combination of CT scan, transesophageal ultrasound, and PET-CT is used to stage the disease. CT is the best initial modality for detecting distant metastasis, gross direct invasion, and enlarged lymph nodes. Ultrasound is the most sensitive modality for assessment of the depth of invasion and regional enlarged lymph nodes. PET can be useful for restaging after the initial neoadjuvant therapy 7.
Plain radiograph
Chest radiograph
Many indirect signs can be sought on a chest radiograph, and these include:
widened azygos-esophageal recess with convexity toward the right lung (in 30% of distal and mid-esophageal cancers)
thickening of posterior tracheal stripe and right paratracheal stripe >4 mm (if tumor located in the upper third of esophagus)
tracheal deviation or posterior tracheal indentation/mass
retrocardiac or posterior mediastinal mass
esophageal gas-fluid level
lobulated mass extending into a gastric bubble (Kirklin sign)
repeated aspiration pneumonia (with tracheo-esophageal fistula)
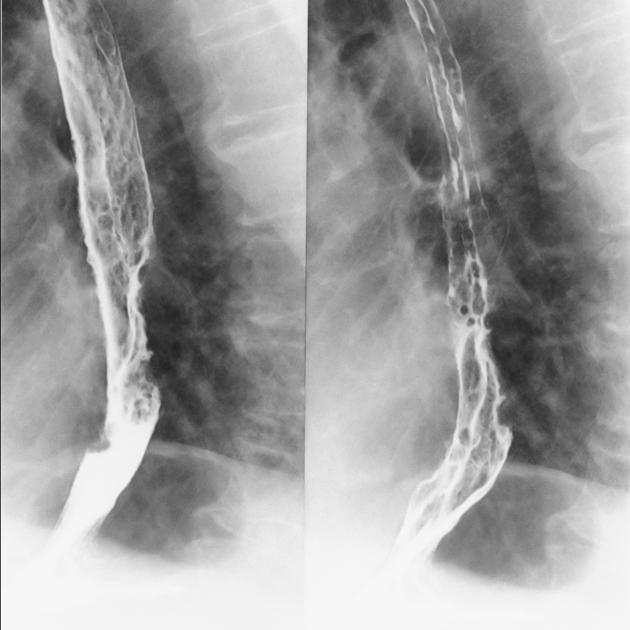
Fluoroscopy
Contrast swallow
irregular stricture
prestricture dilatation with 'hold up'
shouldering of the stricture
US
Endoscopic ultrasound
The most accurate imaging modality for the T staging of esophageal cancer. It defines the layers of the esophageal wall hence can differentiate T1, T2, and T3 tumors.
The esophagus consists of five layers:
first hyperechoic layer represents the interface between the balloon and the superficial mucosa
second hypoechoic layer represents the lamina propria and muscularis mucosae
a third hyperechoic layer represents the submucosa
fourth hypoechoic layer represents the muscularis propria
fifth layer represents the interface between the adventitia and surrounding tissues
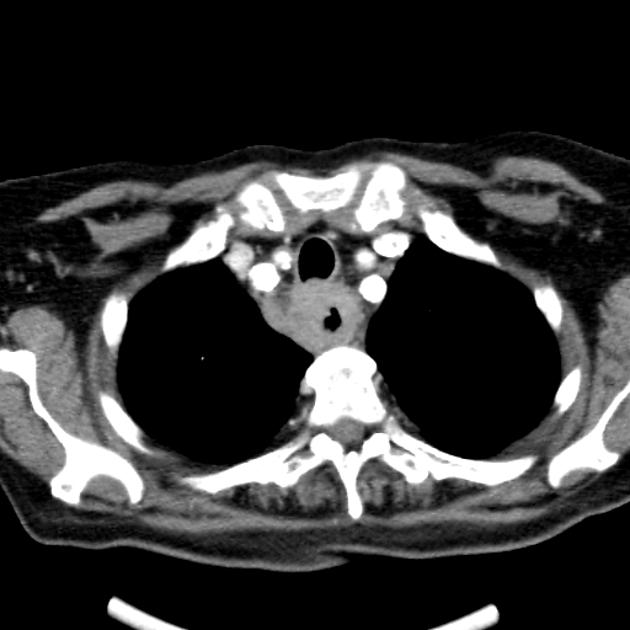
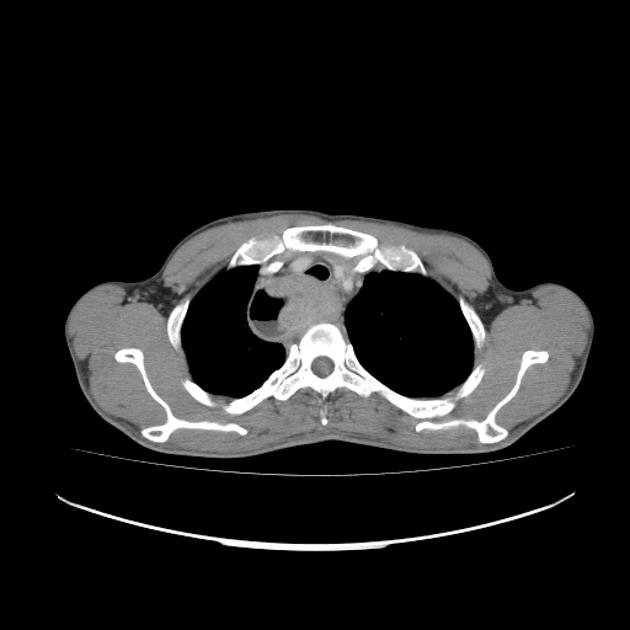
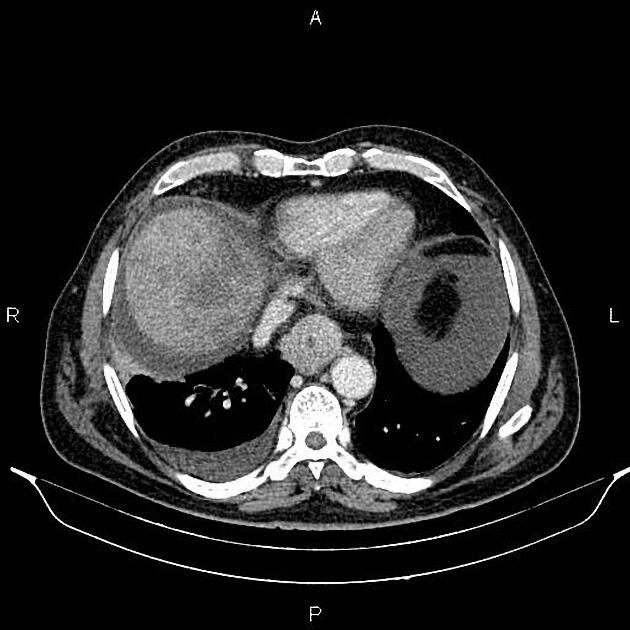
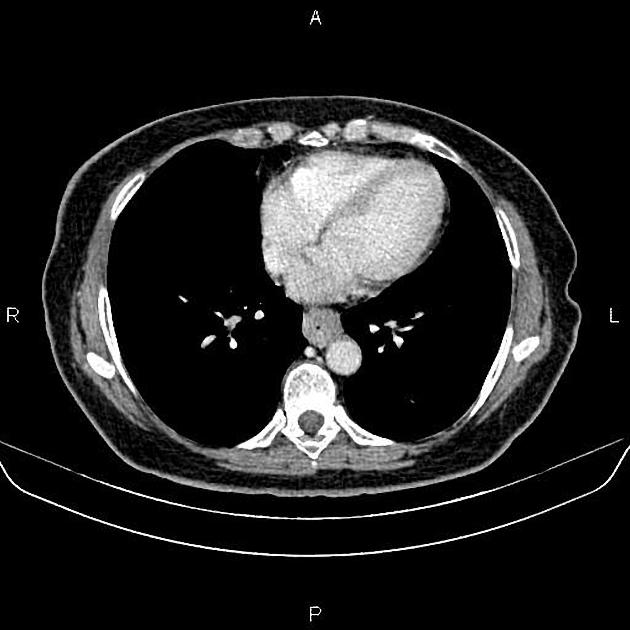
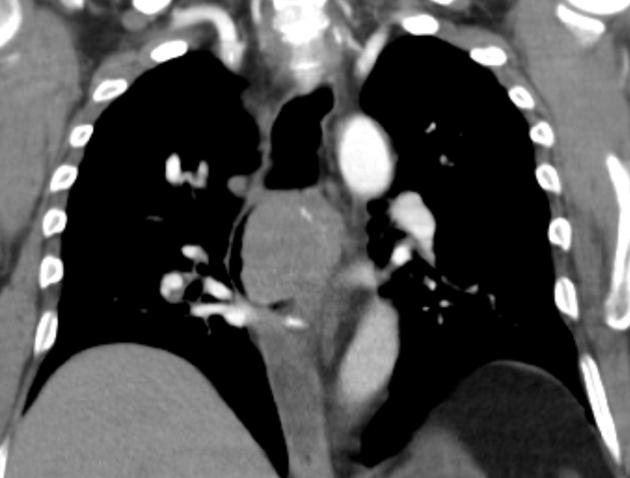
CT
eccentric or circumferential wall thickening >5 mm
periesophageal soft tissue and fat stranding
dilated fluid- and debris-filled esophageal lumen is proximal to an obstructing lesion
tracheobronchial invasion appears as a displacement of the airway (usually the trachea or left mainstem bronchus) as a result of the mass effect by the esophageal tumor
aortic invasion
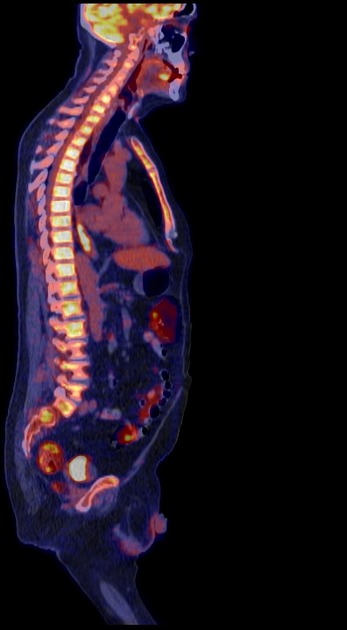
PET-CT
FDG PET-CT is useful for detecting esophageal primary tumors. Yet, it has little role in helping determine the specific T classification because it provides limited information about the depth of tumor invasion.
PET-CT is also superior to CT for detecting lymph node metastases and can depict metastases in normal-sized lymph nodes through the uptake of FDG.
PET-CT has a primary role in depicting distant sites of metastatic disease.
The bones and liver are the most common sites of distant metastases detected at PET (but frequently missed at CT).
Treatment and prognosis
The 5-year mortality depends on the stage of the tumor. Unfortunately, most cases present with regional or distant metastatic disease (30% and 40%, respectively).
localized disease: ~40% 5-year survival
distant metastatic disease: ~5% 5-year survival
Endoscopic mucosal resection, without or with localized ablation, is an option for localized (T1a) disease. These epithelial tumors are usually <2 cm, asymptomatic, and noncircumferential.
For T1b tumors and above, surgical options are mostly limited to esophagectomy (including sometimes with palliative colonic interposition (see case 19)).
Complications
fistula formation to the trachea (5-10%), bronchi or mediastinum: can be either due to direct tumor progression or iatrogenic effects (e.g. radiation therapy)
Differential diagnosis
Imaging differential considerations include:
-
benign tumors of the esophagus
non-malignant conditions (e.g. diffuse inflammation)


































 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.