Lacunar infarcts (LACI) are small (<15 mm) infarcts in the distal distribution of deep penetrating vessels (lenticulostriate, thalamoperforating, and pontine perforating arteries, recurrent artery of Heubner). They result from occlusion of one of the small penetrating end arteries at the base of the brain and have traditionally been thought to occur due to fibrinoid degeneration. However, there is debate in the literature as to whether the etiology of lacunar infarction also includes embolism 5.
On this page:
Clinical presentation
Most lacunar infarcts are clinically silent, but repeated episodes are associated with vascular dementia. Symptomatic patients may present with lacunar stroke syndrome, one of five distinct syndromes.
Pathology
Lacunar infarcts, by definition, are caused by occlusion of small penetrating end-arteries and must be smaller than 15 mm. They are mostly thought to result from in situ microatheroma formation or lipohyalinosis 2. When this occurs at the origin of a penetrating artery, this is known as branch atheromatous disease 7. Additionally, lacunar infarcts can also be described as being caused by embolism 5. Indeed, some argue that it is important to investigate lacunar infarction for underlying embolism even though this may only be present in a minority of patients 6.
Pathologically, lacunar infarcts are small holes of encephalomalacia and are traversed by a cobweb-like mesh of fibrous strands.
Radiographic features
CT
In the acute setting, lacunar infarcts appear as ill-defined hypodensities.
Chronic lesions appear as hypodense foci, similar density to CSF.
MRI
In an acute setting, the following signal changes are seen:
T1: slightly hypointense
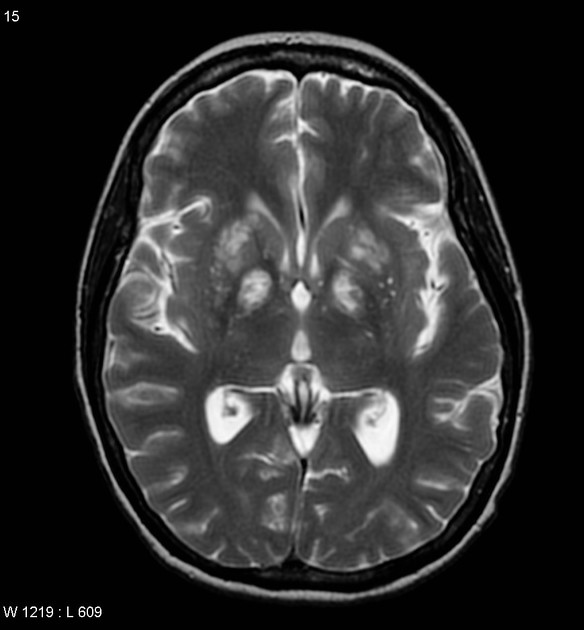
T2/FLAIR: hyperintense
-
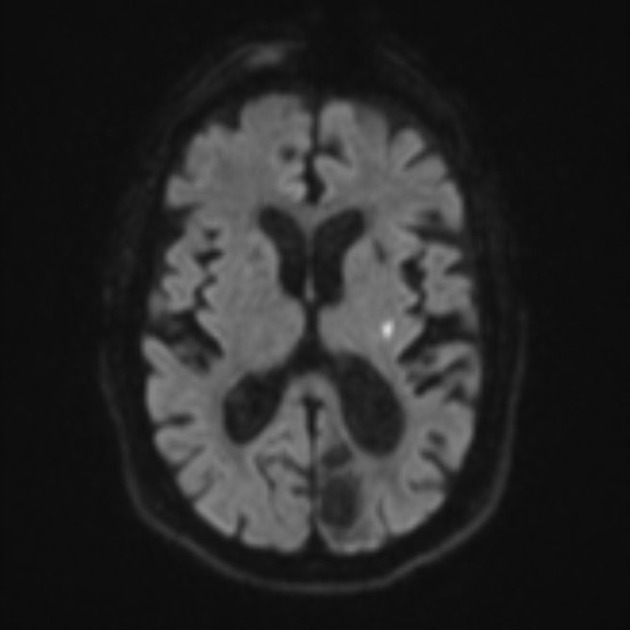
DWI: restricted diffusion
may demonstrate acute lesions not visible on other sequences
T1 C+ (Gd): may enhance if acute (or early subacute)
Chronic lesions are isointense to CSF on all sequences but may demonstrate a peripheral T2/FLAIR hyperintense rim of marginal gliosis.
History and etymology
The term was penned by Charles Miller Fisher (1913-2012) 4, a Canadian neurologist, who described "lacunes" (Latin: lake) of empty fluid within the brains of stroke victims post-mortem.












 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.