Fat necrosis within the breast is a pathological process that occurs when there is saponification of local fat. It is a benign inflammatory process and is becoming increasingly common with the greater use of breast-conserving surgery and mammoplasty procedures.
On this page:
Epidemiology
Most at risk are middle-aged women with pendulous breasts. The onset of fat necrosis can be considerably delayed, occurring 10 years or more after surgery 3.
Pathology
At the microscopic level, the initial change is the disruption of fat cells, with the formation of vacuoles containing the remnants of necrotic fat cells. The vacuoles are then surrounded by lipid-laden macrophages, multinucleated giant cells, and acute inflammatory cells. Fibrosis develops during the reparative phase, peripherally enclosing an area of necrotic fat and cellular debris. Eventually, fibrosis may replace the area of degenerated fat with a scar, or loculated and degenerated fat may persist for years within a fibrotic scar.
Etiology
-
direct trauma, e.g. from a seat belt, breast biopsy, implant removal, prior augmentation, reduction or reconstruction, radiation therapy, direct silicone injection 8.
in everyday practice, trauma and surgery are the most common causes
no history of trauma or surgery in 35-50% of cases 8
When there is calcification within the cyst wall, it is termed liponecrosis macrocystica calcificans.
Location
predilection for the subareolar and periareolar regions
edges of TRAM flap reconstruction where blood supply is more difficult 8
Radiographic features
Mammography
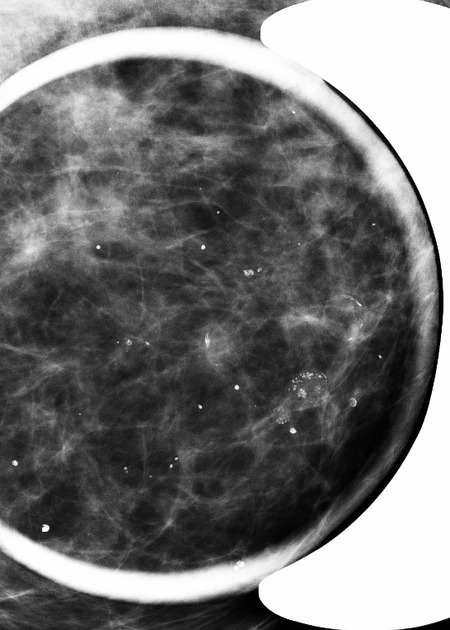
Fat necrosis can have a very variable, sometimes alarming appearance on mammography and is often potentially confusing to the novice breast imager. Initially, it can be seen as an ill-defined and irregular, spiculated mass-like area. Associated calcification can be present, which can mimic that of more malignant entities such as DCIS.
Note that fat necrosis of the breast can change in time with progressive calcification, so comparison with previous imaging is essential. Also, the changes can often be seen and correlated with the position of surgical scarring on the breast itself (refer to the technologist sheet).
The calcification of fat necrosis is typically peripheral with a stippled curvilinear appearance creating the appearance of lucent "bubbles" in the breast parenchyma. Note the low-density centers. Tumor formation is not a part of fat necrosis although it may be clinically palpable.
With time, it becomes more defined and well-circumscribed giving rise to an oil cyst. Oil cysts can have very fine curvilinear calcification of the walls. The center of the lesion becomes increasingly homogeneous with fat density. The cyst wall calcifies in ~5%.
Breast ultrasound
Acute phase (within days): increased echogenicity due to edema of the fatty tissue.
Subacute phase (days to months): ill-defined complex cystic lesion (uni or multiloculated with low-level echoes) surrounded by edematous fat.
Late phase (1.5 years or more): calcified walls and as a consequence posterior shadowing. If postsurgical etiology can present as angular margin or spiculated mass with an echogenic rim 8.
The identification of the subtle wall nodularity in an oil cyst is a dead giveaway but takes effort and real-time imaging. Ultrasound of fat necrosis should always be interpreted in the context of mammographic findings.
Aspiration of an oil cyst shows typically a milky, emulsified fat appearance. In the sample bottle, the fat globules can be seen drifting on the cytology before they disperse. This is the typical appearance and is immediately recognisable.
Differential diagnosis
On ultrasound, the lesion may occasionally represent an intracystic carcinoma and mammographic correlation is recommended in these circumstances 1. The key to diagnosis is the history, the tech sheet and review of multiple cases. Other differentials include lipoma, fibroadenolipoma and galactocele 8.











 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.