Graves disease, also known as Basedow disease in mainland Europe 9, is an autoimmune thyroid disease and is the most common cause of hyperthyroidism.
On this page:
Epidemiology
There is a strong female predilection (F:M = 5:1), and is most common between 30 and 60 years 14. The incidence is 20 per 100,000 people 14.
Pediatric Graves disease accounts for 5% of all cases (incidence 5 per 100,000 children). It is more common in older adolescents. Children have a lower female prediction (F:M = 3.5:1) 15.
Associations
There is a 10x increased relative risk of the following autoimmune diseases 16:
rheumatoid arthritis (the most common co-existing autoimmune disorder)
vitiligo
Clinical presentation
Patients are thyrotoxic with common symptoms being tremor, heat sensitivity, unexplained weight loss, anxiety, goiter, etc. 14. Extrathyroidal manifestations include:
Graves ophthalmopathy (orbitopathy): affects 20-25% of cases
thyroid dermopathy (formerly called pretibial myxedema): occurs in ~2% and is almost always associated with thyroid ophthalmopathy 7
thyroid acropachy: occurs in ~1% 7
encephalopathy associated with autoimmune thyroid disease (EAATD) 2,8: much more commonly associated with Hashimoto thyroiditis
The combination of exophthalmos, palpitations, and goiter is called the Merseburger (or Merseburg) triad.
Pathology
Graves disease results from an antibody-directed stimulation of the thyroid-stimulating hormone (TSH) receptor, with the production and release of T3 and T4, resulting in hyperthyroidism 14.
Etiology
The pathogenesis of Graves disease is not fully known 15. Genetic predisposition accounts for 80% of the risk of Graves disease, with environmental factors (e.g. smoking, iodine excess, selenium deficiency, vitamin D deficiency) accounting for the rest 14.
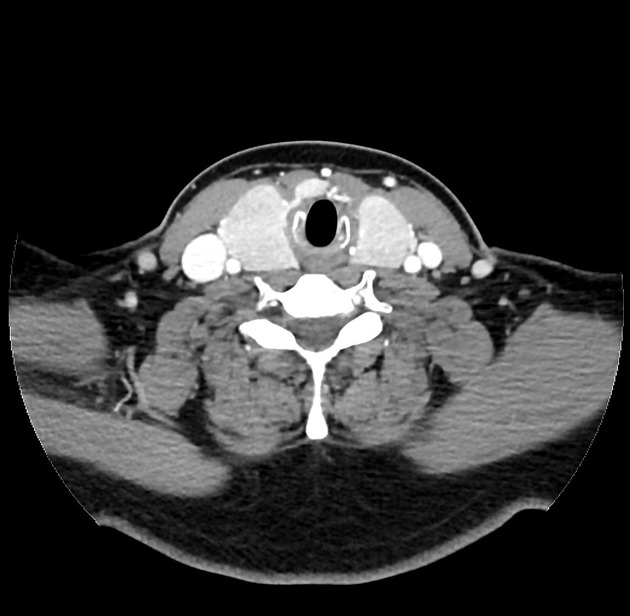
Macroscopic appearance
The affected gland shows diffuse, symmetrical enlargement, with a fleshy red cut surface. This appearance can be altered by preoperative treatment or chronicity.
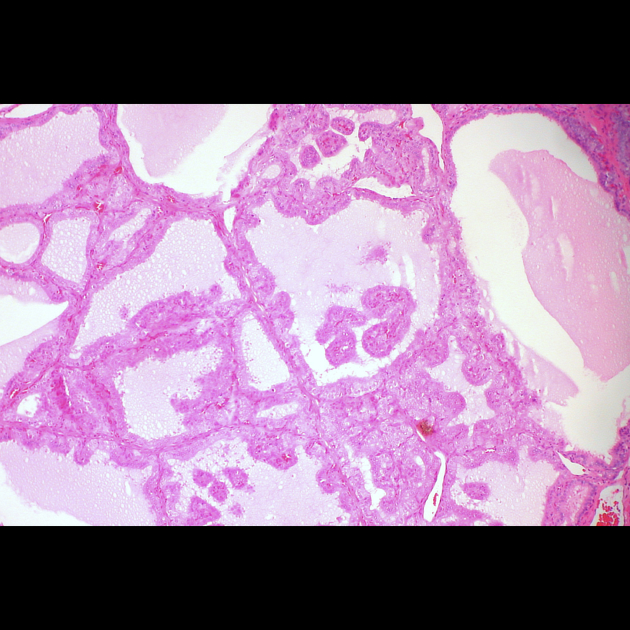
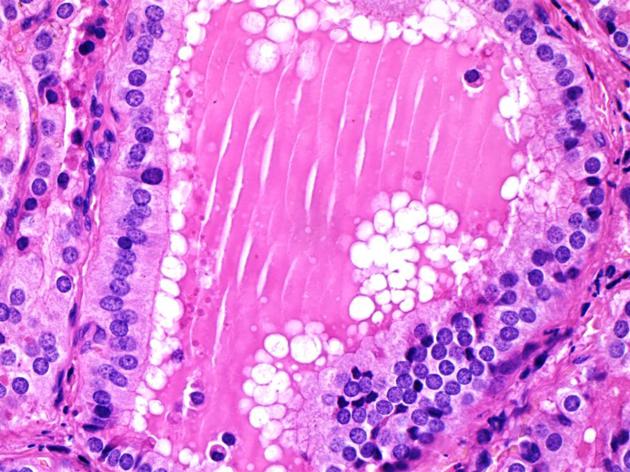
Microscopic appearance
The histological features are consistent with the activated state of the gland:
plump follicular cells with increased amounts of eosinophilic cytoplasm
hyperplastic follicles with papillary epithelial infoldings
evidence of colloid reabsorption, including "scalloping" at the apical membrane and variable follicle collapse and exhaustion
These features can be altered by preoperative treatment or chronicity.
Markers
TSH: suppressed
T4: elevated
T3: elevated
TSH receptor antibodies (TSI, TGI, TBII): positive
Radiographic features
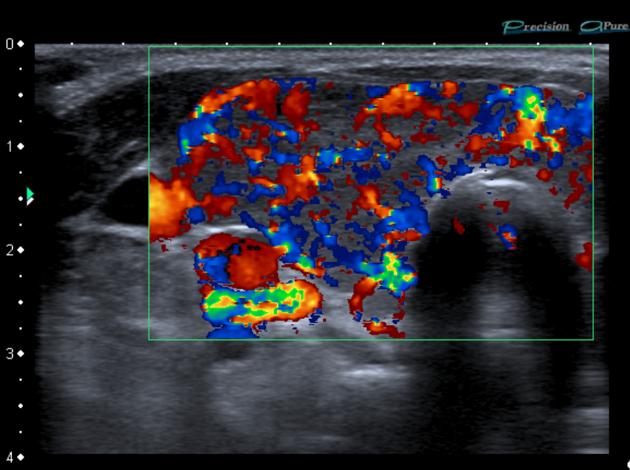
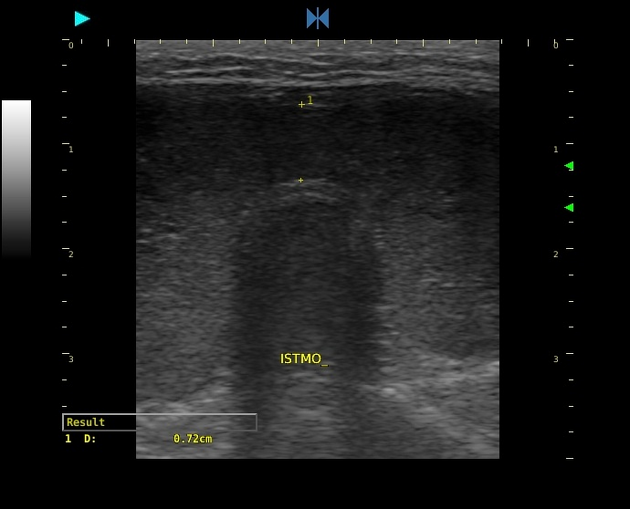
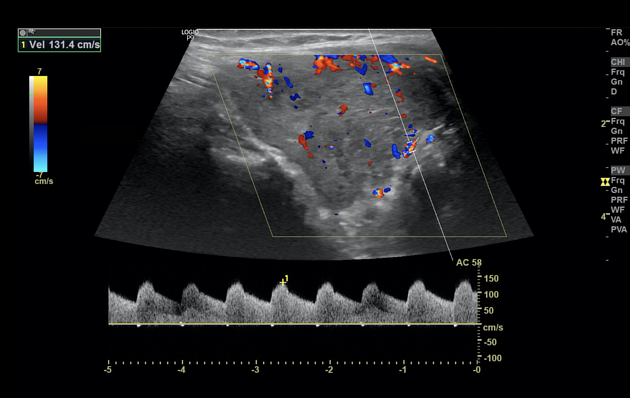
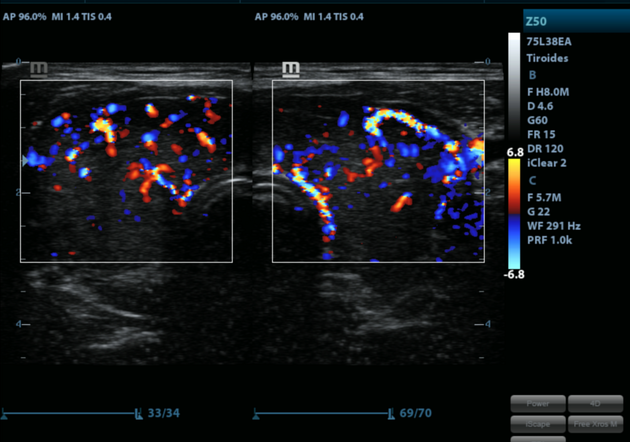
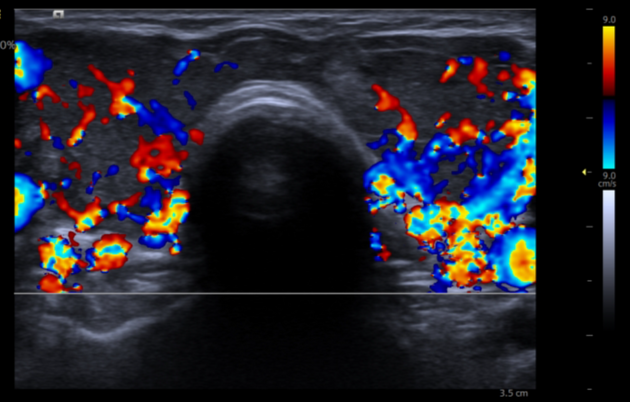
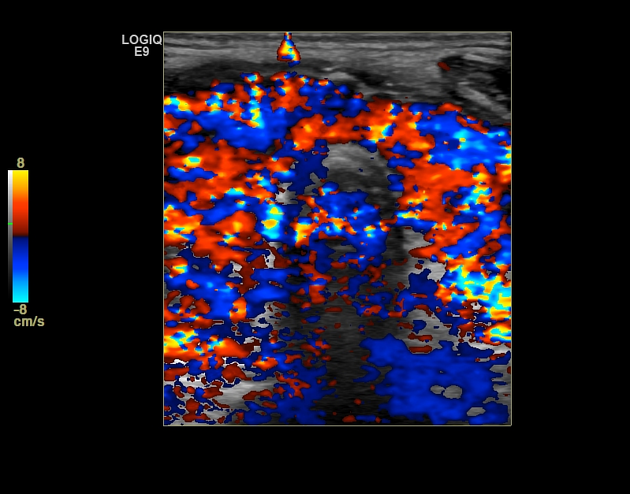
Ultrasound
the thyroid gland is often enlarged and can be hypoechoic
heterogeneous thyroid echotexture
relative absence of nodularity in uncomplicated cases
hypervascular; may demonstrate a thyroid inferno pattern on color Doppler 1
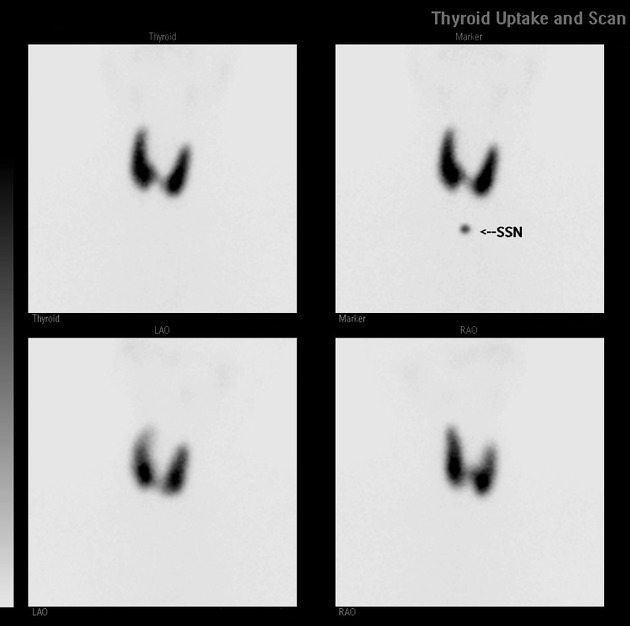
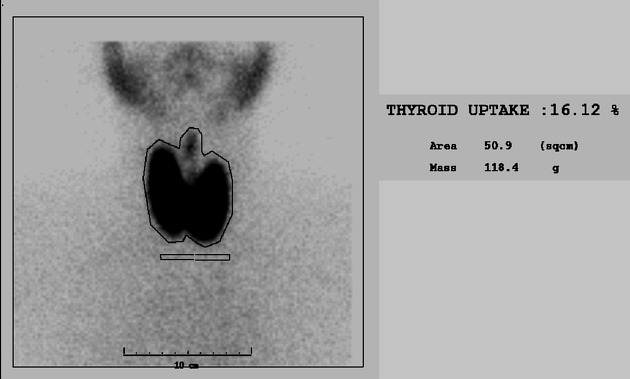
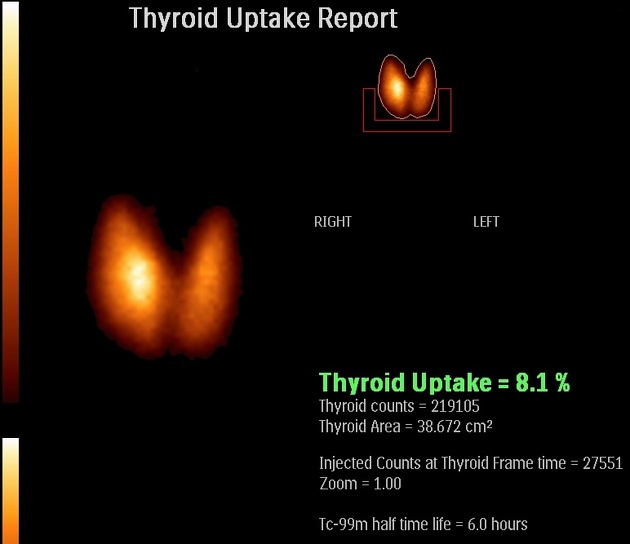
Nuclear medicine
iodine-123: imaging performed at around 2-6 days; classically demonstrates homogeneously increased activity in an enlarged gland
technetium-99m pertechnetate: homogeneously increased activity in an enlarged thyroid gland
Treatment and prognosis
Antithyroid medications (e.g. methimazole/carbimazole) are the first-line treatment. In medication-resistant Graves disease, patients can go onto radioactive iodine or thyroidectomy 14,15.
Complications
increased risk of thyroid cancer 14
History and etymology
It is named after Robert James Graves (1796-1852), an Irish surgeon who first described it in 1835 9, and Carl Adolph von Basedow (1799-1854), a German physician who described it in 1840 10,11,13. The Merseburger triad was first described by Basedow, who practised in Merseburg 12,13.
Differential diagnosis
For hyperthyroidism consider:
toxic thyroid adenoma
toxic multinodular goiter
extrathyroid origin
Practical points
patients with Graves disease are at higher risk of iodinated contrast media-induced thyrotoxicosis








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.