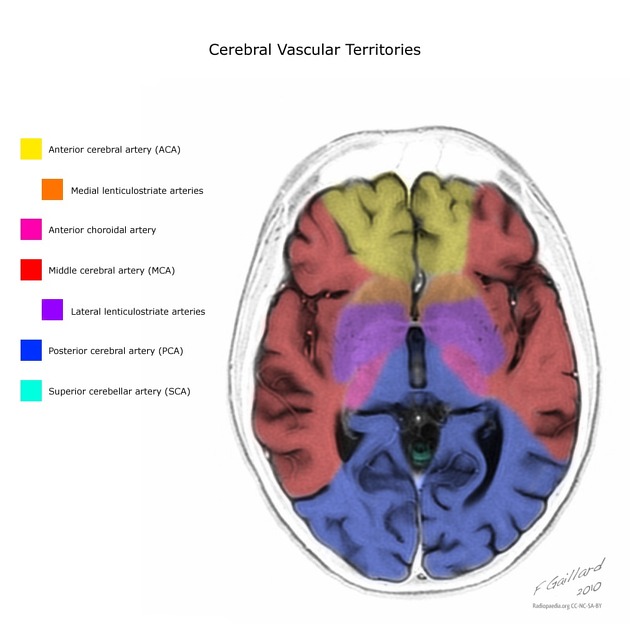
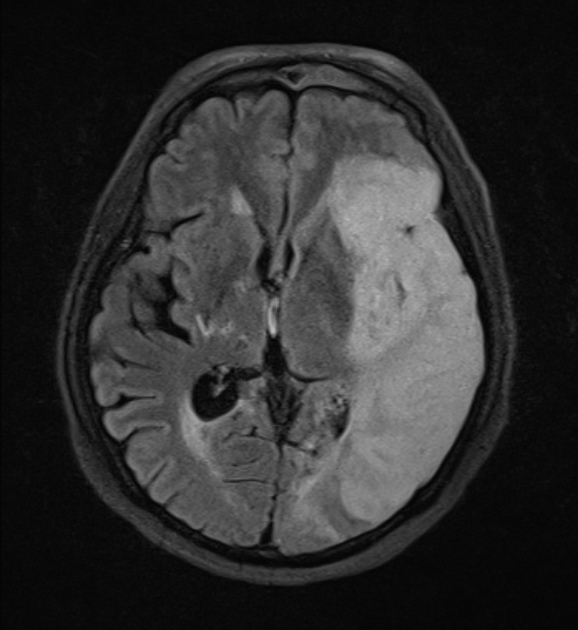
The middle cerebral artery territory is the most commonly affected territory in a cerebral infarction, due to the size of the territory and the direct flow from the internal carotid artery into the middle cerebral artery, providing the easiest path for thromboembolism.
On this page:
Clinical presentation
The neurological deficit will depend on the extent of the infarct and hemispheric dominance, and include:
- contralateral hemiparesis
- contralateral hemisensory loss
- hemianopia
- aphasia: if the dominant hemisphere is involved; may be expressive in anterior MCA territory infarction, receptive in posterior MCA stroke, or global with extensive infarction
- neglect: non-dominant hemisphere
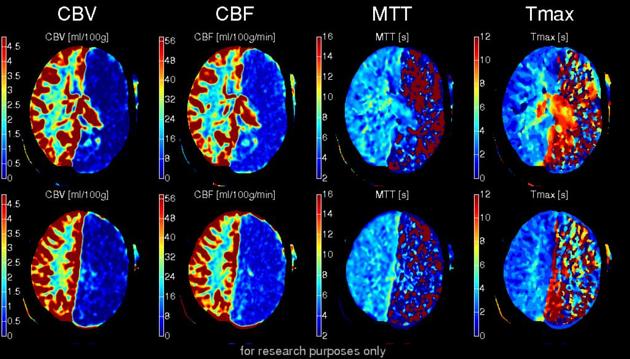
Radiographic features
Generally, the features are those of cerebral infarction, similar to those seen in any other territory. As such these features are discussed in the generic article: cerebral infarction.
There are however certain features specific to middle cerebral artery infarct, and these are discussed below. For both CT and MRI it is worth dividing the features according to the time course.
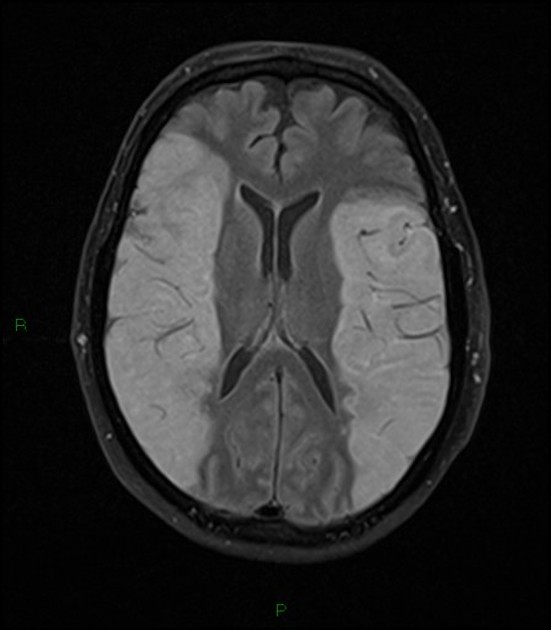
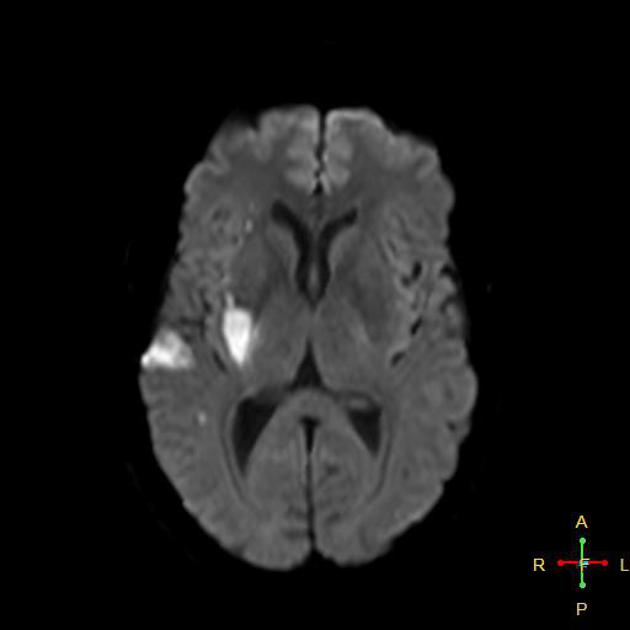
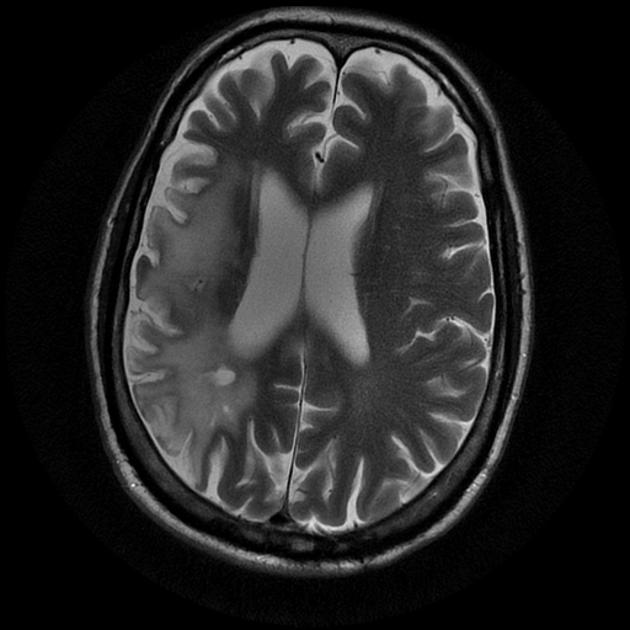
It should also be noted that middle cerebral artery infarcts are often incomplete affecting only perforator branches or one or more distal branches. As such in many cases, only parts of the middle cerebral artery territory are affected.
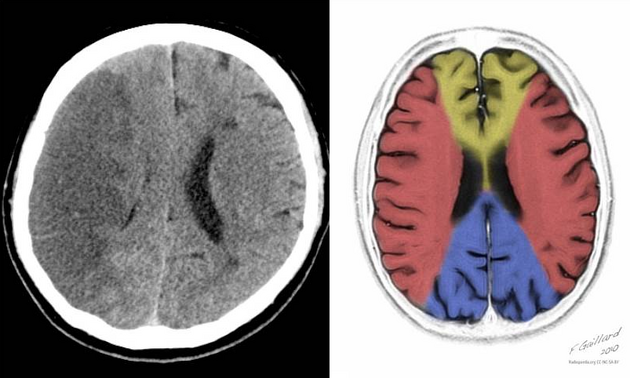
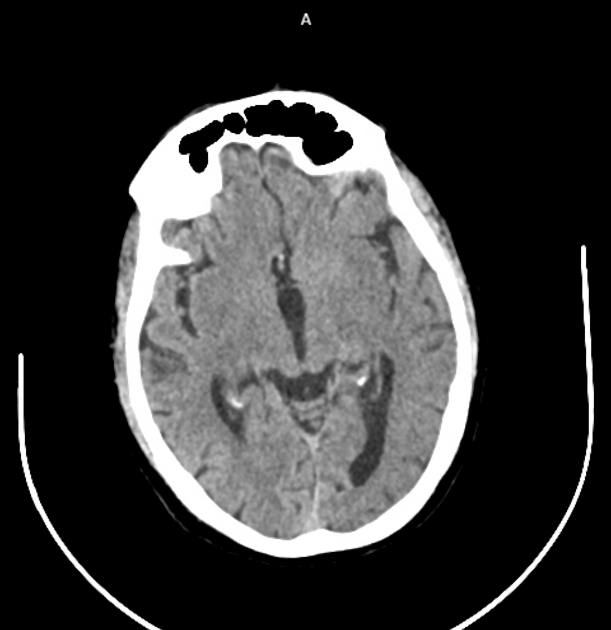
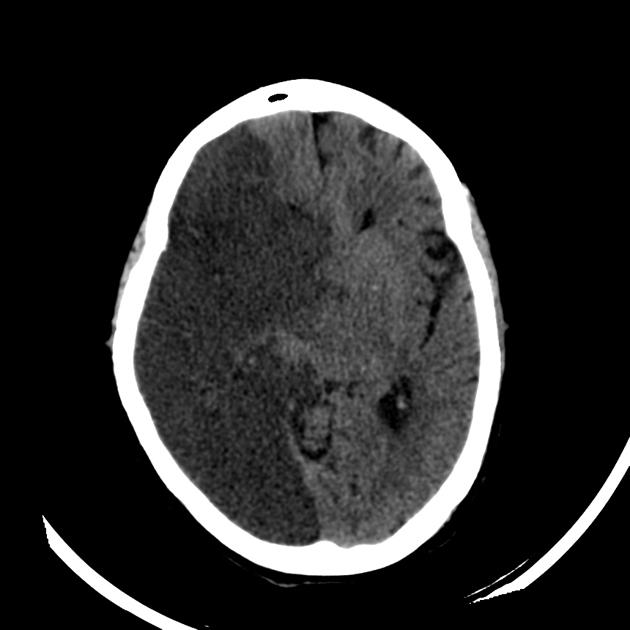
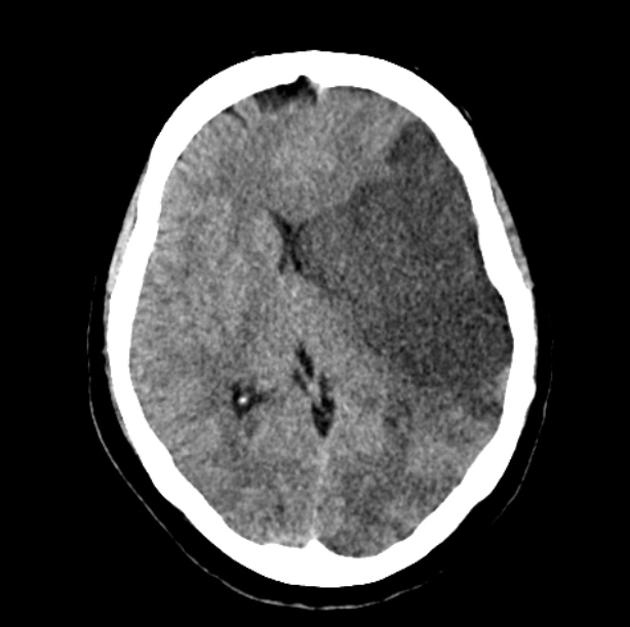
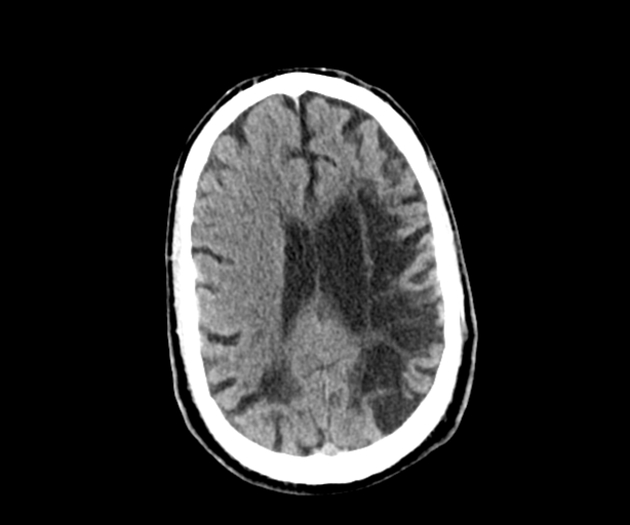
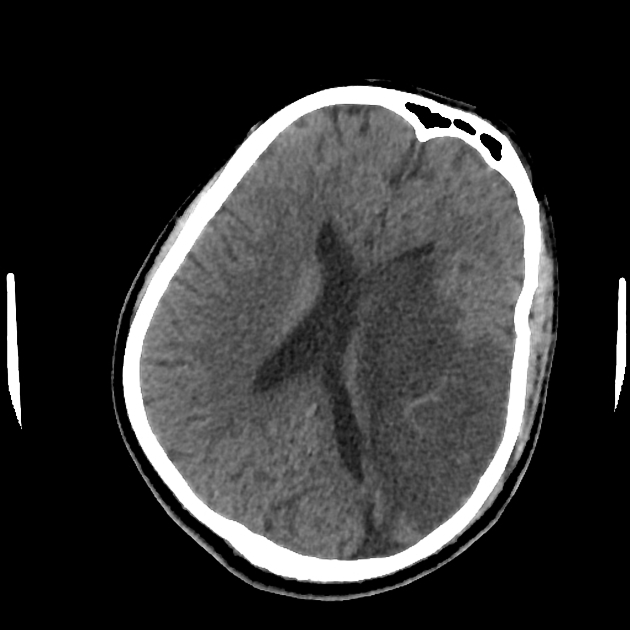
CT
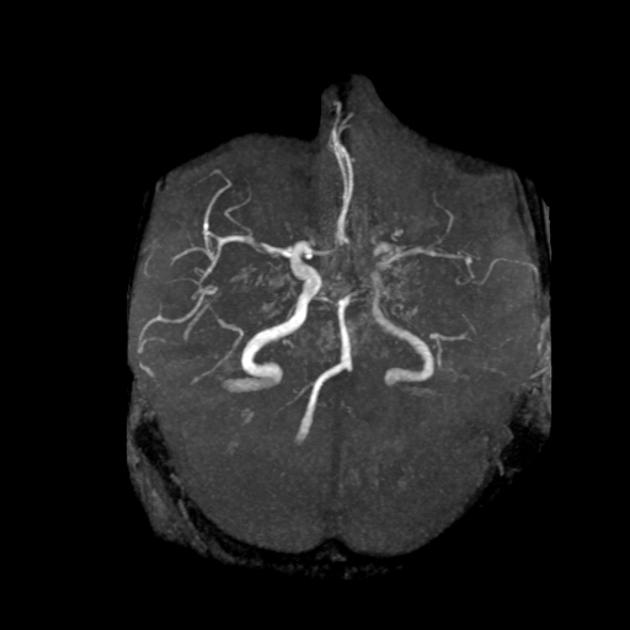
The earliest finding of middle cerebral artery occlusion is:
-
hyperdense middle cerebral artery sign 3
- seen immediately and represents direct visualization of the thromboembolism.
- presence of calcification is important as it is a contraindication to angioplasty
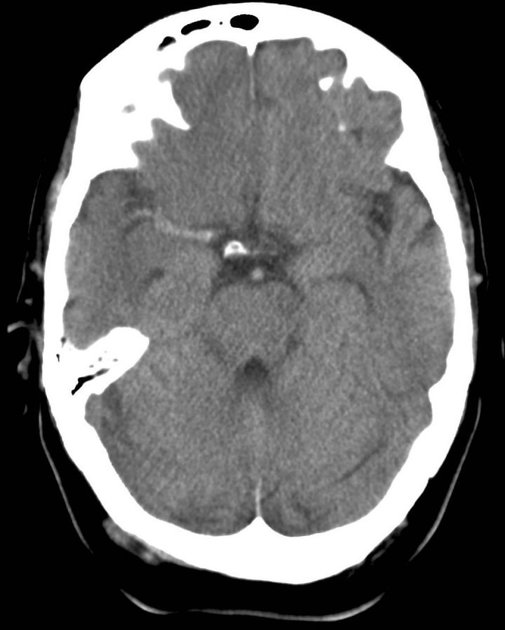
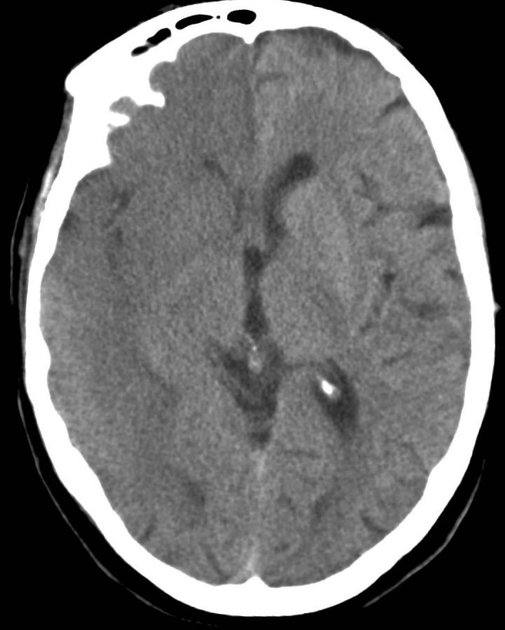
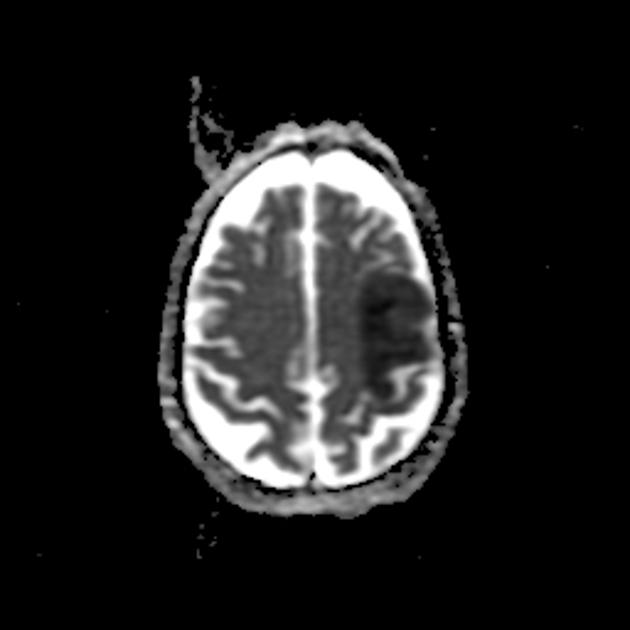
Early parenchymal signs include subtle blurring, decreased attenuation and swelling of the grey-white matter junction of affected regions. It should be noted that deep grey matter structures are affected before the cortex due to lenticulostriate arteries being end arteries, and cytotoxic edema (intracellular fluid accumulation) occurring earlier 2,4:
-
lentiform nucleus; caudate nucleus
- as early as 1 hour after occlusion 4
- visible in 75% of patients at 3 hours 4
-
insular ribbon
- although cortical it is the furthest cortex from collateral circulation and is therefore also affected early 4
- the insular ribbon sign describes loss of normal grey-white differentiation
- surface cortex (including peri-rolandic cortex)
- collateral flow retards the development of CT signs with only 20% of cases demonstrating changes at 3 hours 4
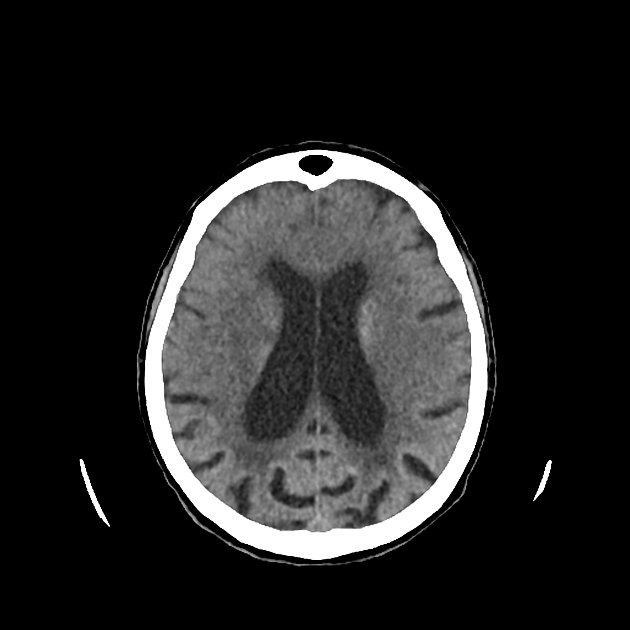
With time the hypo-attenuation and swelling become more marked, and in patients with the majority of the MCA territory affected the mass effect is often dramatic and life-threatening, sometimes requiring a decompressive craniectomy.
As time passes the infarct undergoes a gradual reduction in swelling and mass effect (see cerebral infarction).
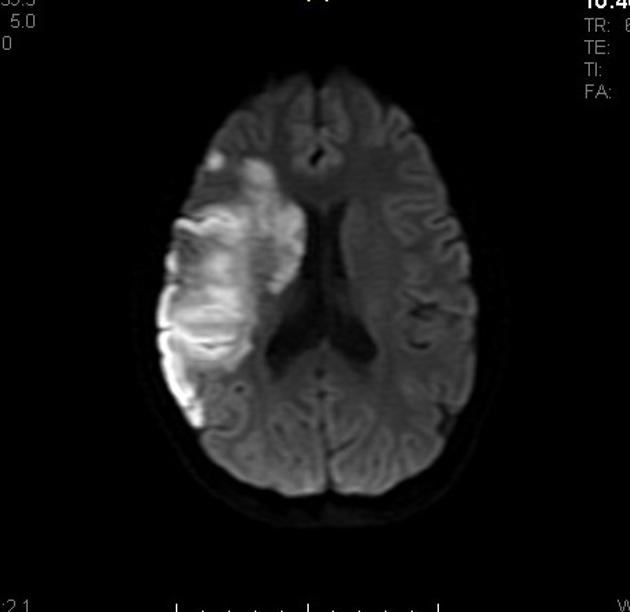
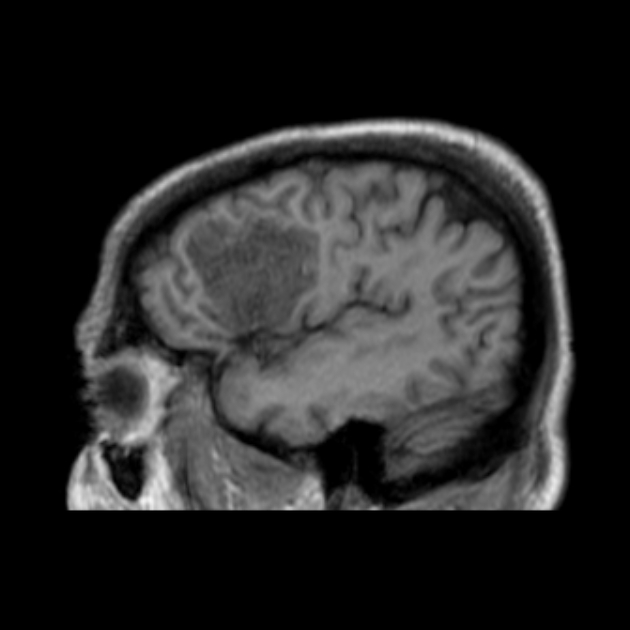
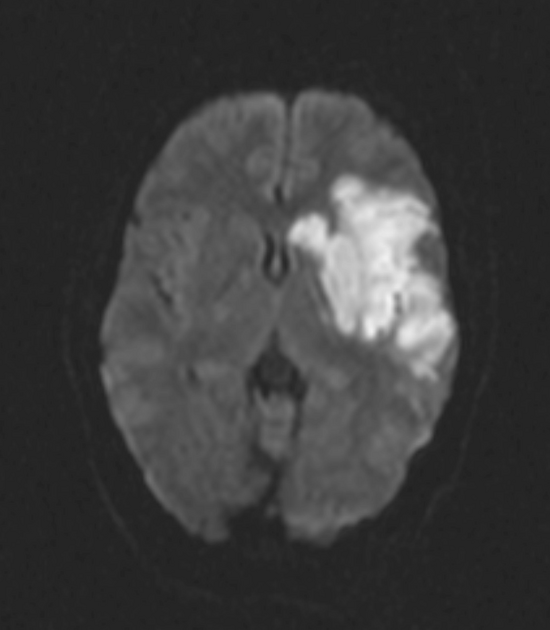
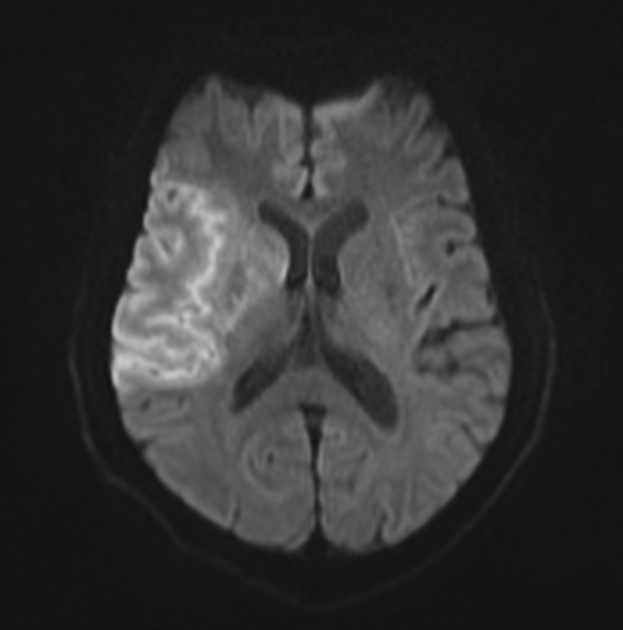
MRI
Other than demonstrating the typical distribution of affected tissue or occlusion of the vessel on MRA, appearances of a middle cerebral artery infarct are similar to those of infarcts anywhere else (see cerebral infarction).
Treatment and prognosis
Treatment of middle cerebral artery infarcts is the same as infarcts anywhere else in the anterior circulation (see cerebral infarction) except that due to the size of the involved territory the degree of mass effect resulting from infarction can be marked and life-threatening. As such decompressive craniectomy is advocated by many as a life-saving procedure.












 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.