Multiple myeloma (MM), also known by the names plasma cell myeloma and Kahler disease, is a multifocal proliferation of plasma cells based in the bone marrow. It is the most common primary malignant bone neoplasm in adults. It arises from red marrow due to the monoclonal proliferation of plasma cells and manifests in a wide range of radiographic abnormalities. Multiple myeloma remains incurable.
Multiple myeloma accounts for one of the 'M's in the popular mnemonic for lucent bone lesions FEGNOMASHIC.
On this page:
Terminology
As per the WHO classification of tumors of hematopoietic and lymphoid tissues, multiple myeloma is called plasma cell myeloma 14. Historically, it was sometimes known as Kahler disease or myelomatosis 13.
Four main patterns are recognized:
disseminated form: multiple well-defined "punched out" lytic lesions: predominantly affecting the axial skeleton
disseminated form: diffuse skeletal osteopenia
solitary plasmacytoma: a single large/expansile lesion most commonly in a vertebral body or in the pelvis
The remainder of this article relates to the disseminated forms. Please refer to the article plasmacytoma for discussion of the latter.
Smoldering multiple myeloma refers to a form that falls on the spectrum between monoclonal gammopathy of unknown significance (MGUS) and active multiple myeloma. Patients are asymptomatic, with worse biochemistry than MGUS but without the end-organ damage of active multiple myeloma 9.
Diagnosis
International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma has following definition for multiple myeloma 15:
clonal bone marrow plasma cells ≥10% or biopsy-proven bony or extramedullary plasmacytoma, and
-
any one or more of the following myeloma defining events:
-
evidence of end-organ damage that can be attributed to the underlying plasma cell proliferative disorder, specifically:
hypercalcemia: serum calcium >0.25 mmol/L (>1 mg/dL) higher than the upper limit of normal or >2.75 mmol/L (>11 mg/dL)
renal insufficiency: creatinine clearance <40 mL per min or serum creatinine >177 μmol/L (>2 mg/dL)
anemia: hemoglobin value of >20 g/L below the lower limit of normal, or a hemoglobin value <100 g/L
bone lesions: one or more osteolytic lesions on skeletal radiography, CT, or PET-CT
-
any one or more of the following biomarkers of malignancy
clonal bone marrow plasma cell percentage ≥60%
involved:uninvolved serum free light chain ratio ≥100
>1 focal lesions on MRI studies
-
The myeloma defining events can be recalled with the mnemonic SLiM-CRAB 15.
Epidemiology
Multiple myeloma is a common malignancy in patients above 40; 70% of cases are diagnosed between ages 50 and 70 with a median age of diagnosis being 70 years; there is a male predilection (M: F 2:1) 7,12,14. It accounts for 1% of all malignancies and 10-15% of all hematological neoplasms 12,14. Black populations are affected at nearly twice the rate as White populations 14. Multiple myeloma and osteosarcoma combined account for ~50% of all primary bone malignancies 7.
Clinical presentation
Clinical presentation of patients with multiple myeloma is varied, and includes 1,2,7:
-
bone pain
initially intermittent, but becomes constant
worse with activity/weight-bearing, and thus is worse during the day
-
anemia
typically normochromic/normocytic
renal failure
hypercalcemia
proteinuria
The typical features can be recalled with the mnemonic CRAB 12.
Complications
Presentation may also be with a complication, including:
-
vertebral compression fracture
long bone fracture (e.g. proximal femur)
recurrent infection: e.g. pneumonia due to leukopenia
plasmacytomas typically progress to multiple myeloma
Pathology
Multiple myeloma results from monoclonal proliferation of malignant plasma cells which produce immunoglobulins and infiltrate haemopoietic locations (i.e. red marrow). The paraprotein produced is most commonly IgG (~50%), followed by IgA (~20%) and light chain only (~15%), while IgM and non-secretory multiple myeloma are very rare 17.
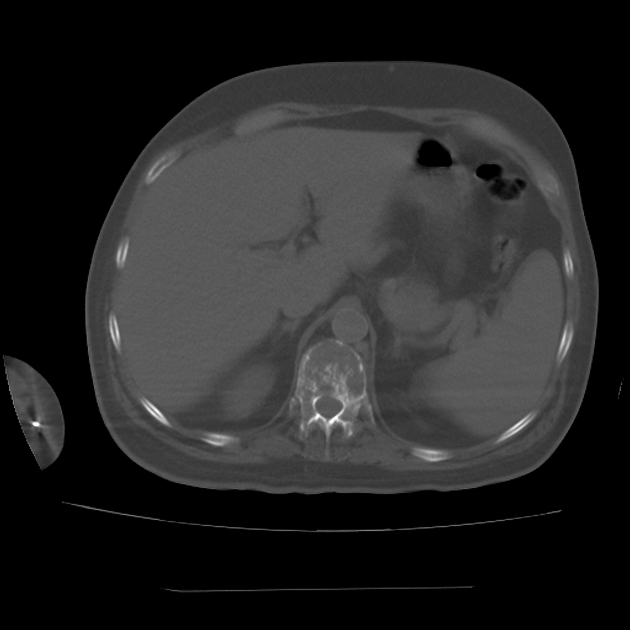
Renal involvement is common and renal failure is multifactorial:
-
obstructive casts form in the renal tubules composed of Bence Jones proteins, immunoglobulins, albumin and Tamm-Horsfall proteins
most common cause of renal failure in multiple myeloma
direct nephrotoxicity of Bence Jones proteins on the epithelial cells of the renal tubules
hypercalcemia and dehydration
hyperuricemia and urate nephropathy due to high cell turnover
amyloidosis (AL type)
increased risk of renal infection
The initial presentation occasionally is a polyneuropathy when it is part of POEMS syndrome (mostly the sclerotic form).
Markers
reverse albumin/globulin ratio (i.e. low albumin, high globulin)
monoclonal gammopathy (IgA and/or IgG peak)
Bence Jones protein (Ig light chain) proteinuria
hypercalcemia
decreased or normal alkaline phosphatase (ALP) unless there is a pathological fracture due to impaired osteoblastic function
Approximately 3% of cases will have a negative serum electrophoresis (i.e. non-secretory MM) 16 and negative urine Bence Jones protein ref.
Staging
The most popular staging system, the International Staging System, uses the combination of β2-microglobulin test and serum albumin 6.
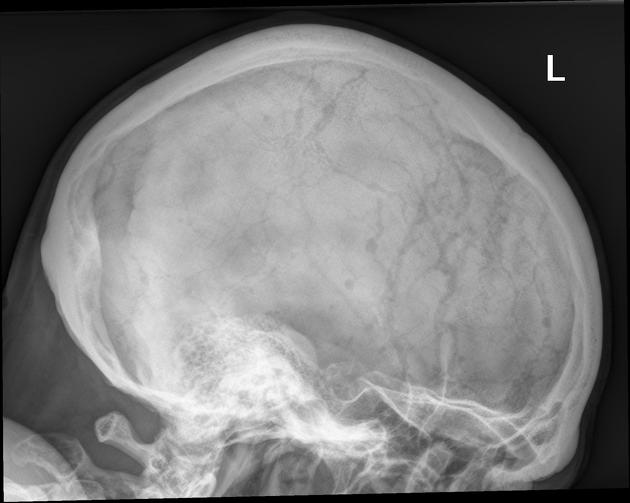
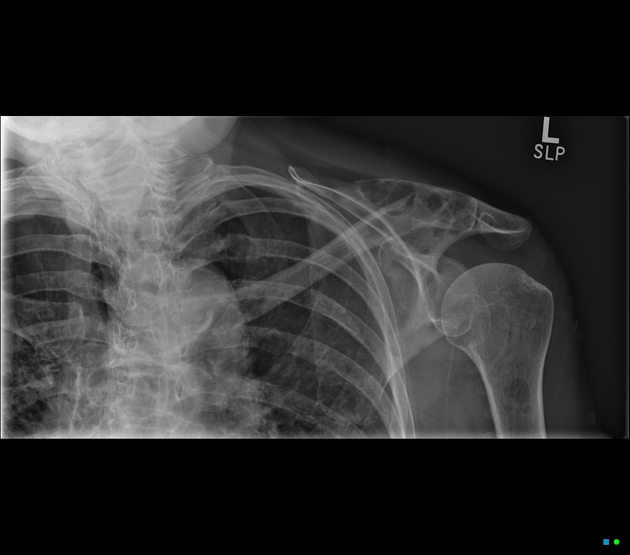
Distribution
Distribution of multiple myeloma mirrors that of red marrow in the older individual, and thus this is mostly encountered in the axial skeleton and proximal appendicular skeleton 14:
vertebrae (most common)
ribs
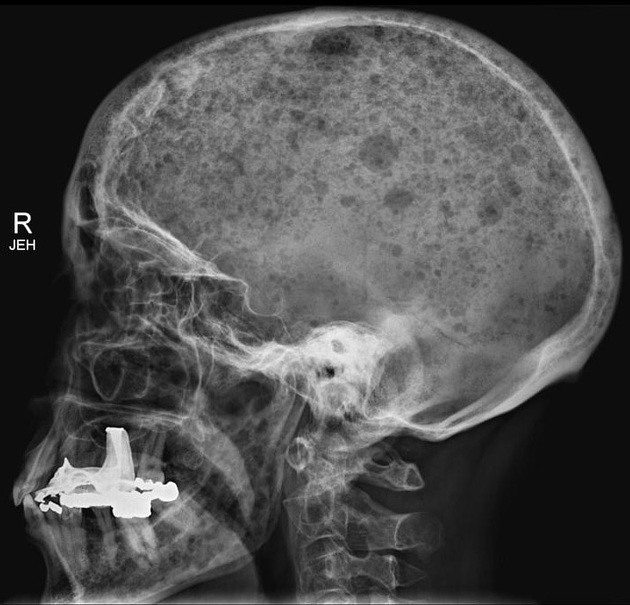
skull
shoulder girdle
pelvis
long bones
extraskeletal structures (extraosseous myeloma): rare
Radiographic features
Radiology has a number of roles in the diagnosis and management for multiple myeloma:
suggest the diagnosis / exclude other causes
assess possible mechanical complications (e.g. pathological fracture)
assess disease progression
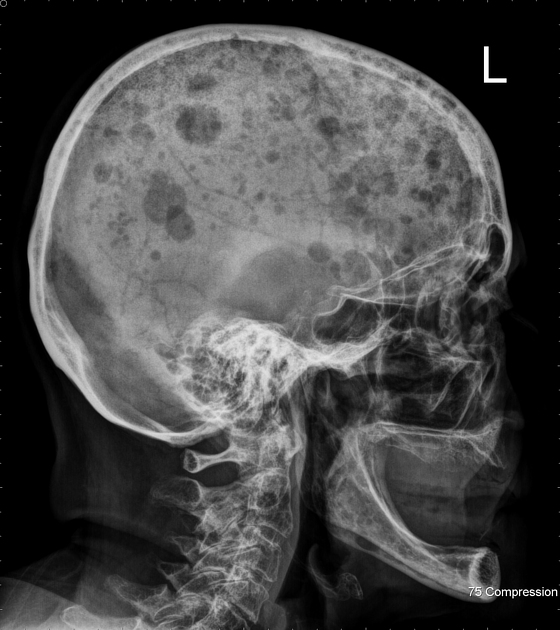
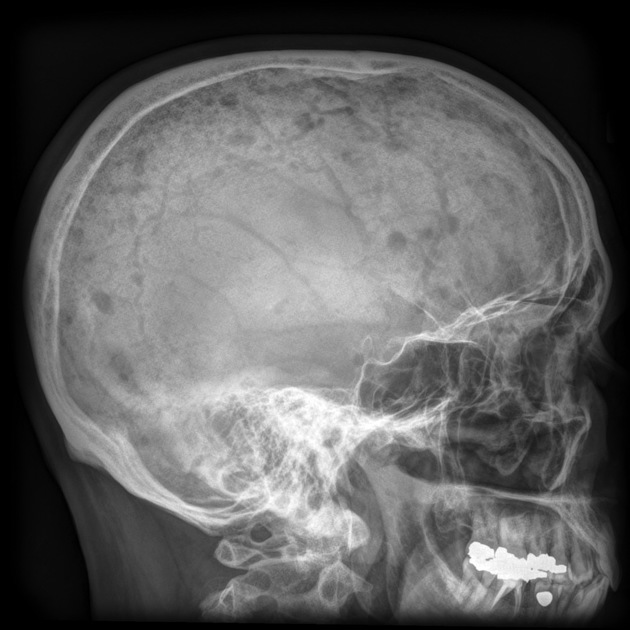
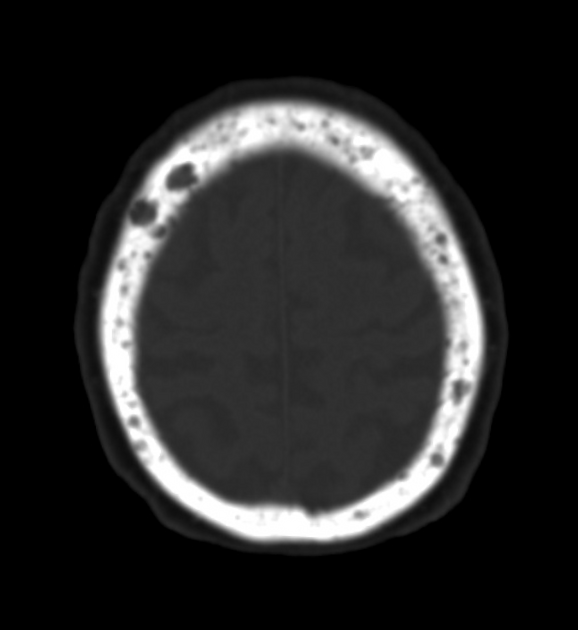
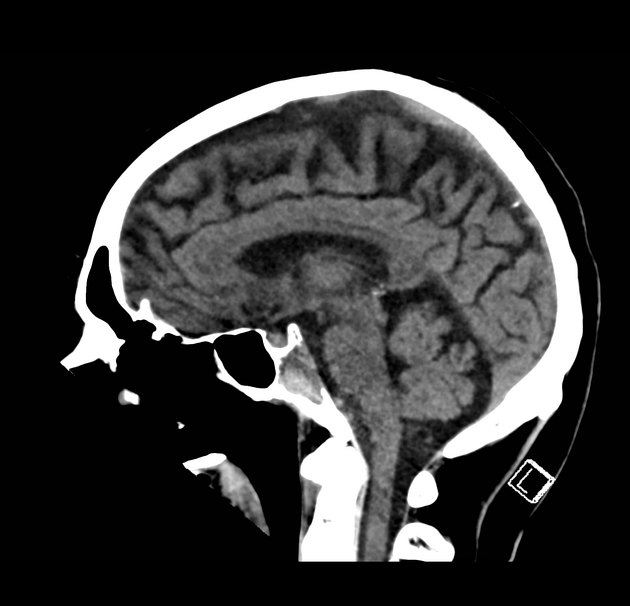
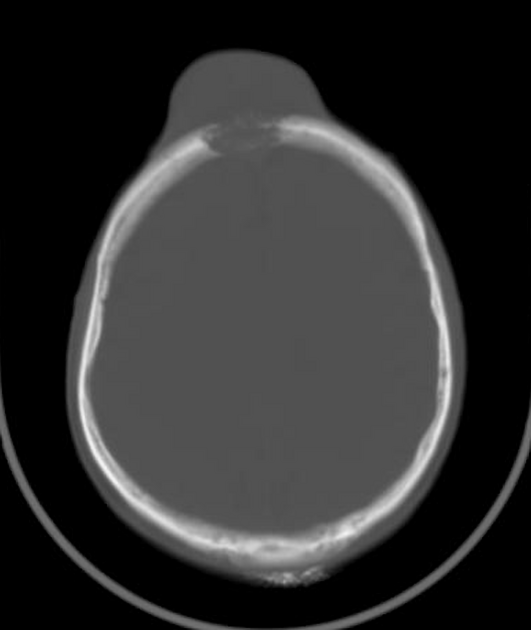
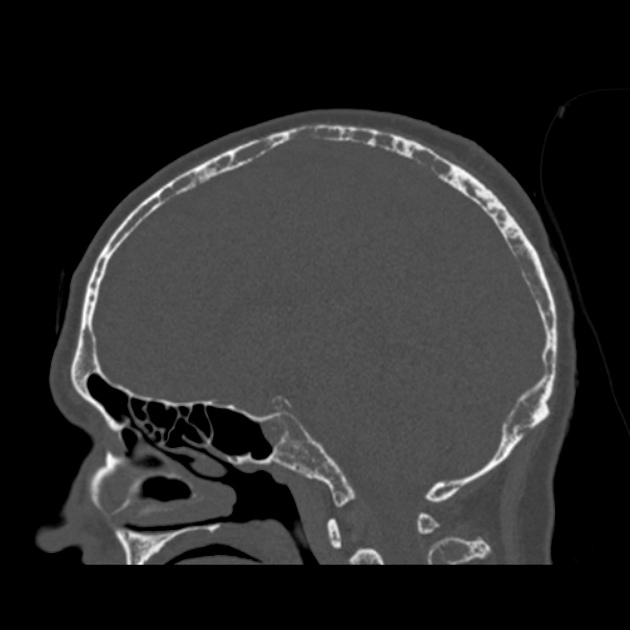
Disseminated multiple myeloma has two common radiological appearances, although it should be noted that initially, radiographs may be normal, despite the presence of symptoms. The two main diffuse patterns are 12:
-
numerous, well-circumscribed, lytic bone lesions (70% of cases 14)
-
punched out lucencies
-
-
generalized osteopenia (less common)
often associated with vertebral compression fractures/vertebra plana
Plain radiograph
A skeletal survey is essential not only for the diagnosis of multiple myeloma but also in pre-empting potential complications (e.g. pathological fracture) and assessing response to therapy. ~40% bone destruction is required for lesion detection, thus giving the skeletal survey a high false-negative rate of ~50% (range 30-70%) 12.
The vast majority of lesions are purely lytic, sharply defined/punched out, with endosteal scalloping when abutting the cortex. Lesions are sclerotic in only 3% of patients 7.
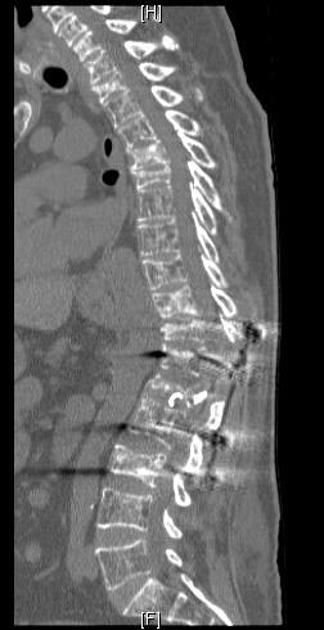
CT
Whole-body low dose CT is more accurate than a skeletal survey with a sensitivity of ~70% and specificity of ~90% with a dose 1-2x that of a skeletal survey 12. Whole-body low dose CT is also better to assess the risk of pathological fracture in severely affected bones as well as the presence of extramedullary lesions 12.
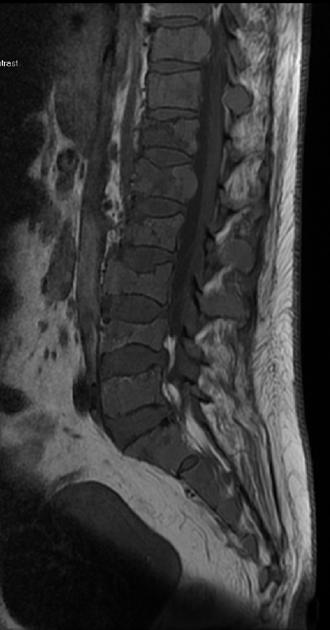
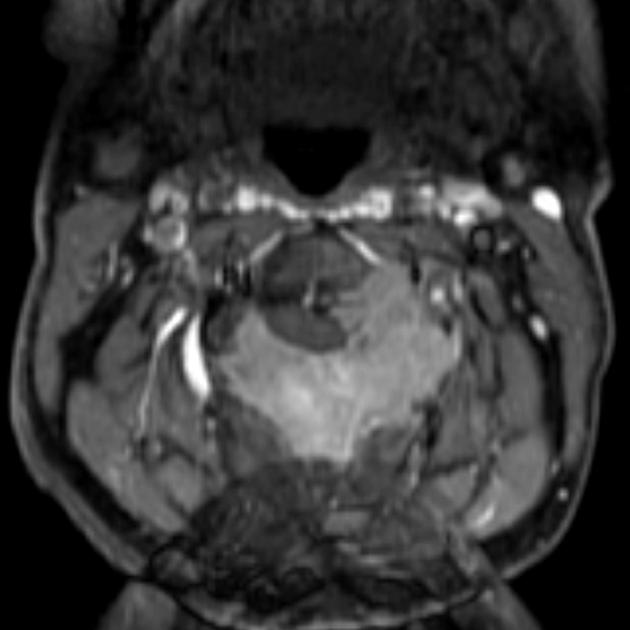
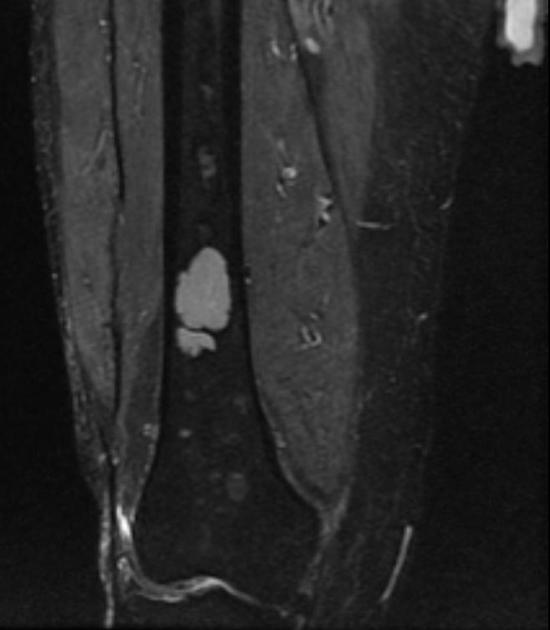
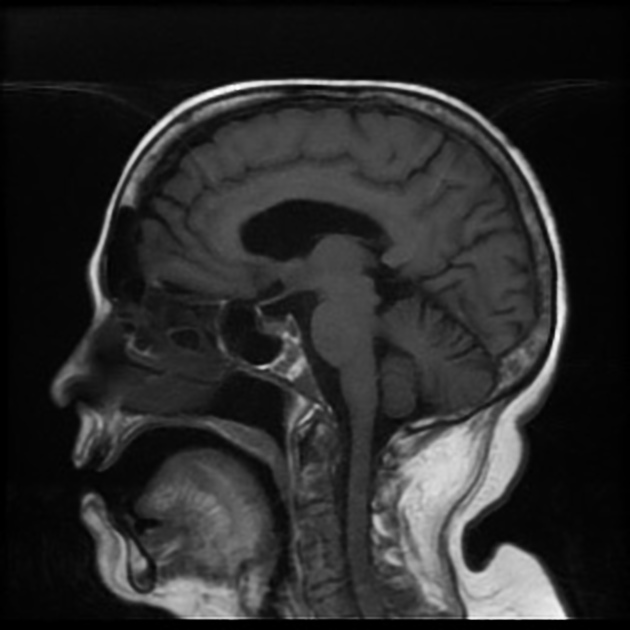
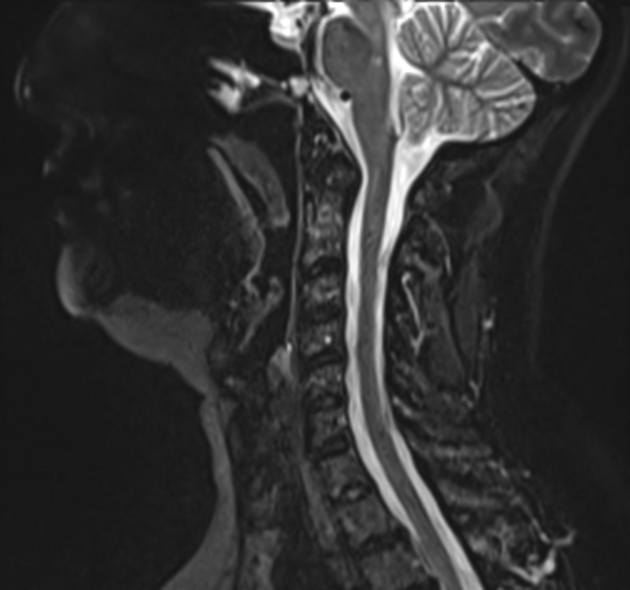
MRI
A whole-body MRI technique may be deployed. MRI is more sensitive in detecting multiple lesions compared to the standard plain film skeletal survey and CT 8,12. Five patterns have been described 12:
normal bone marrow signal
diffuse involvement
focal involvement
combined diffuse and focal involvement
variegated ("salt and pepper")
Signal characteristics
Most frequently used MR sequences for the evaluation of bone marrow are conventional T1 spin-echo and T2 spin-echo sequences 11.
-
T1
typically low signal
high-grade, diffuse involvement may become isointense to adjacent normal marrow
-
T2 with fat-suppression
high signal
infiltration of the ribs is probably best appreciated on T2 images with fat suppression, appearing bright: ‘white ribs sign’
-
T1 C+ (Gd)
hyperintense
-
several enhancement curves may be seen:
type 4 curve: represents a steep wash-in of contrast medium, due to the high vascularization and perfusion with leakage through the highly permeable capillaries, followed by an early wash-out back into the intravascular space because of the small interstitial space with closely packed plasma cells 10,11
type 3 and type 5 curves may also be seen
DWI/ADC: lesions usually exhibit restricted diffusion, with higher signal on high b-value DWI compared to the very low signal of normal background marrow 11
Nuclear medicine
Bone scintigraphy
Bone scintigraphy appearances of disseminated multiple myeloma is variable due to the potential lack of osteoblastic activity. Larger lesions may be either hyperactive (hot) or photopenic (cold). Bone scans may also be normal. Therefore, bone scans usually do not contribute significant information to the workup of patients with suspected or established disseminated multiple myeloma, as the sensitivity of detecting lesions is less than that of a plain film skeletal survey 7.
FDG PET-CT
FDG PET-CT is effective in identifying the distribution of disease 14. F-18 FDG uptake by the myeloma lesions corresponds to lytic bone lesions or soft tissue plasmacytomas seen on CT. However, focal high FDG uptake in the bone may be considered a positive lesion even in the absence of osteolysis on CT.
Treatment and prognosis
Multiple myeloma remains incurable with a median survival of 5.5 years (range <6 months to >10 years) 14. Management with agents such as thalidomide, lenalidomide, bortezomib (proteasome inhibitor), and daratumumab (CD38 monoclonal antibody) have provided significant survival gains 6. These are typically used in combination with older agents such as cyclophosphamide, melphalan, or dexamethasone 6.
Stem-cell harvest and autologous hematopoietic stem cell transplant post-chemotherapeutic/radiotherapy bone marrow ablation are also used, although relapse is inevitable.
Response assessment
As imaging is not required to diagnose multiple myeloma, assessment of treatment response does not necessitate imaging studies, with the exception of so-called "imaging plus minimal residual disease negative" status, which requires FDG PET. However, patients who have known lesions identified on radiologic studies of various modalities at baseline should have these reevaluated as part of response assessment. See the separate article on the International Myeloma Working Group response criteria.
Complications
Differential diagnosis
The main differential is that of widespread bony metastases. Findings that favor the diagnosis of bone metastases over that of multiple myeloma include:
more commonly affect the vertebral pedicles rather than vertebral bodies
distal appendicular skeleton
although both entities have variable bone scan appearances (both hot and cold) unlike myeloma, extensive bony metastases rarely have a normal appearance
Other rare entities include:
Waldenström macroglobulinemia: IgM paraprotein



























 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.