Pulmonary embolism (PE) refers to partial or complete embolic occlusion of one or more pulmonary arteries, most commonly due to thrombus. PE is apparent as a ventilated perfusion defect on V/Q scan 35.
Non-thrombotic pulmonary emboli sources include 30:
gas embolism, e.g. air embolism, carbon dioxide embolism, nitrogen, helium
tumor embolism: comprised of tumor thrombus
-
infectious material
foreign body, e.g. catheter embolism or brachytherapy seeds
-
particulate material embolism, e.g.
cement embolism: comprised of polymethyl methacrylate (PMMA)
On this page:
Terminology
Classification of a pulmonary embolism may be based upon:
the presence or absence of hemodynamic compromise
temporal pattern of occurrence
the presence or absence of symptoms
the vessel which is occluded
Epidemiology
Risk factors
recent surgery
prolonged bed rest/immobility
malignancy: including multiple myeloma 23
-
HIV 22:
2-10x increased risk, cf. non-HIV matched controls
COVID-19 27
-
medication
oral contraceptives
thalidomide, lenalidomide 31
pregnancy
known or previous DVT
-
presence of certain venous aneurysms
e.g. popliteal venous aneurysm 15
Diagnosis
Clinical decision rules, in conjunction with physician gestalt and estimated pretest probability of disease, may serve as a supplement in risk stratification:
PERC rule (to rule out PE)
ECG
sinus tachycardia: the most common abnormality
-
right heart strain pattern
incomplete or complete right bundle branch block
prominent R wave in lead V1
right axis deviation
T-wave inversion in the right precordial leads +/- the inferior leads is seen in up to 34% of patients and is associated with high pulmonary artery pressures 25
SIQIIITIII pattern
Clinical presentation
The patient may report a history of immobilization or surgery, active malignancy, hormone usage, or a previous episode of thromboembolism. The physical exam may reveal suggestive features such as:
-
clinical signs of deep venous thrombosis (DVT)
asymmetric pitting lower extremity edema
prominent superficial collateral vessels
tenderness to palpation along the deep venous system
tachycardia
dyspnea
pleuritic chest pain
hemoptysis
Pathology
Classification
-
hemodynamic
low-risk
-
temporal pattern
acute
subacute
-
vessel
lobar
segmental
subsegmental
Markers
D-dimer (ELISA) is commonly used as a screening test in patients with a low and moderate probability clinical assessment, in these patients:
normal D-dimer has almost 100% negative predictive value (virtually excludes PE): no further testing is required
raised D-dimer is seen with PE but has many other causes and is, therefore, non-specific: it indicates the need for further testing if pulmonary embolism is suspected 4
In patients with a high probability clinical assessment, a D-dimer test is not helpful because a negative D-dimer result does not exclude pulmonary embolism in more than 15%. Patients are treated with anticoagulants while awaiting the outcome of diagnostic tests 4.
Radiographic features
Depends to some extent on whether it is acute or chronic. Overall, there is a predilection for the lower lobes.
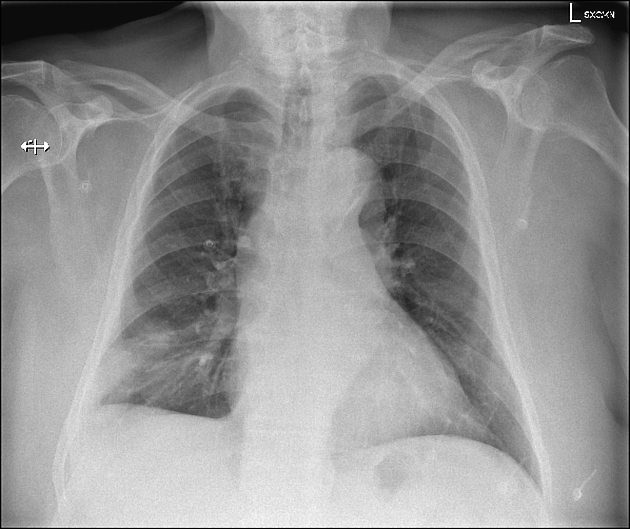
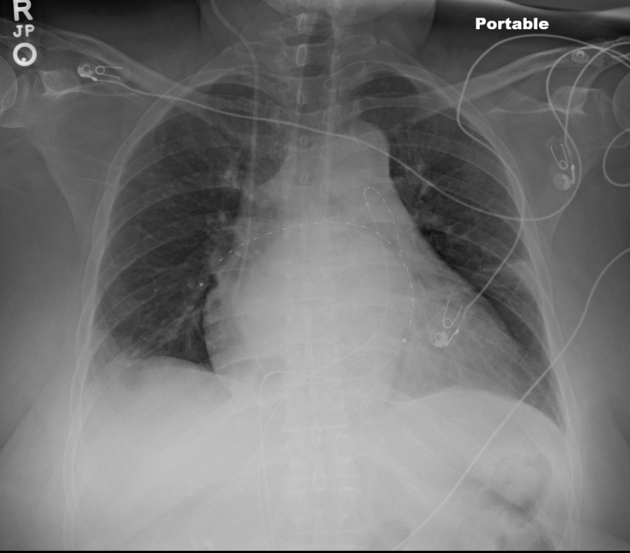
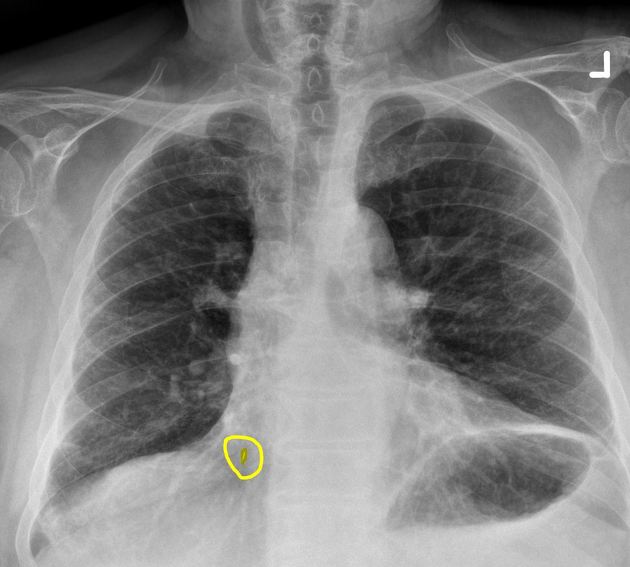
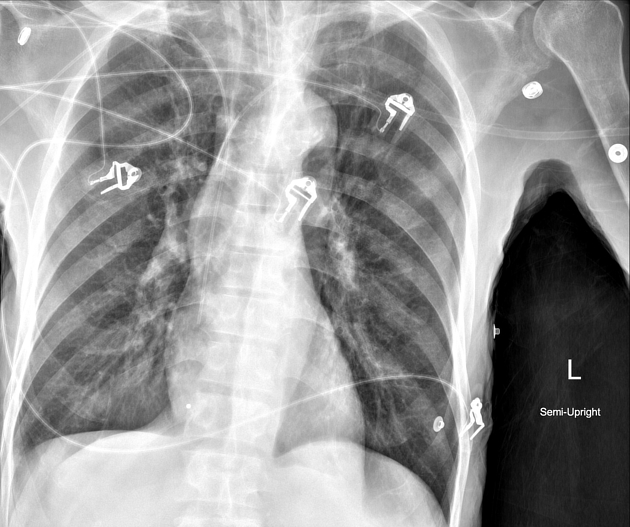
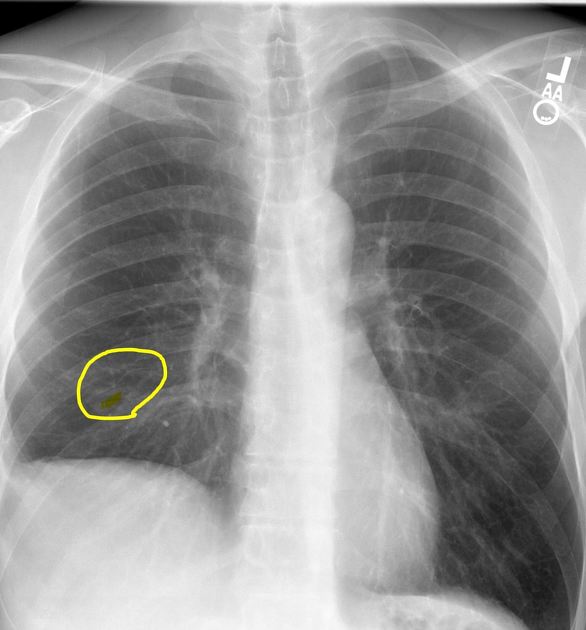
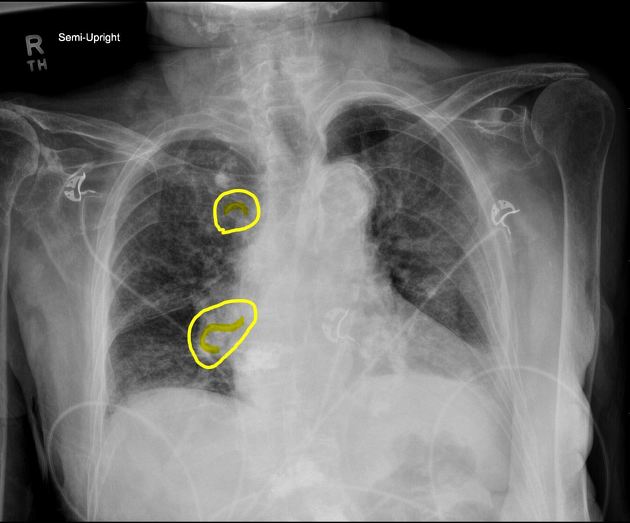
Plain radiograph
Chest radiography is neither sensitive nor specific for a pulmonary embolism. It is used to assess differential diagnostic possibilities such as pneumonia and pneumothorax rather than for the direct diagnosis of PE.
Pleural effusions are associated in 35% of cases (see pleural effusions in pulmonary embolism).
Described chest radiographic signs include:
Fleischner sign: enlarged pulmonary artery (20%)
Hampton hump: peripheral wedge of airspace opacity and implies lung infarction (20%)
Westermark sign: regional oligemia and highest positive predictive value (10%)
knuckle sign 11
Palla sign 17: enlarged right descending pulmonary artery
Chang sign 18: dilated right descending pulmonary artery with sudden cut-off
Sensitivity and specificity of chest x-ray signs 1:
-
sensitivity ~14%, specificity ~92% , PPV: ~38%, NPV: ~76%
-
vascular redistribution
sensitivity: ~10% , specificity: ~87% , PPV: ~21%, NPV: ~74%
-
sensitivity: ~22% , specificity: ~82%, PPV: ~29%, NPV: ~76%
-
sensitivity: ~36% , specificity: ~70%, PPV: ~28%, NPV ~76%
-
sensitivity: ~20%, specificity: ~85%, PPV: ~30%, NPV: ~76%
Ultrasound/echocardiography
Acute pulmonary emboli
Point-of-care ultrasonography is not recommended for a haemodynamically stable patient with suspected pulmonary embolism. In the presence of hemodynamic compromise, echocardiography may be of value to assess for the presence of severe right ventricular dysfunction;
if absent, another cardiopulmonary derangement is likely responsible
if unequivocally present, it can establish the need for emergent treatment
Echocardiographic features which may be suggestive include:
-
right ventricular dysfunction
commonly dilated and hypocontractile
flattening or dyskinesis of the interventricular septum
Of note, transesophageal echocardiography has a reported sensitivity of 81% and a specificity of 97% for ruling in acute pulmonary embolism after the detection of right ventricular overload on transthoracic echocardiography 24.
Chronic pulmonary emboli
Again not recommended as part of first-line work up.
Cumulative damage from repeated embolic insults is a common cause of chronic thromboembolic pulmonary hypertension, which demonstrates a variable degree of the aforementioned signs, but with significantly higher right ventricular pressures, right ventricular hypertrophy and diastolic dysfunction, and a higher degree of tricuspid regurgitation.
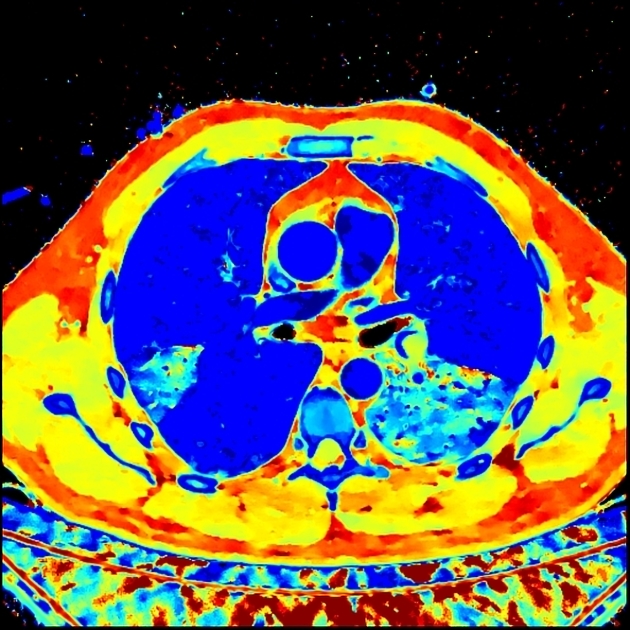
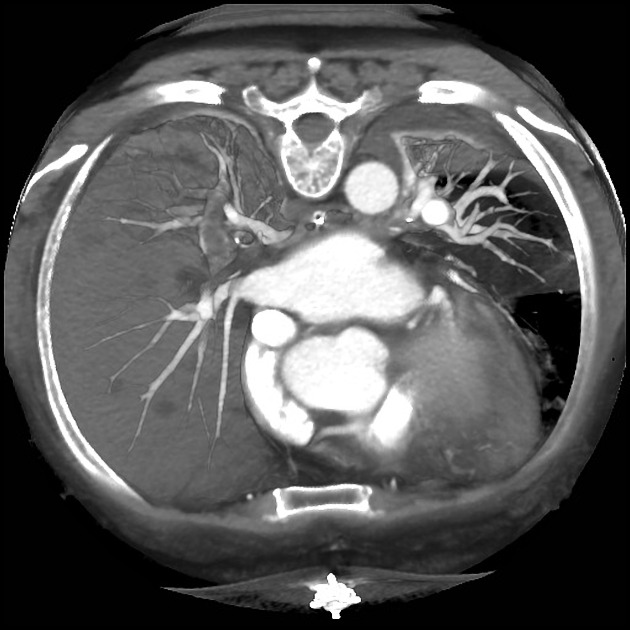
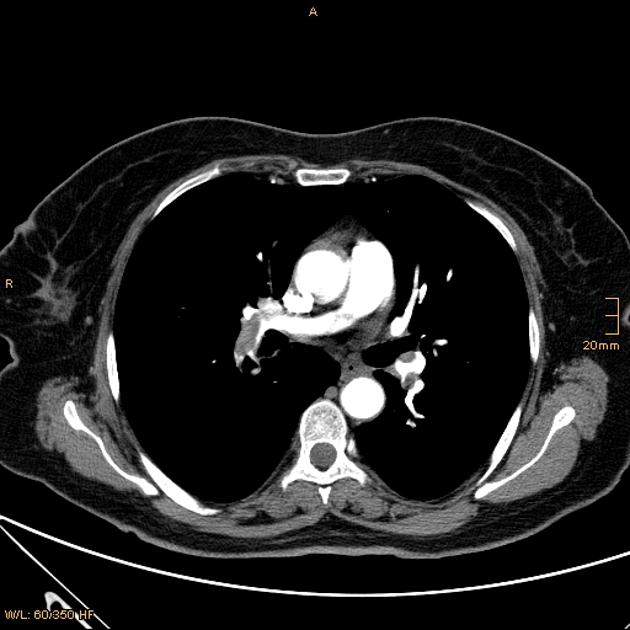
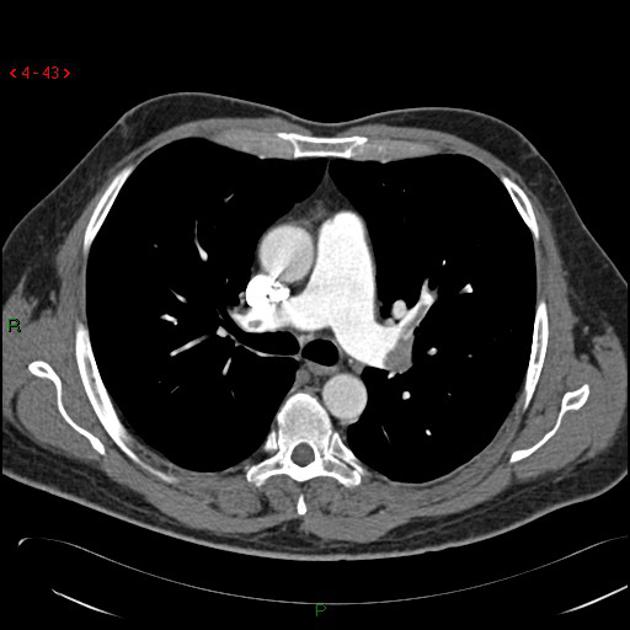
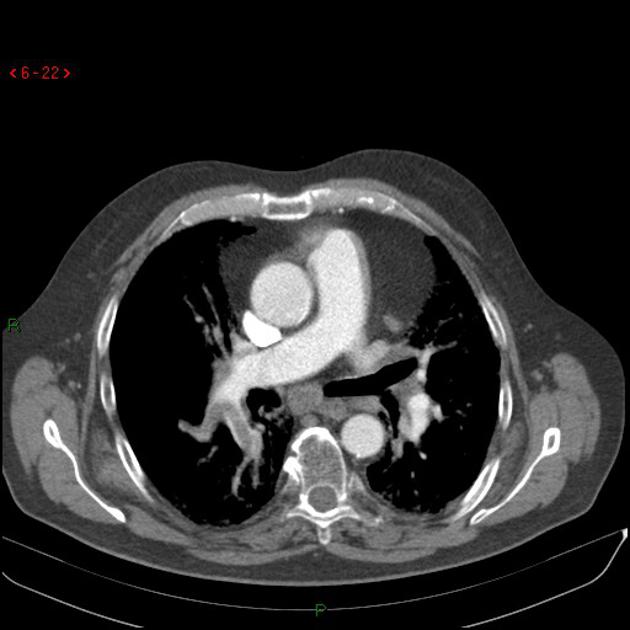
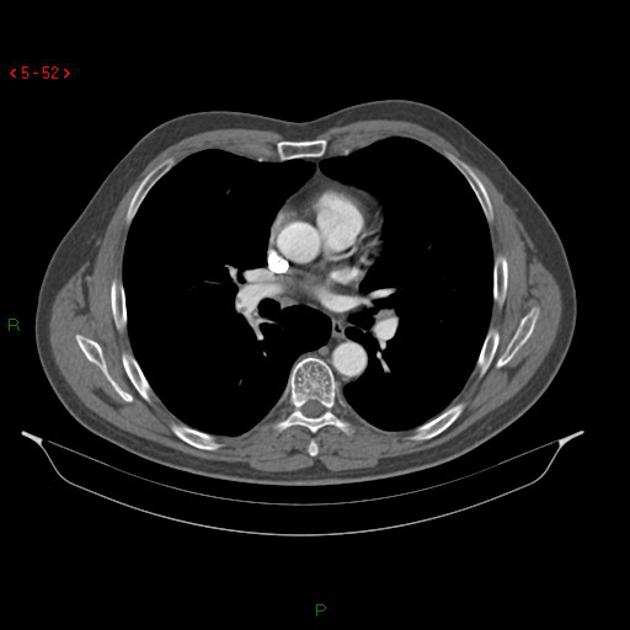
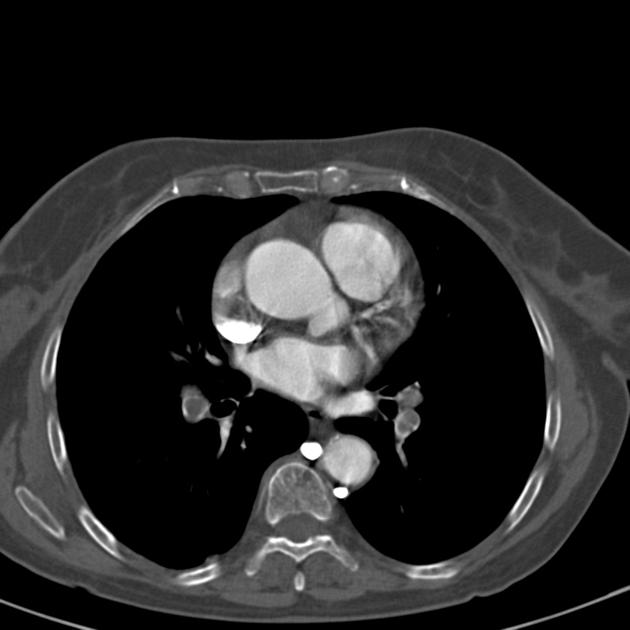
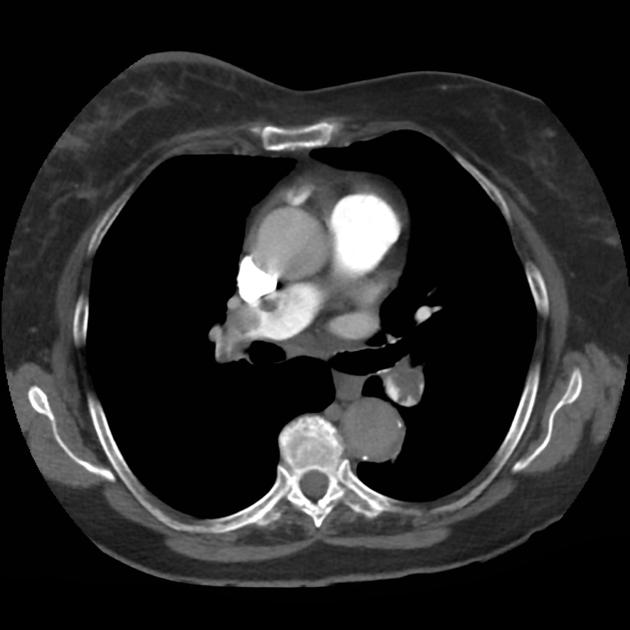
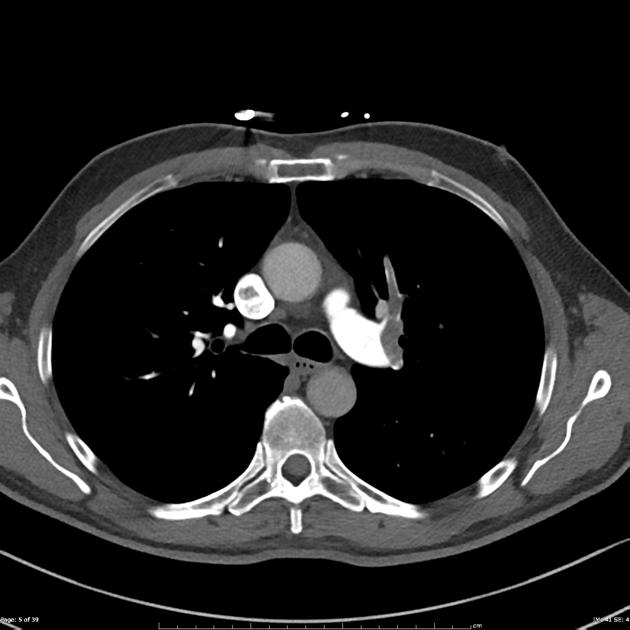
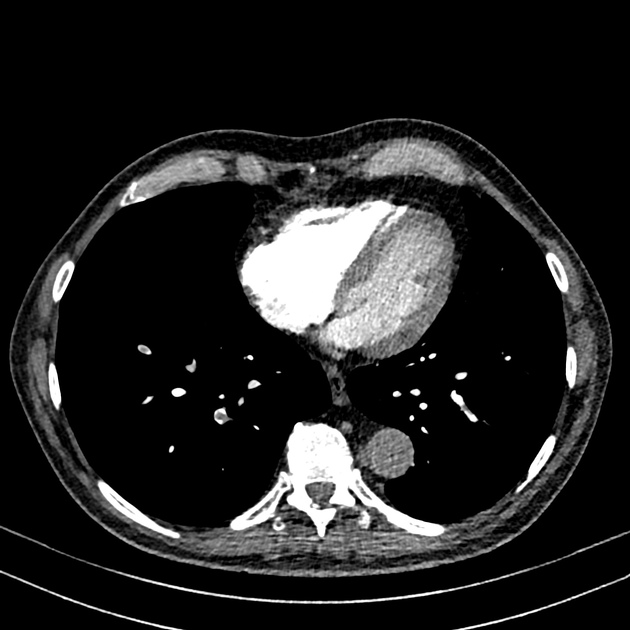
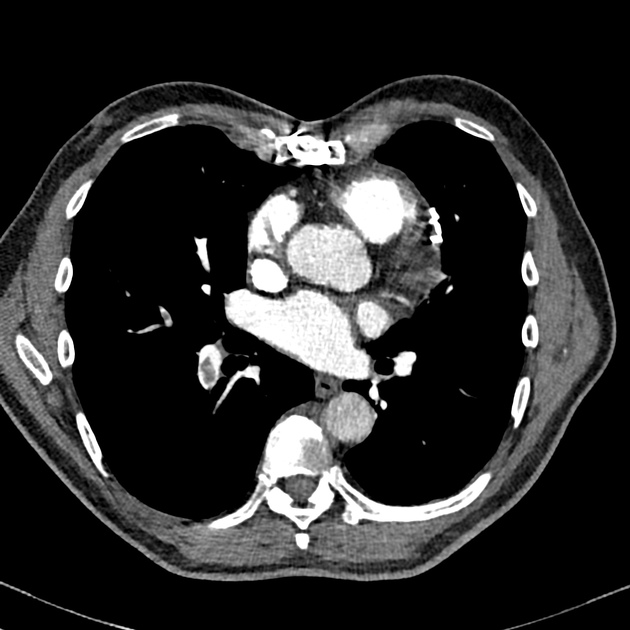
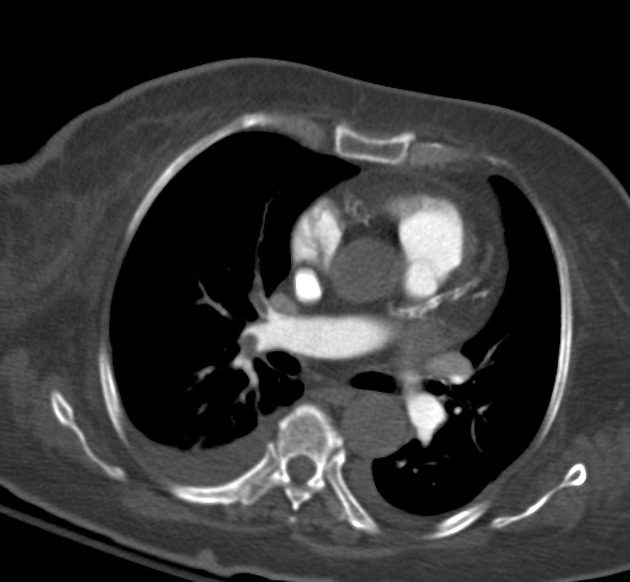
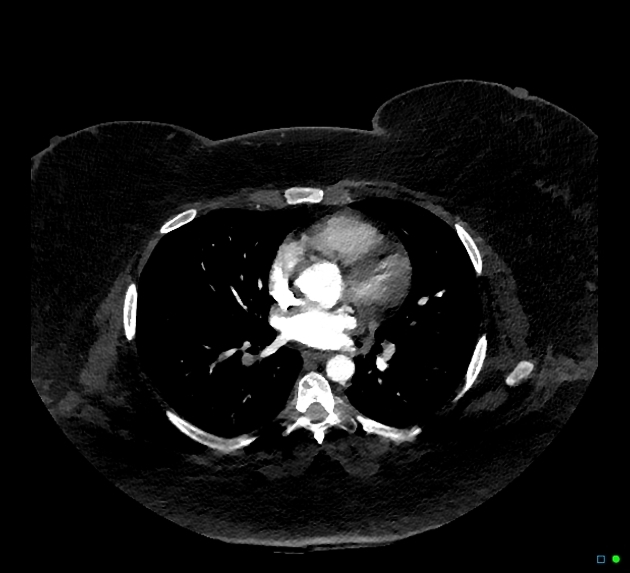
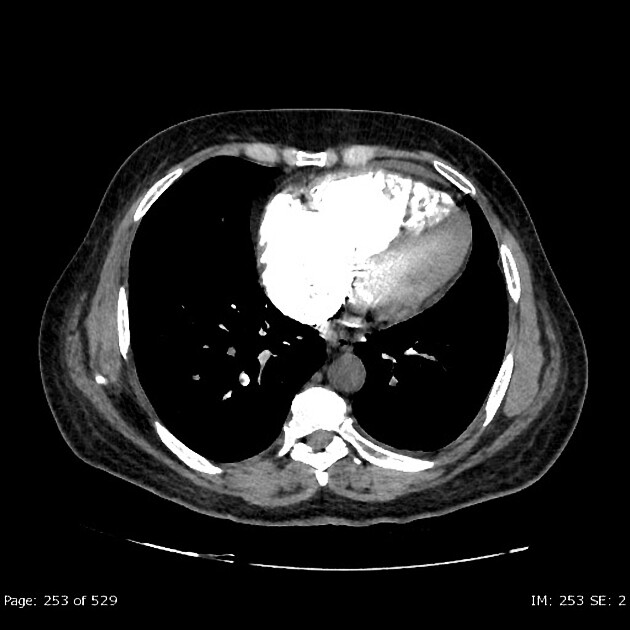
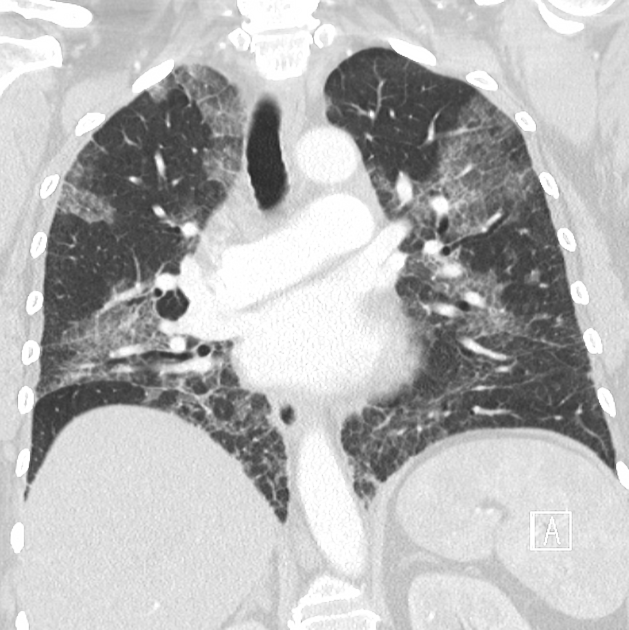
CT
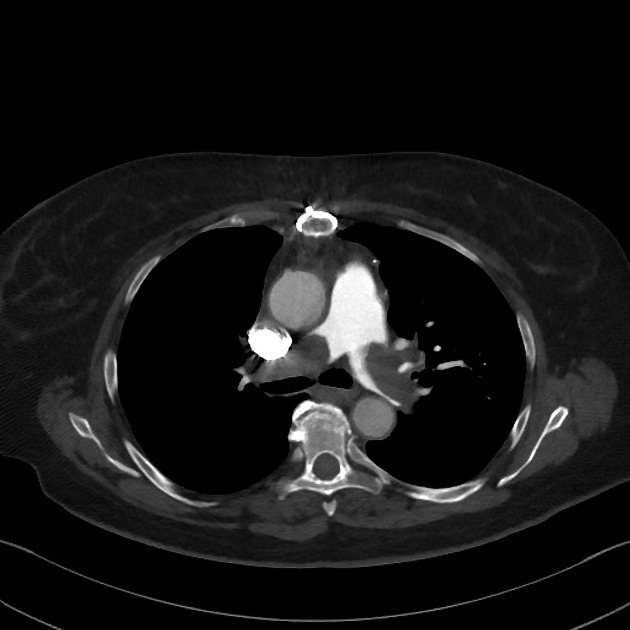
Acute pulmonary emboli
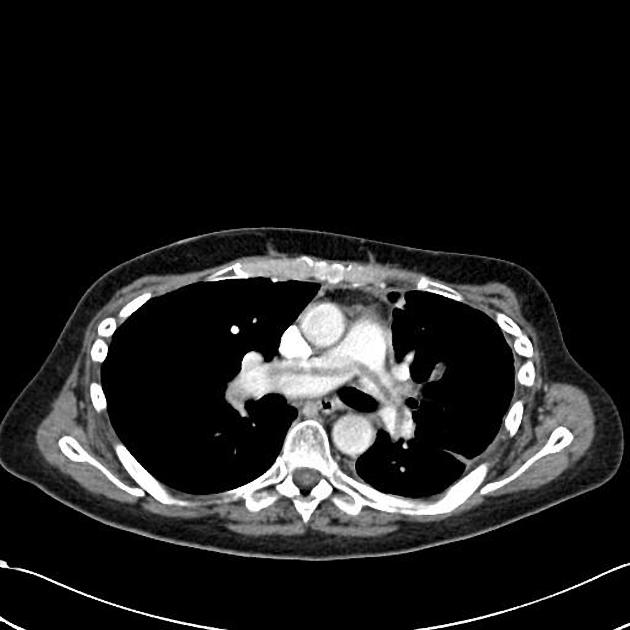
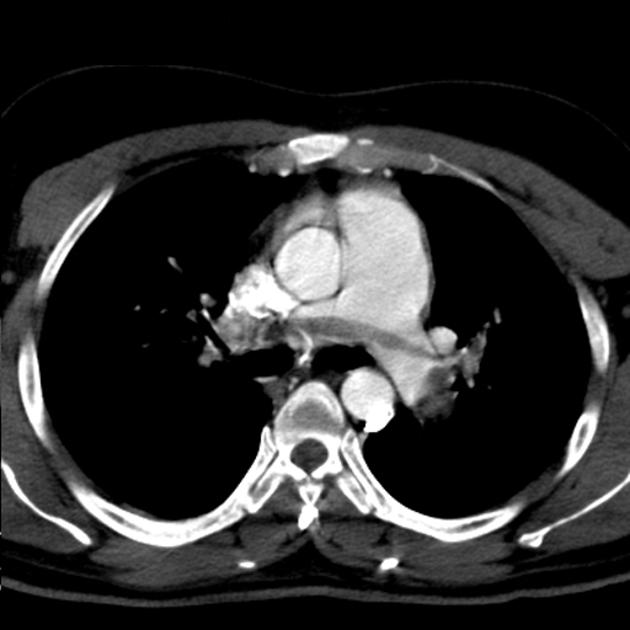
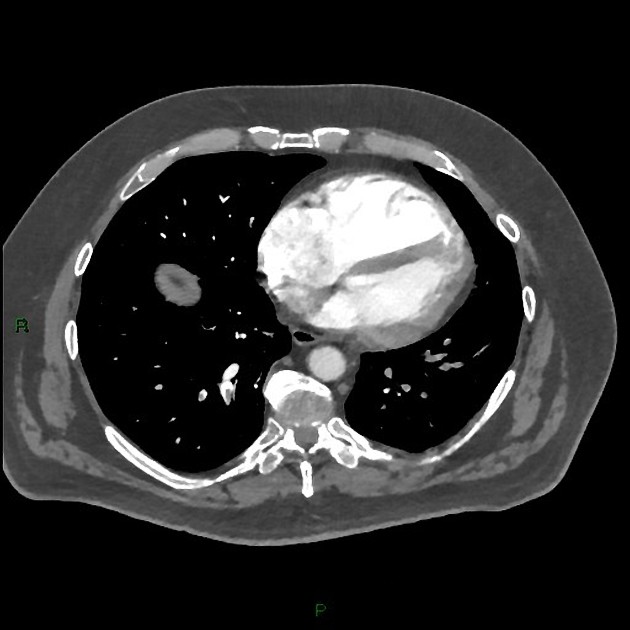
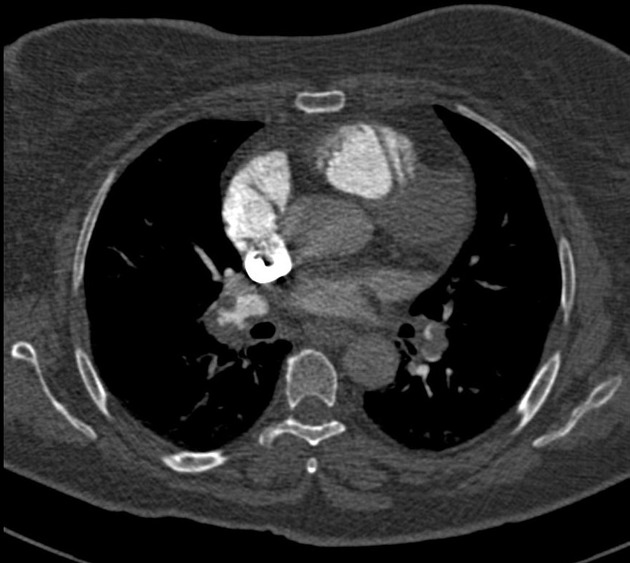
CT pulmonary angiography (CTPA) will show filling defects within the pulmonary vasculature with acute pulmonary emboli. When the artery is viewed in its axial plane the central filling defect from the thrombus is surrounded by a thin rim of contrast, which has been called the polo mint sign.
Emboli may be occlusive or non-occlusive, the latter is seen with a thin stream of contrast adjacent to the embolus. Typically the embolus makes an acute angle with the vessel, in contrast to chronic emboli. The affected vessel may also enlarge 9.
Acute pulmonary thromboemboli can rarely be detected on non-contrast chest CT as intraluminal hyperdensities 12.
Pulmonary infarction can occur when pulmonary artery branches < 3mm are occluded due to inadequate bronchopulmonary anastomoses at this level. Larger infarctions can occur with concomitant heart failure.
Dual-energy CT holds much promise for the diagnosis and prognosis of PE. Z effective and iodine maps provide lung perfusion assessment. The use of low monoenergetic reconstructions (low monoE) allows 'iodine boosting' of the pulmonary arteries which are useful during suboptimal contrast opacification thereby preventing the need to repeat undiagnostic scans ref.
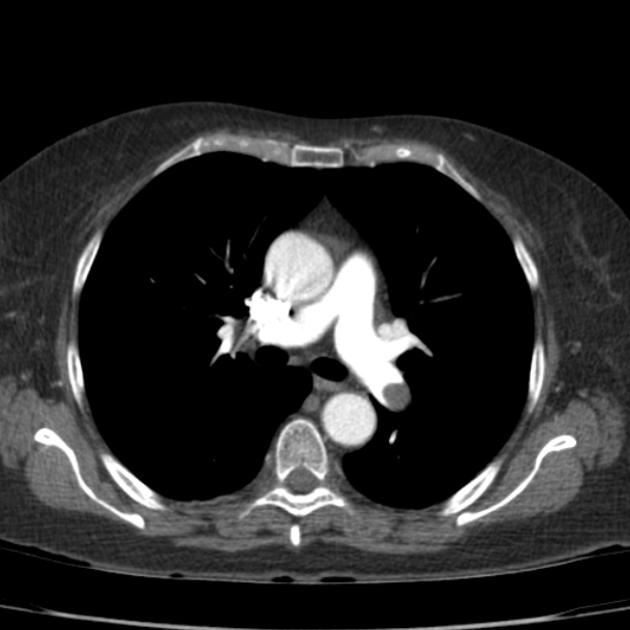
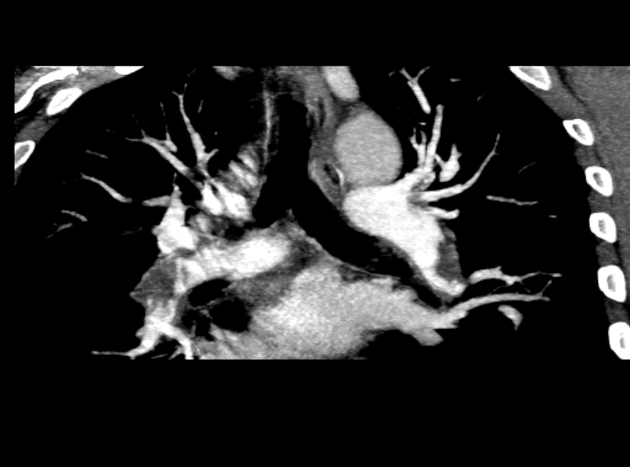
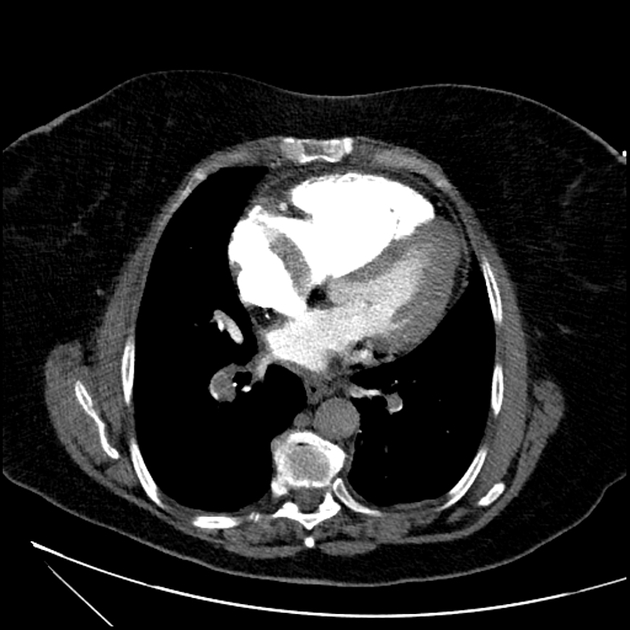
Chronic pulmonary emboli
In contrast to acute pulmonary embolism, chronic thromboemboli are often complete occlusions or non-occlusive filling defects in the periphery of the affected vessel which form obtuse angles with the vessel wall 9. The thrombus may be calcified.
Features noted with chronic pulmonary emboli include:
webs or bands, intimal irregularities 3
abrupt narrowing or complete obstruction of the pulmonary arteries 3
“pouching defects” which are defined as chronic thromboembolism organized in a concave shape that “points” toward the vessel lumen 3
Indirect signs include 7:
vascular calcification
bronchial or systemic collateralisation
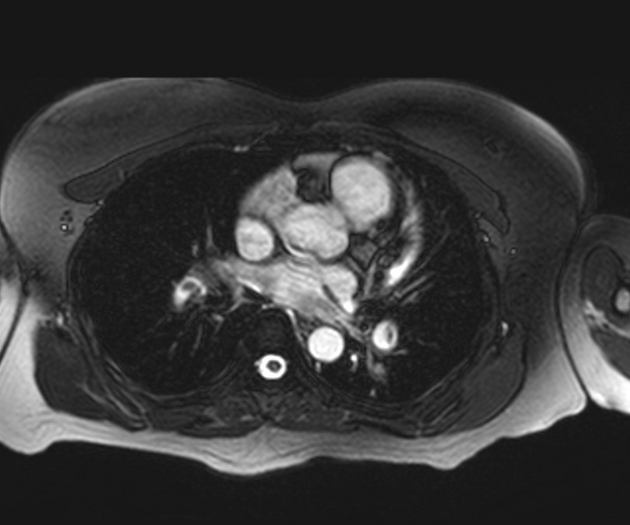
MRI
It is difficult to obtain technically adequate images for pulmonary embolism patients using MRI. Magnetic resonance pulmonary angiography (MRPA) should be considered only at centers that routinely perform it well and only for patients for whom standard tests are contraindicated. Technically-adequate magnetic resonance angiography has a sensitivity of 78% and a specificity of 99% 13.
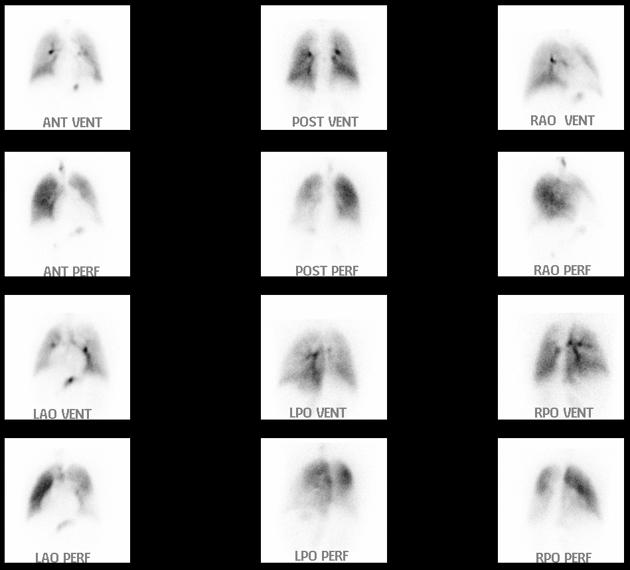
Nuclear medicine
A ventilation/perfusion (V/Q) scan will show ventilation-perfusion mismatches. A high probability scan is defined as showing two or more unmatched segmental perfusion defects according to the PIOPED criteria.
Treatment and prognosis
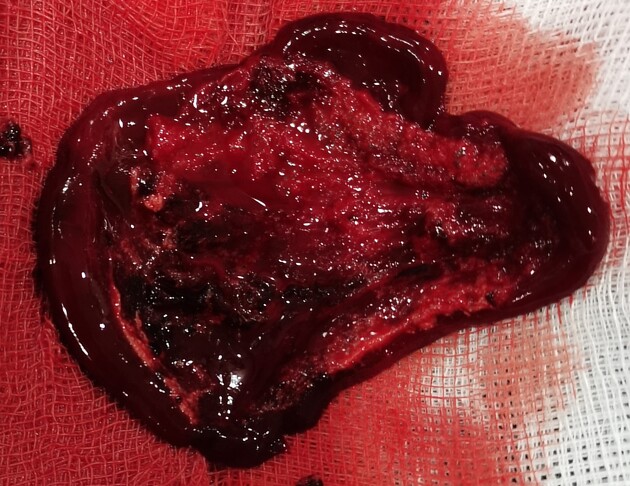
Providing cardiopulmonary support is the initial treatment. Anticoagulation is provided in patients without risk of active bleeding. If the emboli are large or there is a large clot burden, thrombolysis is an option. In some cases, embolectomy or placement of vena cava filters is required.
Anticoagulation treatment for subsegmental pulmonary embolism may be driven by considerations on recurrence risk, bleeding risk, and patient's preferences 34.
The right ventricular failure due to pressure overload is considered the primary cause of death in severe PE 14.
Complications
-
acute emboli
pulseless electrical activity (PEA) in the context of a large obstructing saddle embolus (see mnemonic for causes of PEA)
-
acute or chronic emboli
-
-
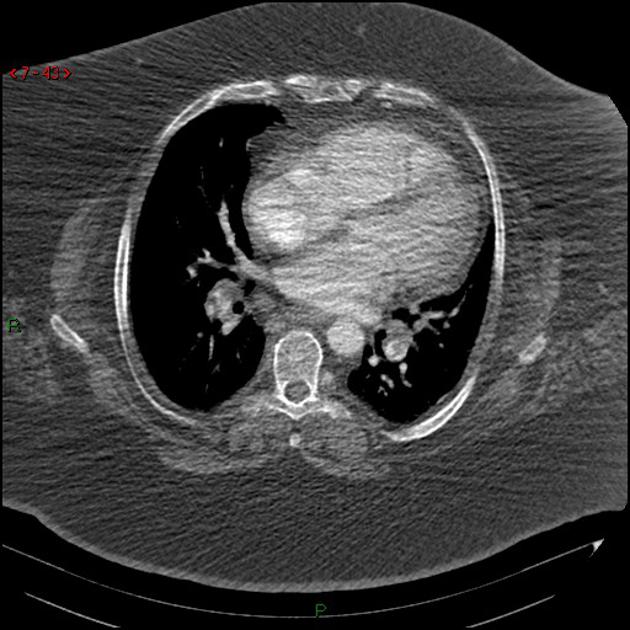
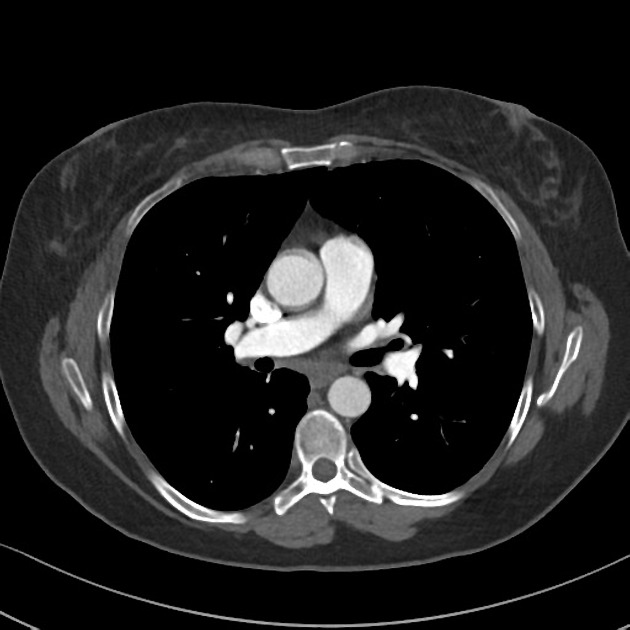
CT features suggestive of right ventricular dysfunction include 8:
abnormal position of the interventricular septum
inferior vena cava contrast reflux
-
RVD (right ventricular diameter): LVD (left ventricular diameter) ratio >1 on reconstructed four-chamber views
RVD:LVD ratio >1 on standard axial views is not considered to be a good predictor of right ventricular dysfunction 8
termed submassive PE when right ventricular dysfunction demonstrated on imaging (CT or echo) but without clinical hemodynamic compromise 19
-
-
-
subacute to chronic emboli
-
chronic emboli
Prognosis
Around 80% of emboli resolve at approximately 30 days 20,21. Residual pulmonary obstruction at 6 months after the first episode was shown to be an independent predictor of recurrent venous thromboembolism and/or chronic thromboembolic pulmonary hypertension 28.
History and etymology
It was first reported in the 1850s by the German physician and pathologist Rudolf Virchow 33.
Differential diagnosis
-
artifacts
contrast-blood level, due to slow flow
breathing motion
-
hyperconcentrated contrast in the superior vena cava
medical devices, e.g. catheters, orthopedic prostheses
patient's arms in a down position
transient contrast bolus interruption 16, due to Valsalva or a patent foramen ovale, causing non-opacified blood to enter the right ventricle and pulmonary arteries (scanning in end-expiration can reduce or eliminate this artifact)
-
iatrogenic
cavopulmonary anastomosis
-
neoplastic
-
inflammatory
-
interpretational
misidentification of pulmonary veins for arteries
arterial bifurcations (or branch points) - usually easily distinguished on multiplanar assessment
chronic emboli may be mistaken for acute emboli
thromboembolic emboli may be mistaken for other embolized material

















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.