Cerebral hemorrhagic contusions are a type of intracerebral hemorrhage, also sometimes considered a "brain bruise", and are common in the setting of significant head injury. They are usually seen on CT as hyperattenuating foci in the frontal lobes adjacent to the floor of the anterior cranial fossa and in the temporal poles.
On this page:
Epidemiology
Cerebral contusions result from blunt head trauma and are thus seen more frequently in young males. Typical causes include motor vehicle accidents or situations in which the head strikes the ground, such as falls in the elderly 9.
Associations
Pathology
Cerebral contusions occur due to rapid deceleration of the brain and collision against the inner surface of the skull (coup-contrecoup injury), accentuated by the natural irregular contours of the skull base (see below).
In the early phase, there is initially pericapillary hemorrhage and edema, followed by extravasation of hemorrhage through the cortex, white matter, and subarachnoid space. An inflammatory response to the injured tissue then occurs, characterized by abundant macrophages, ultimately resulting in a cavitated region of gliosis 10.
Chronic contrecoup contusions have a characteristic macroscopic appearance of retracted yellow-brown plaques due to the accumulation of hemosiderin. These plaques, also known as "plaque jaune", may be foci for subsequent epilepsy 10.
Location
Cerebral contusions can occur anywhere, but have a predilection for certain locations, as a result of the direction of the head strike and the intrinsic shape of the skull cavity:
Radiographic features
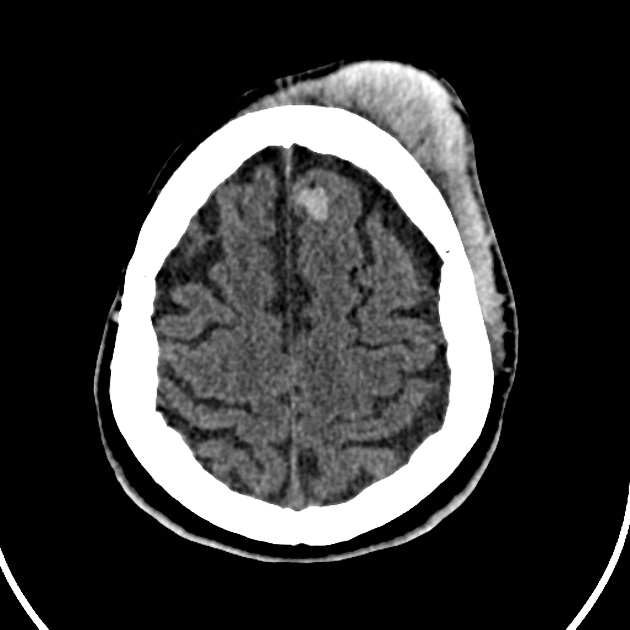
CT
CT is usually the first and often only investigation used to assess cerebral contusions. It has a high sensitivity in the acute phase 12.
Contusions vary in size and can appear as small punctate hyperdense foci involving the grey matter and subcortical white matter, or as large hyperdense cortical or subcortical hematomas. These lesions are typically surrounded by regions of white matter hypodensity reflecting vasogenic edema 12.
Small or occult contusions may only become apparent on follow-up imaging due to further hemorrhage or surrounding edema 11. A follow-up CT within 1-2 days is usually performed, which may detect an increase in the number and size of the lesions, typically also reflected by the clinical deterioration of the patient 11.
Contusions eventually fade over a number of weeks, leaving behind distinct areas of gliosis.
NB: the Hounsfield unit (HU) of blood is dependent on the hemoglobin concentration (i.e. hematocrit). With a normal hematocrit of 45%, the density of blood is 45-65 HU (grey matter is 37-41 HU, and white matter is 30-34 HU). Therefore, acute blood appears hyperdense compared to grey or white matter. However, in anemic patients, acute blood may appear isodense.
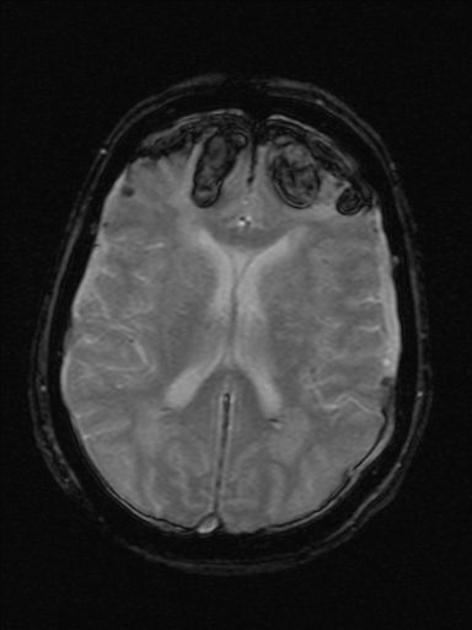
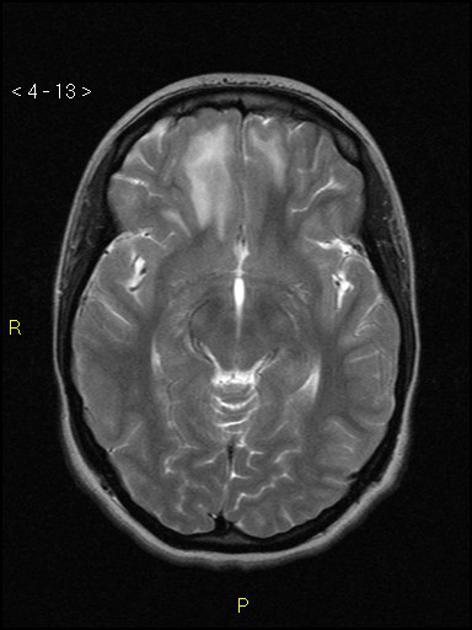
MRI
Although not typically used to assess cerebral contusions, MRI is far more sensitive to small contusions after the first 24 hours compared to CT, especially on T2* sequences, e.g. SWI 3,12.
T1: high signal intensity
-
T2: low signal intensity (except during the late subacute phase where it is hyperintense due to extracellular methemoglobin 5)
FLAIR may show hyperintense edema surrounding "occult" contusions
T2*/SWI: low signal intensity and blooming artifact 8
MRI imaging characteristics in hemorrhage are dependent on the sequence and age of the blood.
Differential diagnosis
-
cerebral contusions undergo expected evolution of blood products whereas cavernomas stay stable or re-bleed
look for an associated developmental venous anomaly (DVA)
Practical points
a potential pitfall is missing a small contusion near the skull base, which can be overlooked on CT due to partial volume averaging











 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.