Colorectal cancer (CRC) is the most common cancer of the gastrointestinal tract and is one of the most frequently diagnosed malignancies in adults. CT is the mainstay for colon cancer locoregional staging and MRI is the mainstay for rectal cancer locoregional staging.
This article focuses on colon cancer. See also, the rectal cancer standalone article.
On this page:
Epidemiology
Colorectal cancer is common, accounting for 15% of all newly diagnosed cancers, and tends to be a disease of the elderly, with the median age of diagnosis between 60 and 80 years of age 2, slightly younger for rectal cancer. There is also a slight male predilection for rectal cancers, not found in tumors elsewhere in the colon.
Risk factors
Many predisposing factors have been identified, including:
low fiber, and high fat and animal protein diet
obesity: especially in men
-
inflammatory bowel disease (IBD)
Crohn disease (particularly in bypassed loops/in the vicinity of chronic fistula)
asbestos exposure
a family history of benign/malignant colorectal tumors
history of endometrial/breast cancer
pelvic irradiation
ureterosigmoidostomy
dysplasia of colon within flat mucosa
prominent lymphoid follicular pattern
Associations
Syndromes
Recognized hereditary syndromes are seen in 6% of colorectal cancers ref. These include:
Clinical presentation
Clinical presentation is typically insidious:
altered bowel habit (constipation and/or diarrhea)
iron-deficiency anemia (chronic occult blood loss)
However initial manifestation may be acute:
Less common presentations include:
that of metastatic disease (e.g. respiratory symptoms from lung metastases)
paraneoplastic syndromes (e.g. dermatomyositis)
bacteremia or bacterial endocarditis with Streptococcus bovis (Streptococcus gallolyticus) 6
In general:
right-sided tumors are larger and present with a mass, distant disease or iron deficiency anemia
left-sided tumors present earlier with altered bowel habit
Pathology
Colorectal cancers, 98% of which are adenocarcinomas, arise in the vast majority of cases from pre-existing colonic adenomas (neoplastic polyps), which progressively undergo a malignant transformation as they accumulate additional mutations 2 (so-called multi-hit hypothesis).
Morphologically cancers can be:
sessile
exophytic
circumferential (apple core)
ulcerated
desmoplastic
Rarely the malignant cells will widely invade the submucosa, analogous to linitis plastica of the stomach. These are typically scirrhous adenocarcinomas (signet-ring type).
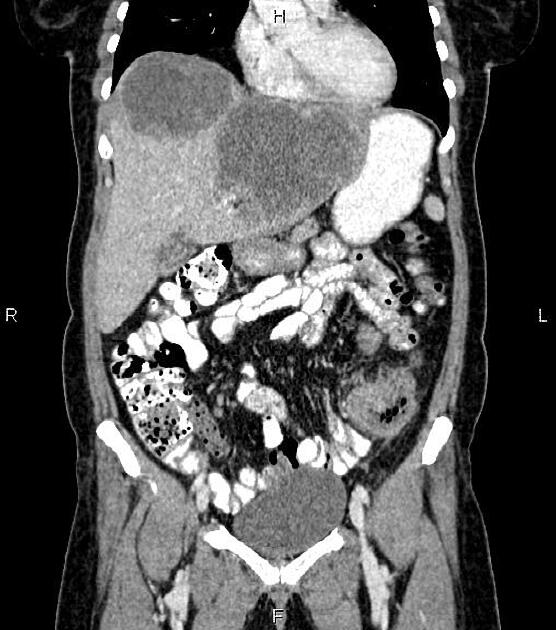
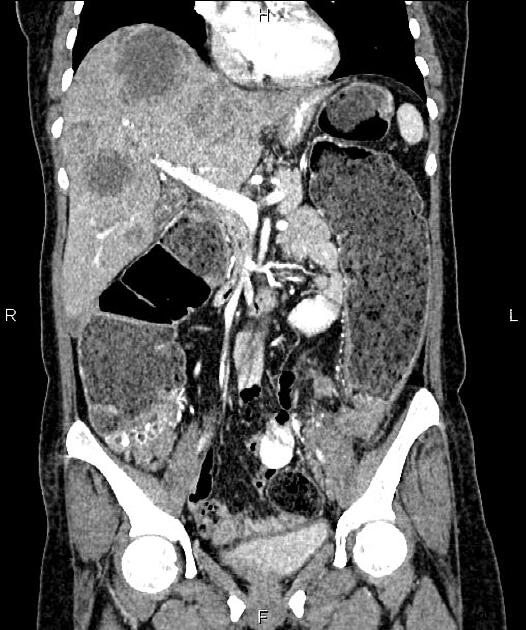
Metastases may be widespread in advanced disease, although the liver is by far the most common site involved.
Specific subtypes
Location
Colorectal cancers can be found anywhere from the cecum to the rectum, in the following distribution 2,5:
rectosigmoid: 55%
-
cecum and ascending colon: ~20%
ileocecal valve: 2%
transverse colon: ~10%
descending colon: ~5%
Genetics
Approximately 10% of colorectal cancers have a BRAF mutation, which is more common in females, right colon colorectal cancer, advanced stage at diagnosis, and a mucinous histology 7.
Staging
See: colon cancer staging.
Radiographic features
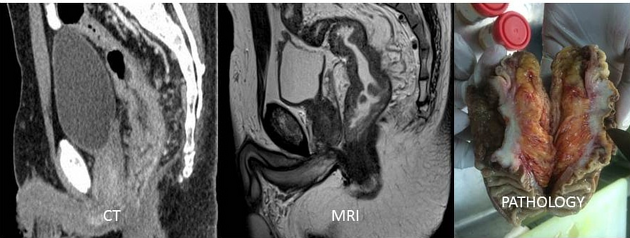
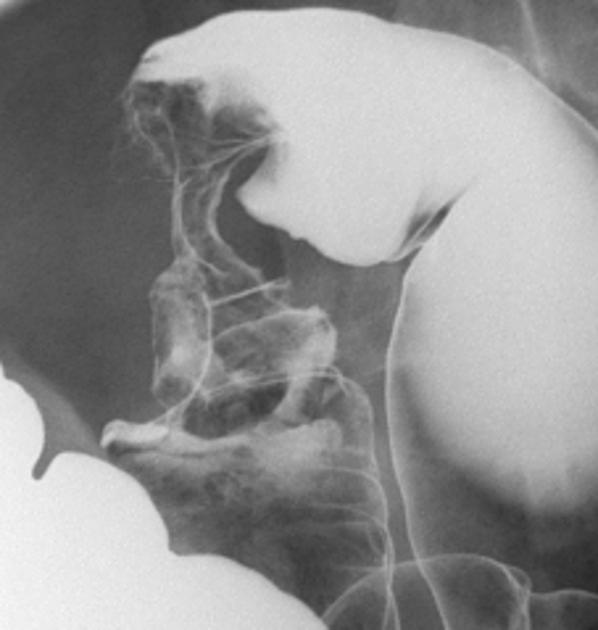
Fluoroscopy
Barium enema
-
sensitivities for polyps >1 cm
single contrast: 77-94%
double-contrast: 82-98%
polyps <1 cm: <50% detection 3
Appearances will reflect macroscopic appearance, with lesions seen as filling defects. These need to be differentiated from residual fecal matter. Typically they appear as exophytic or sessile masses or maybe circumferential (apple core sign). Fistulas to bladder, vagina, or bowel may also be demonstrated.
Rarely the stenotic segment will be long particularly with scirrhous adenocarcinomas.
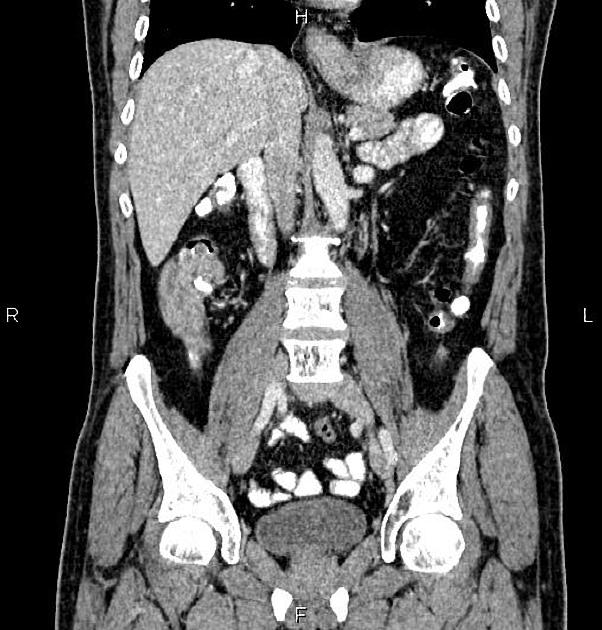
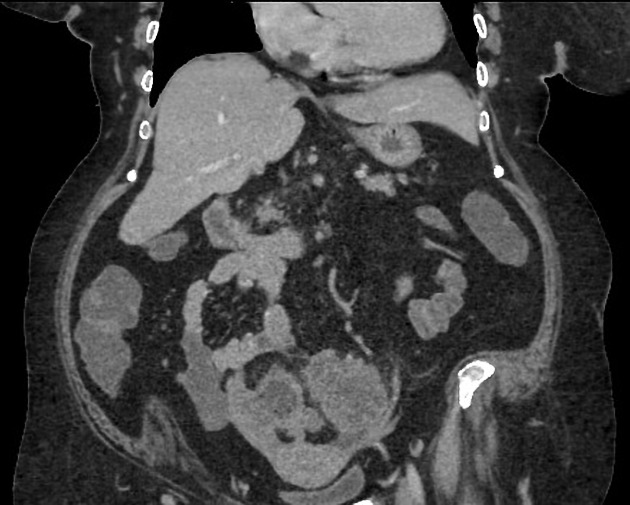
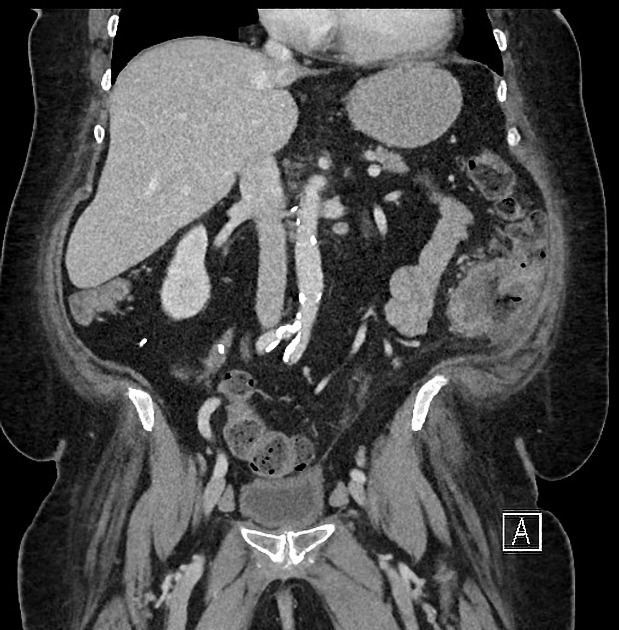
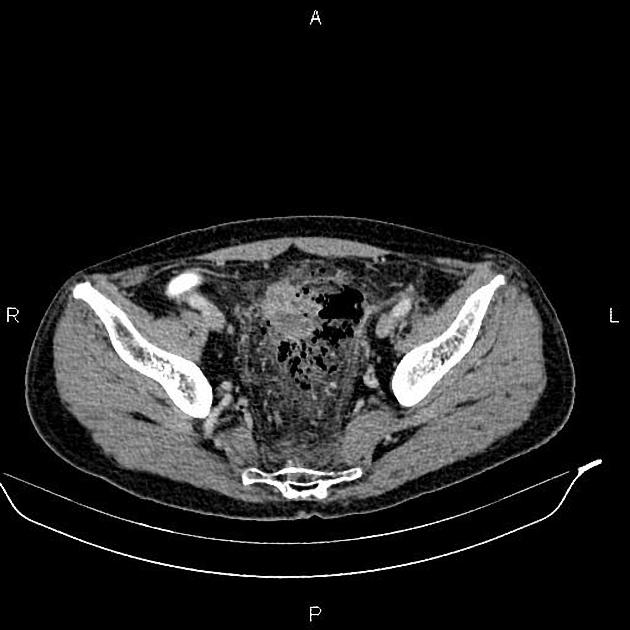
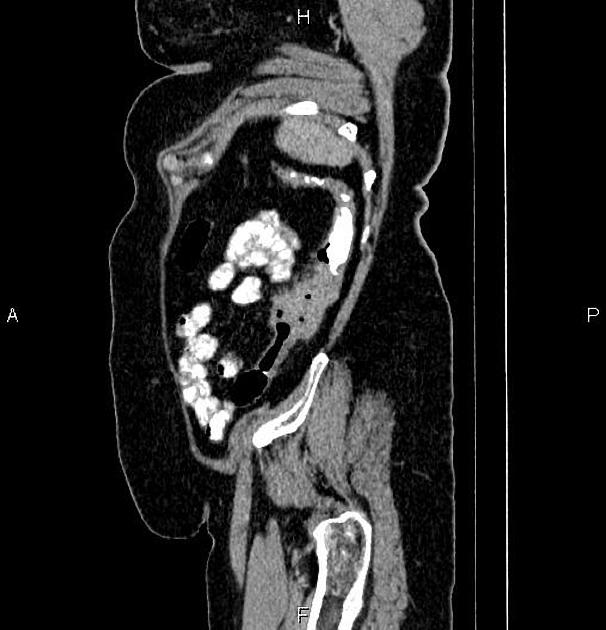
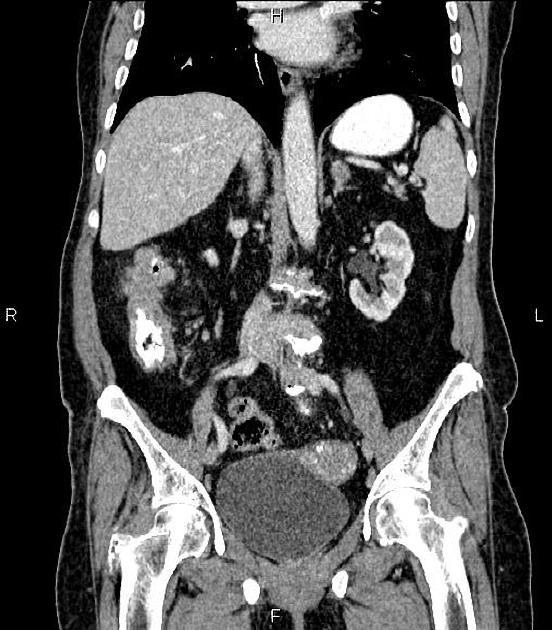
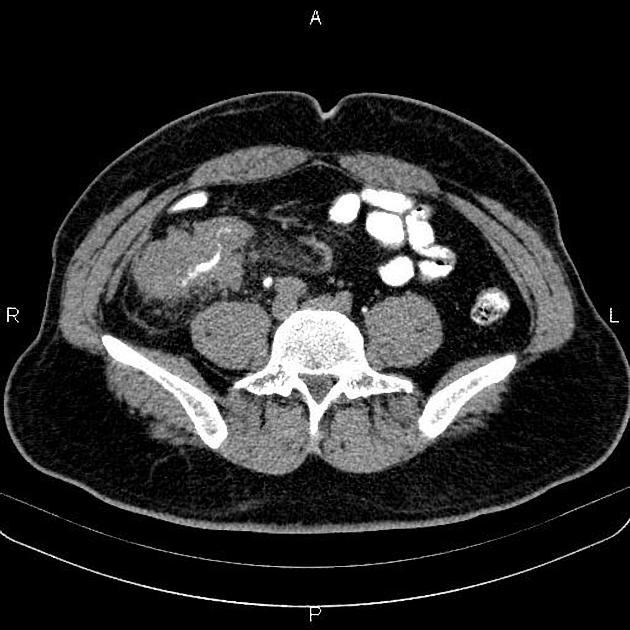
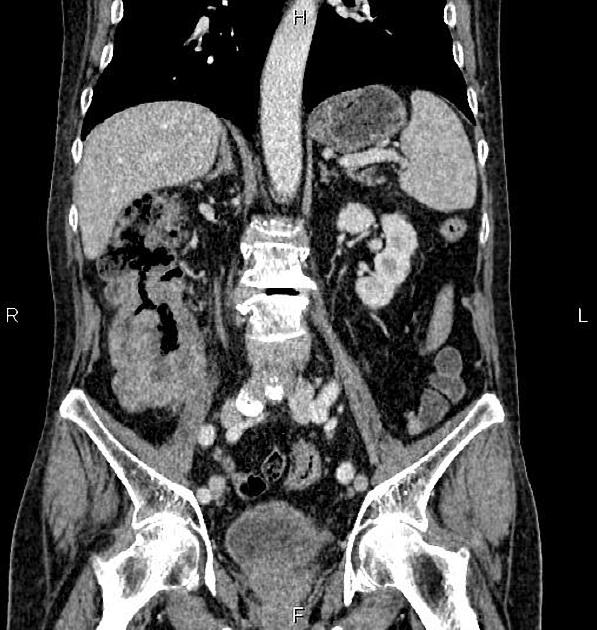
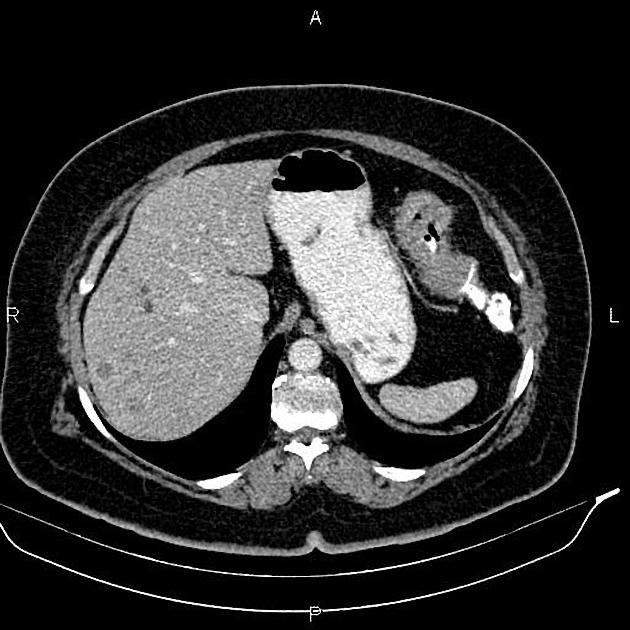
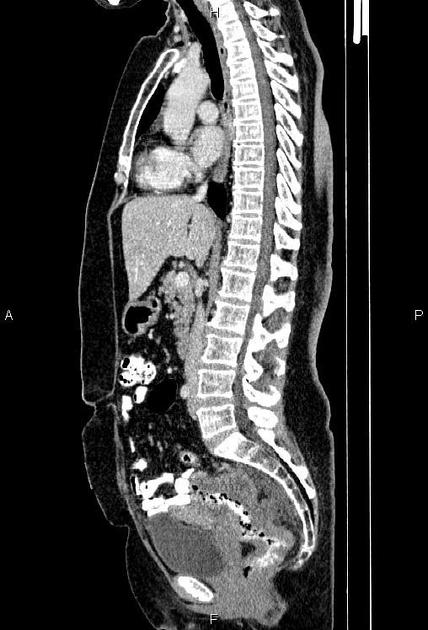
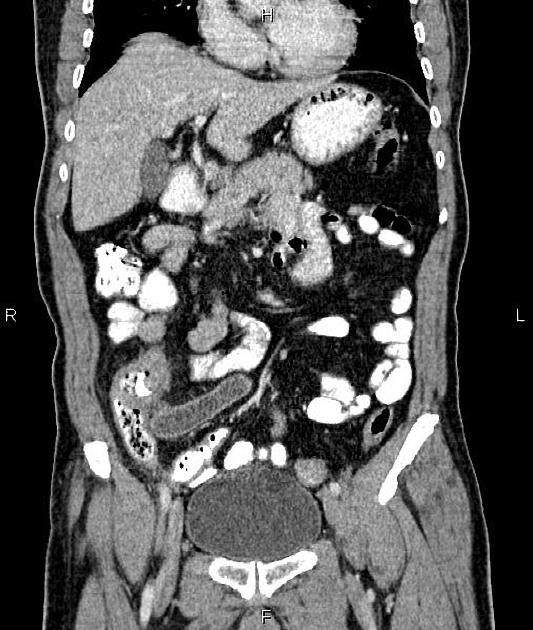
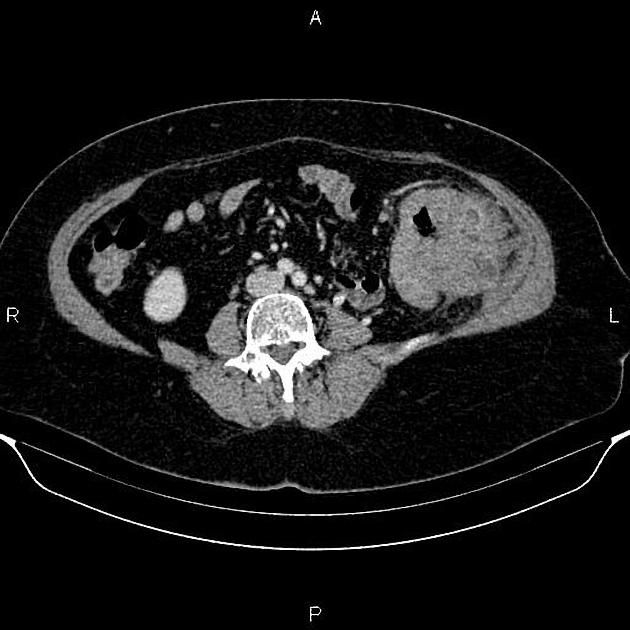
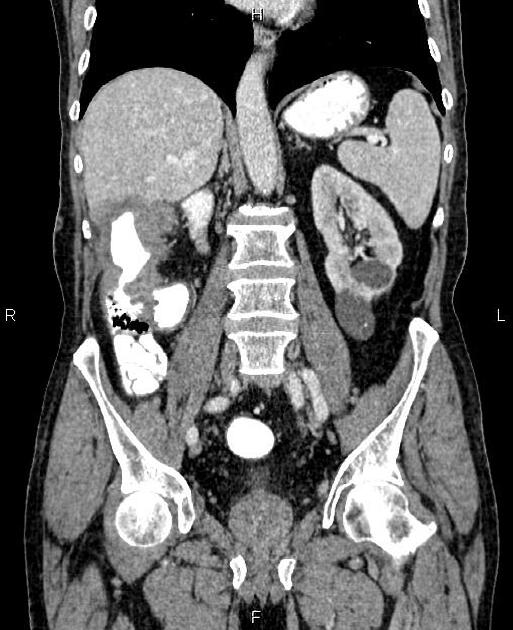
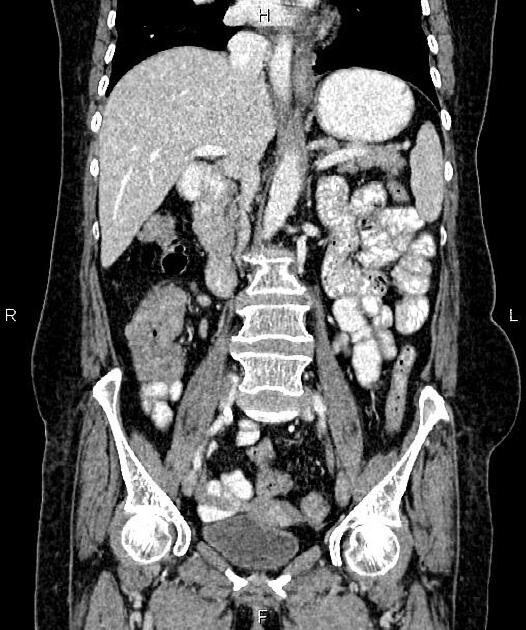
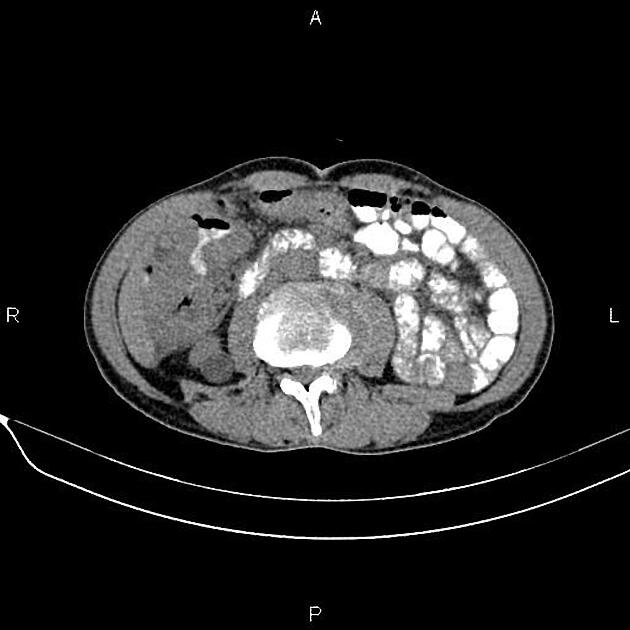
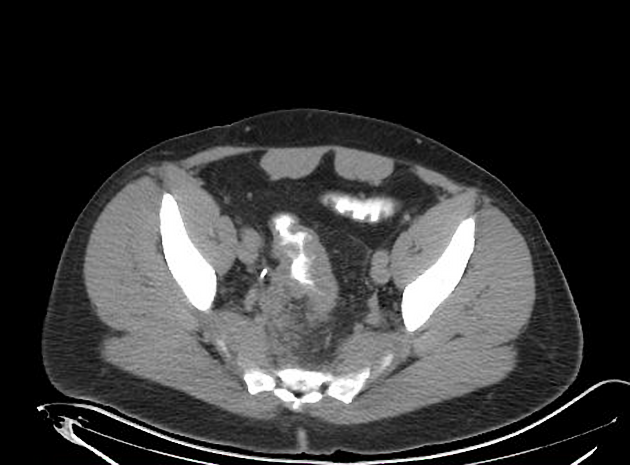
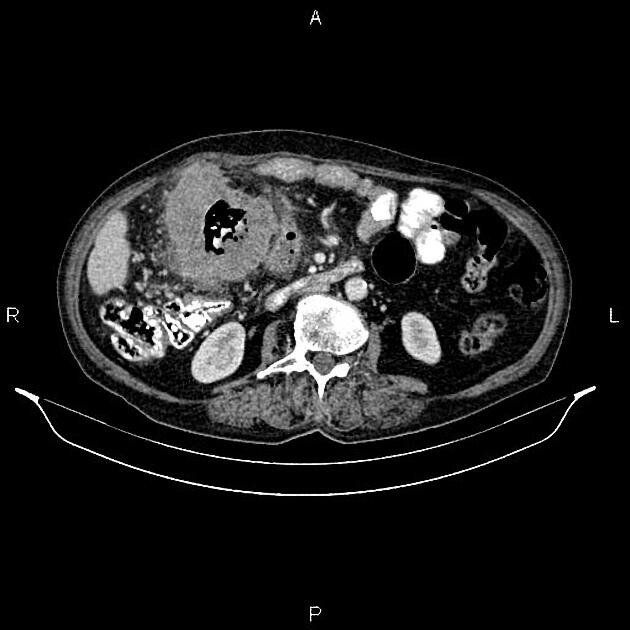
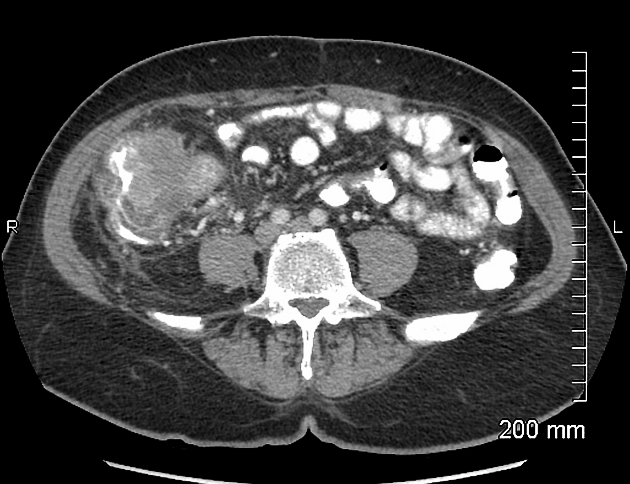
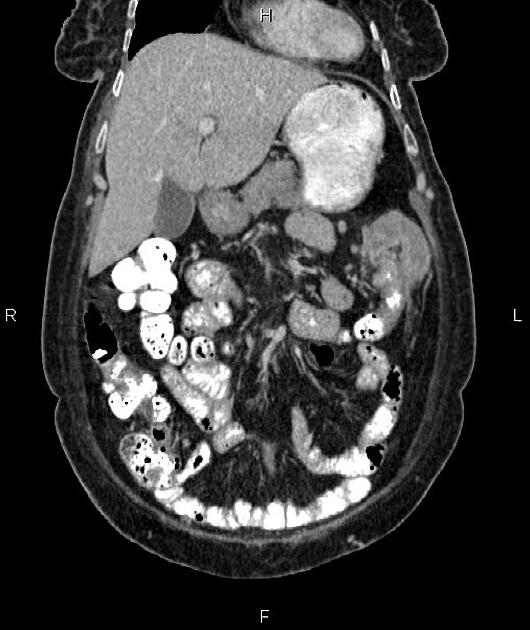
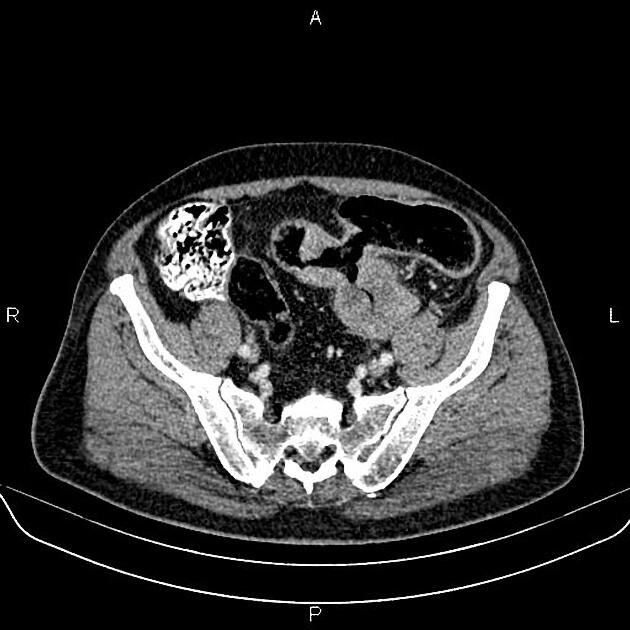
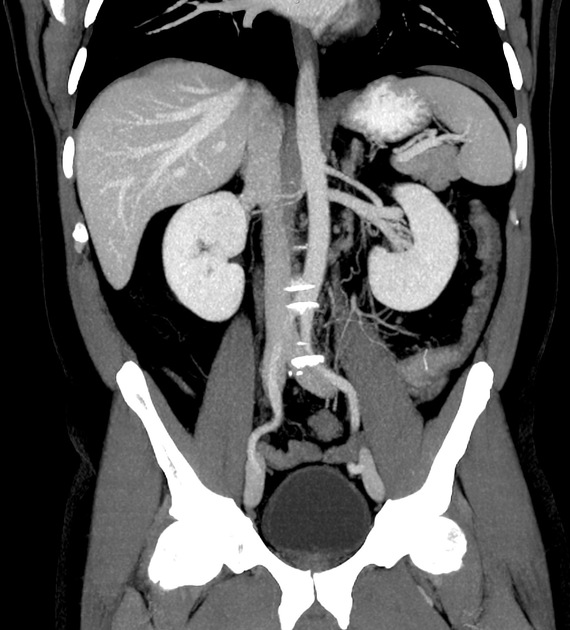
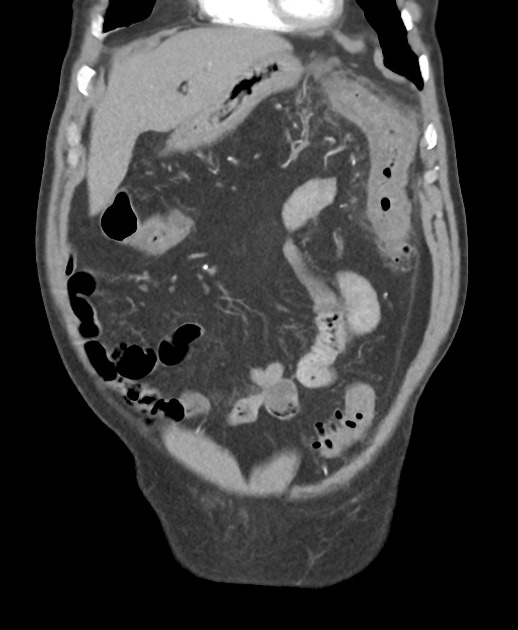
CT
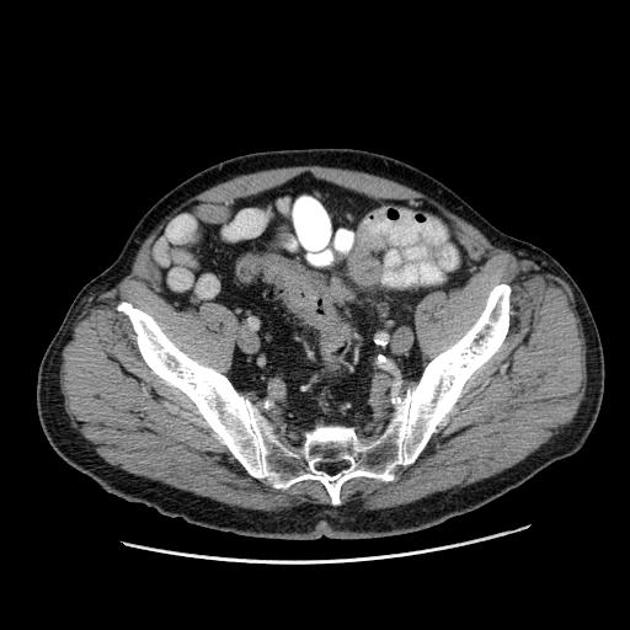
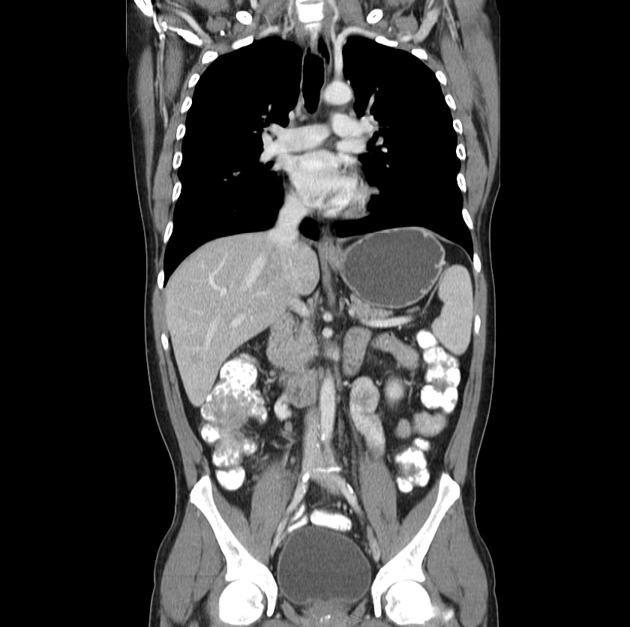
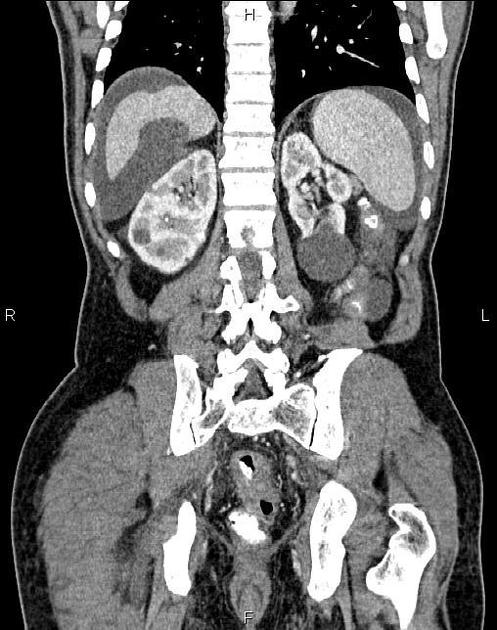
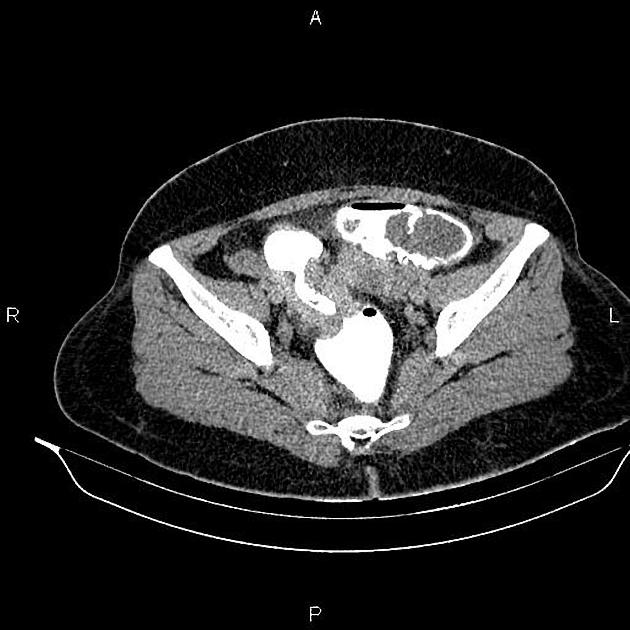
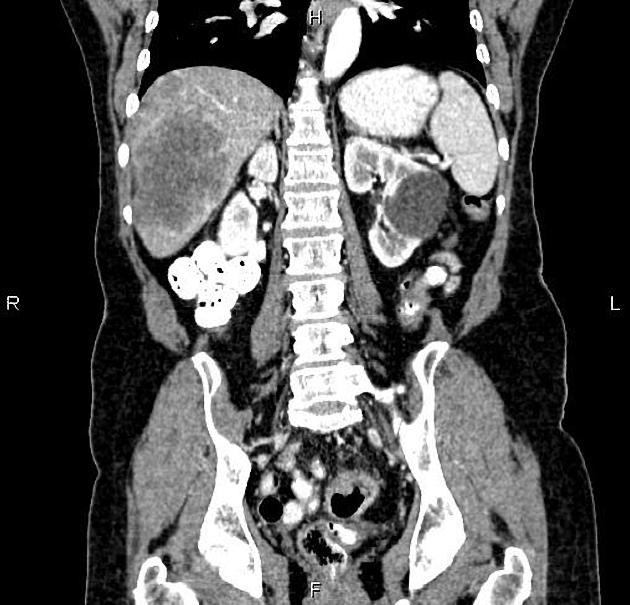
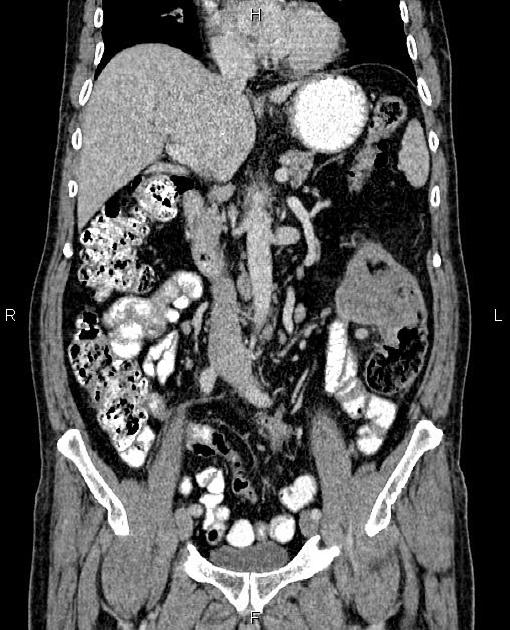
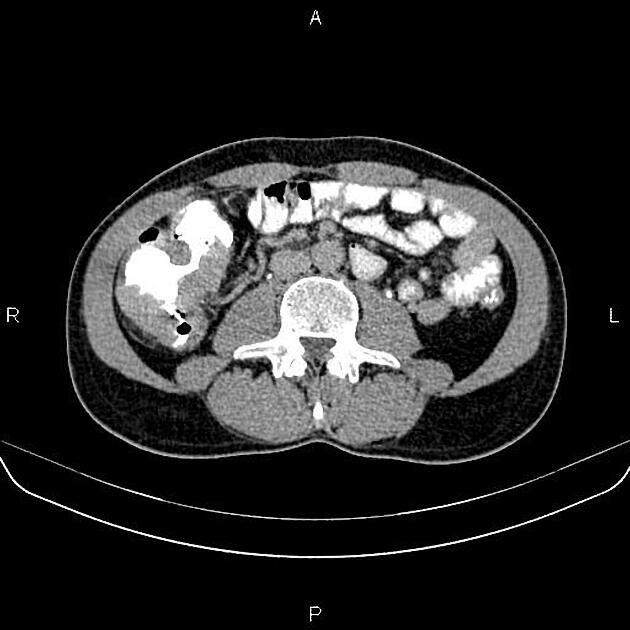
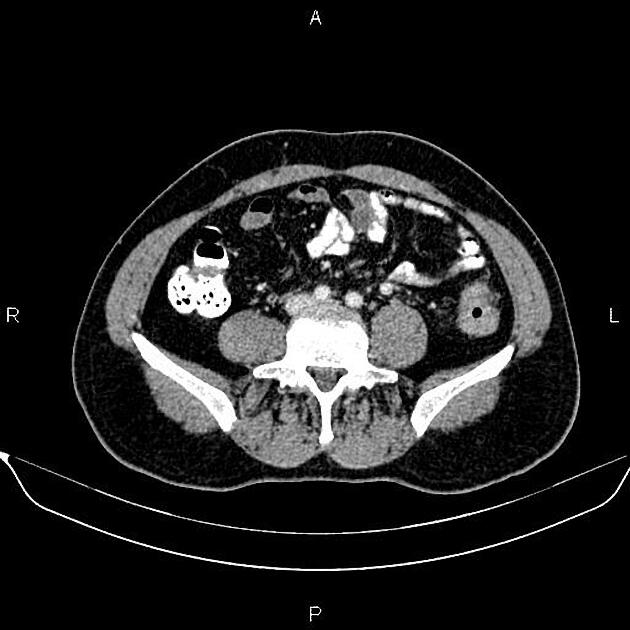
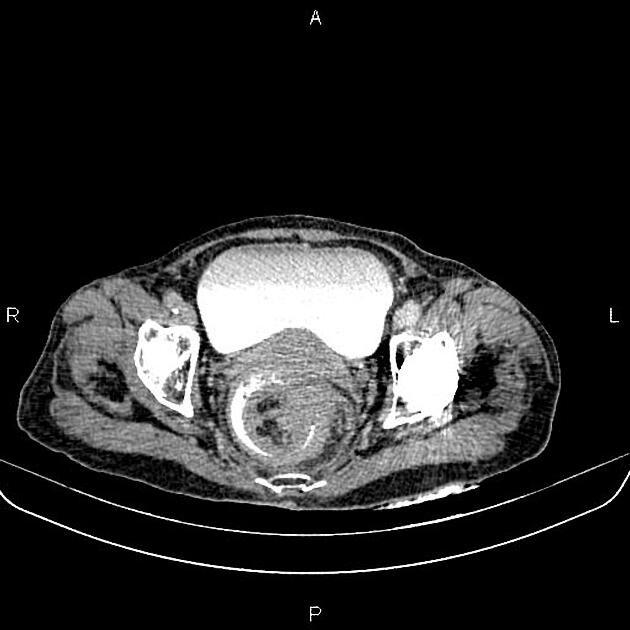
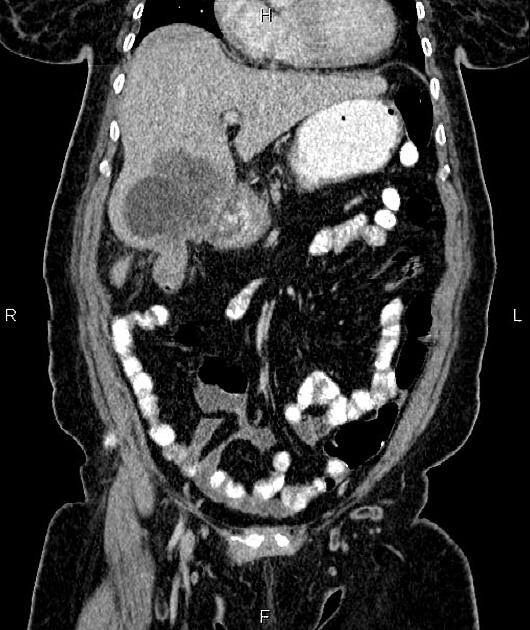
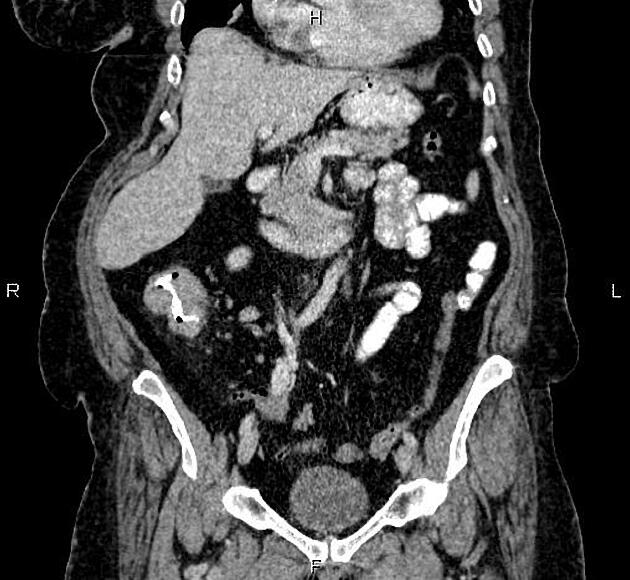
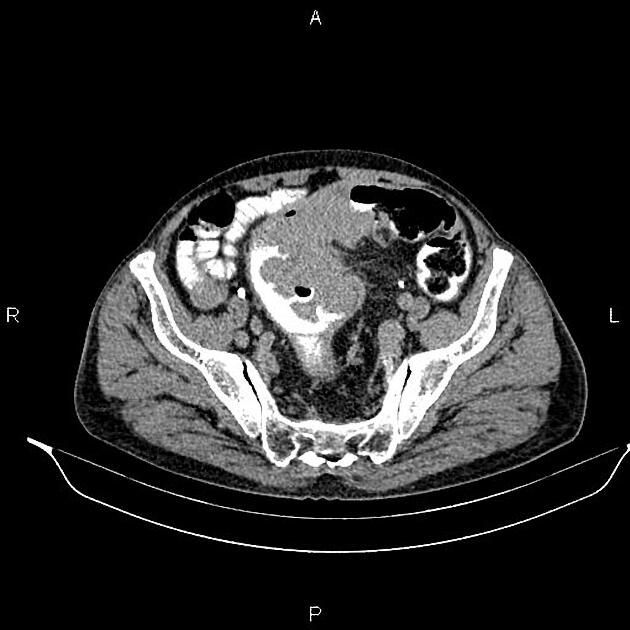
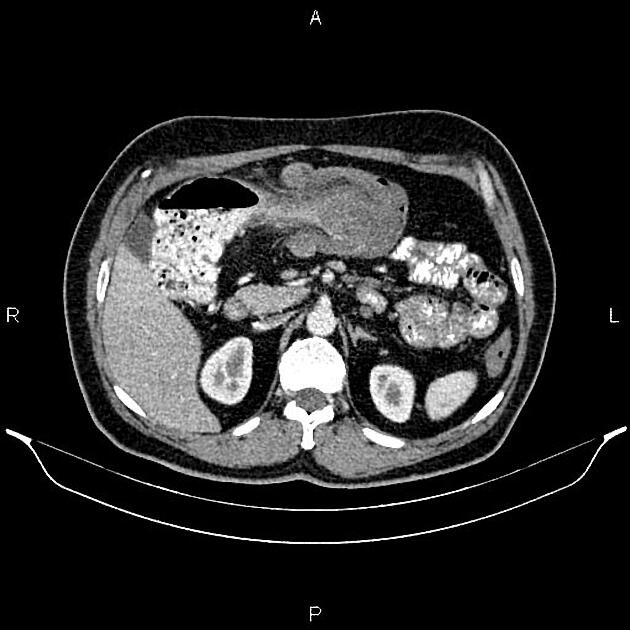
Contrast enhanced CT of chest, abdomen and pelvis is used for locoregional staging of colon cancer, identification of metastatic disease, assessment for suitability of surgical or other interventions, and assessing treatment response 9. CT fails to identify ~15% (range 10-20%) of subsequently proven colon cancers 13.
Most colorectal cancers are of soft tissue density that narrow the bowel lumen 4. Ulceration in larger masses is also seen. Occasionally low-density masses with low-density lymph nodes are seen in mucinous tumors. Psammomatous calcifications in mucinous adenocarcinoma can also be present.
Findings such as fat stranding, dilated vasa recta, and enlarged lymph nodes are helpful secondary features to identify colon cancers 13.
Complications may also be evident, e.g. fistula, obstruction, intussusception, perforation 4.
Staging
T-staging of CRC with CT is limited by soft tissue resolution with a sensitivity of 77% (range 61-87%) and specificity of 70% (range 49-89%), although accuracy can be improved by the use of multidecetctor CT, multiplanar reformats (MPR), and thin (0.6-1.5 mm) slices 9,10,12. The main use of CT is differentiating early disease (T1-T3ab) with <5 mm of extramural extension from advanced disease (T3cd/4) disease >5 mm of extramural extension as neoadjuvant therapy can be indicated for the latter 10-13.
Other important prognostic factors such as tumor deposits and extramural venous invasion (EMVI) can be detected on CT. The latter is best done on a portal venous phase 14.
Similarly, N-staging of CRC also suffers from relatively poor accuracy (positive predictive value ~60%) as normal, inflammatory (reactive), and malignant nodes can have a similar appearance 9,12. Indicators of nodal disease include size >10 mm alone or >5 mm along with internal heterogeneous density and/or irregular borders 12,13, and nodal clustering near the tumor or supplying vessels but none are proven strongly as diagnostic criteria 12.
M-staging of distant nodal disease and haemotogeneous metastases can also be performed with CT 12.
MRI
MRI is the primary modality for the locoregional staging of rectal cancer, as well as in the assessment of potentially resectable liver metastases 9.
Treatment and prognosis
Early-stage colon cancer standard treatment is surgical resection of the primary tumor and regional lymph nodes, which may be followed by adjuvent chemotherapy for stage 2 disease depending on individual risk factors 12. Adjuvant chemotherapy is recommended for stage 3 disease 12.
BRAF-mutated colorectal cancer has a poorer prognosis with a median survival of <12 months 7.
Recurrence is common:
local recurrence at the site of anastomosis: tend to occur within two years of diagnosis (80%) 4
The tumor marker carcinoembryonic antigen (CEA) is routinely used for detecting postoperative early recurrence and metastatic disease (especially liver disease). It is also used for monitoring response to treatment of metastatic disease.
as with most tumor markers, it is inappropriate for screening given its poor sensitivity and specificity
-
higher levels of CEA are associated with:
higher grade tumors
higher stage disease
visceral metastases (especially liver metastases)
Screening recommendations
Screening recommendations are contentious and vary widely from country to country. An example would be ref:
for persons >50 years of age: an annual fecal occult blood test (often a fecal immunochemical test (FIT)) and sigmoidoscopy/barium enema every 3 to 5 years
for first-degree relatives of patients with colon cancer: screening should start at age 40
Differential diagnosis
Diverticulosis
On CT colonography, the two most useful discriminators of colorectal carcinoma and diverticular disease are absence of diverticula within the affected segment, and shouldered edges, with both features having a high negative and positive predictive value for carcinoma 8. Other features favoring carcinoma include a shorter segment length, destroyed mucosal folds, straightening of the segment, absence of thickened fascia, and more and larger locoregional nodes.
Other imaging differential considerations on CT include:









































 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.