Fibrous dysplasia (FD) is a developmental benign medullary fibro-osseous process characterized by the failure to form mature lamellar bone and arrest as woven bone that can be multifocal. It can affect any bone and occur in a monostotic form involving only one bone or a polyostotic form involving multiple bones. Since the WHO classification of soft tissue and bone tumors (5th edition) it has been titled a benign bony neoplasm.
Fibrous dysplasia accounts for the "F" in the popular mnemonic for lucent bone lesions FEGNOMASHIC.
This article is confined to the monostotic (involves a single bone) and polyostotic (multiple bones are involved) forms. Craniofacial fibrous dysplasia and cherubism are discussed in separate articles.
On this page:
Terminology
Terms such as "liposclerosing myxofibrous tumor" and "fibrocartilaginous dysplasia" are no longer recommended 1.
Epidemiology
Fibrous dysplasia is uncommon, occurs in children and adults and can affect all age groups 1,2. It is usually first diagnosed in children and young adults. The true incidence is not known but it is estimated to make up for ~5% of benign bone lesions 3,4. There is no gender predilection 1.
Associations
Although fibrous dysplasia is usually sporadic, a number of associations are well recognized 4,5:
McCune-Albright syndrome: in 2-3% of cases with the polyostotic form
-
isolated endocrinopathy without the full McCune-Albright syndrome precocious puberty in girls
Cushing syndrome: osteoporosis, acne
growth restriction
Mazabraud syndrome: soft-tissue myxomas (rare); typically multiple intramuscular lesions in the vicinity of most severely affected bone
Diagnosis
The diagnosis of fibrous dysplasia is mainly based on clinical and typical radiographic features 1 and if the imaging features are characteristic the lesion does not require histology 5,6.
Histological confirmation is indicated in cases with atypical imaging appearance or in isolated monostotic lesions with clinical symptoms or other concerning features 5,6. Typical asymptomatic lesions are followed-up with serial radiographs to rule out significant mechanical implications and assure biological inactivity 5.
Diagnostic criteria
Diagnostic criteria according to the WHO classification of soft tissue and bone tumors (5th edition) 1:
Essential features include 1:
a bone lesion with compatible imaging characteristics
osseous part consisting of irregular curvilinear branching trabeculae of woven bone without apparent osteoblastic rimming
fibrous part consisting of bland fibroblasts
The following additional criterion is desirable:
evidence of GNAS activating missense mutations
Clinical presentation
The condition is often an incidental finding and is usually painless. Alternatively, it may present with bony expansion and remodeling or with pain 1,2. Morbidity may arise from pathologic fracture 4 or compression and displacement of adjacent structures. The latter is particularly true in craniofacial fibrous dysplasia, where the content of the orbit or cranial nerves may be compressed resulting in loss of vision or hearing loss 4.
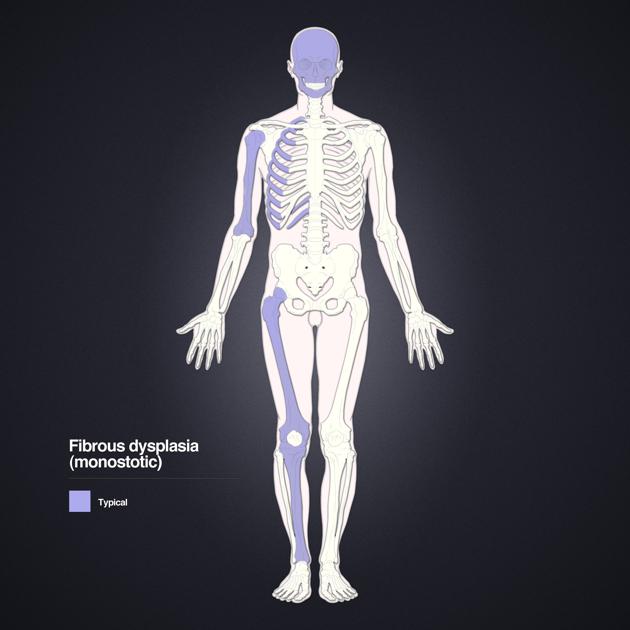
Monostotic form
The monostotic form is far more common accounting for 70-80% of cases and is usually asymptomatic until the 2nd to 3rd decade but can be seen throughout adulthood 7. After puberty, the disease can become inactive.
Polyostotic form
The polyostotic form accounts for 20-30% and presents earlier, typically in childhood with about 60% showing symptoms before the age of 10 years 2.
Pathology
Fibrous dysplasia is characterized by altered osteogenesis leading to an intramedullary fibro-osseous proliferation with fibrous and osseous tissue components being present in varying degrees 1. It comes in a monostotic or polyostotic form depending on whether only one single bone or multiple bones are affected. However, there is no progression from the monostotic to the polyostotic form 5.
Etiology
Fibrous dysplasia is linked to postzygotic activating missense GNAS mutations that encode the alpha subunit of the stimulatory G-protein 1-5.
Location
Monostotic form
ribs: 28%, most common 7,8
proximal femur: 23%
tibia
craniofacial bones: 10-25% 9
humerus
Polyostotic form
often unilateral and monomelic: one limb 7
femur: 91%
tibia: 81%
pelvis: 78%
foot: 73%
ribs
skull and facial bones: 50% 9
upper extremities
lumbar spine: 14%
clavicle: 10%
cervical spine: 7%
Subtypes
There are no officially recognized subtypes 1.
Macroscopic appearance
Macroscopically, lesions are intramedullary, well-circumscribed, and often expansile with abnormal whitish or tannish-grey color and gritty consistency. Cystic changes might be present, especially in older lesions. Rarely cartilage might be found characterized by a blue-tinged translucent appearance 1,2.
Microscopic appearance
Microscopically fibrous dysplasia is characterized by the following 1,2,4,7:
varying proportions of fibrous and osseous tissue
fibrous tissue principally made up of bland spindle cells without conspicuous cellular atypia
irregular curvilinear branching trabeculae of woven bone with a pattern that has been characterized as “looking like Chinese characters” 2,4
absence of osteoblastic rimming
uncommon mitoses unless there is a fracture
Other possible histological features include 1,2:
cementum-like bone deposition
rounded psammomatous calcifications
islands of benign hyaline cartilage might rarely be seen
possibly aneurysmal bone cyst-like changes
The absence of osteoblastic rimming aids in the differentiation from the cemento-ossifying fibroma.
Genetics
In about 50-70%, GNAS activating missense mutations can be detected in particular involving pArg201His and pArg201Cys 1,4.
Radiographic features
General imaging features of fibrous dysplasia are 7:
intramedullary, expansile lesion
well-defined borders
maintenance of a smooth cortical contour
endosteal scalloping might be present
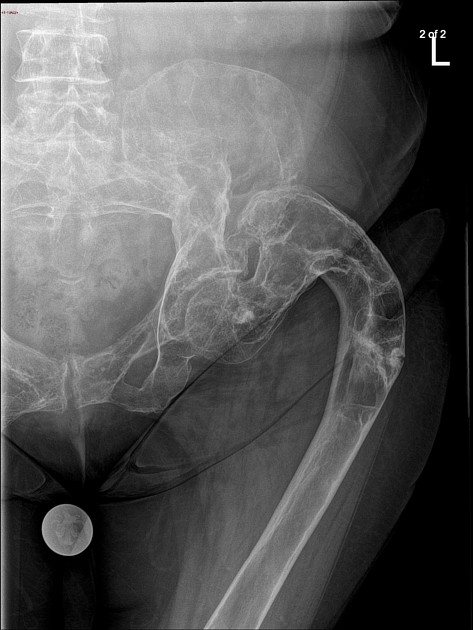
Plain radiograph
Fibrous dysplasia can generally display the following three main imaging features 5:
cystic/lucent
sclerotic
mixed
Beyond that, appearances are usually smooth and homogeneous with endosteal scalloping and cortical thinning 5. The borders are well defined and the cortex is usually intact but thinned due to the expansive nature of the lesion 5. Other features include:
ground-glass matrix
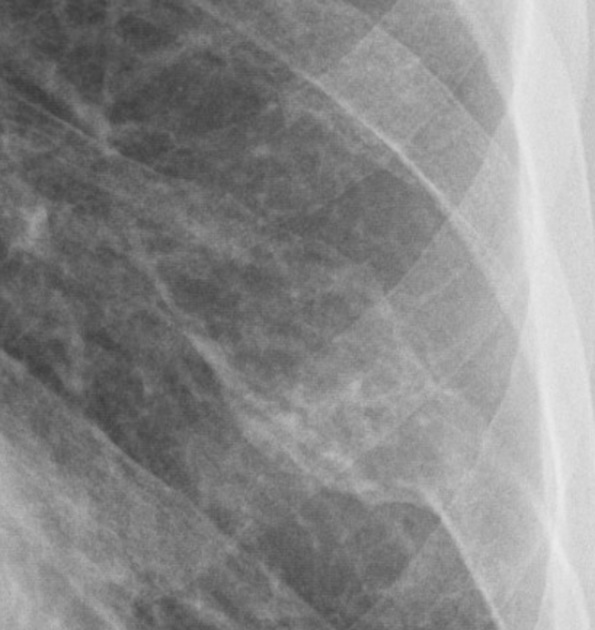
Pelvis and ribs
Ribs are the most common site of monostotic fibrous dysplasia. Fibrous dysplasia is the most common cause of a benign expansile lesion of a rib (see rib lesions)
bubbly cystic lesions
fusiform enlargement of ribs
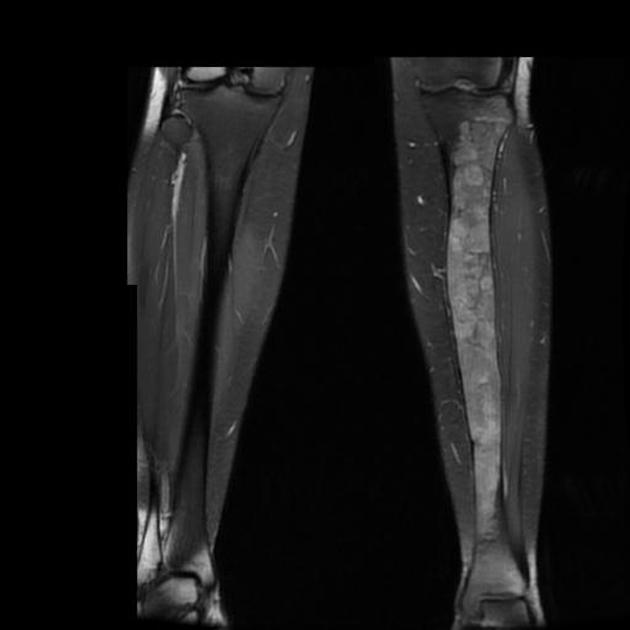
Extremities
may lead to premature fusion of growth plates leading to short stature
bowing deformities
shepherd crook deformity of the femoral neck
discrepant limb length
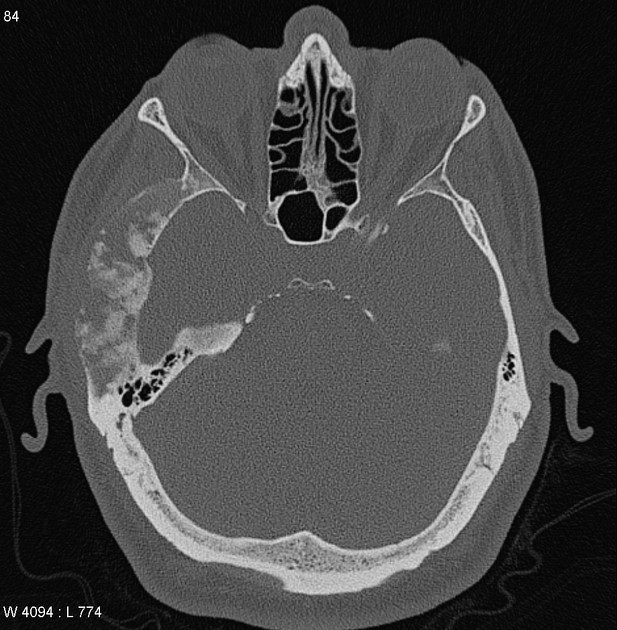
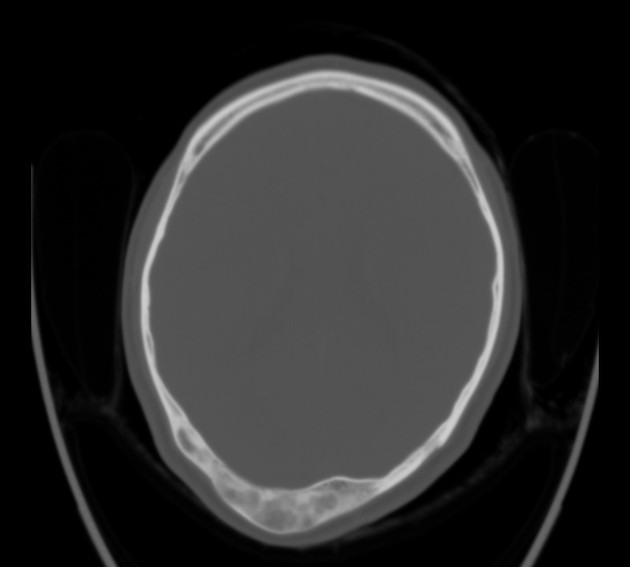
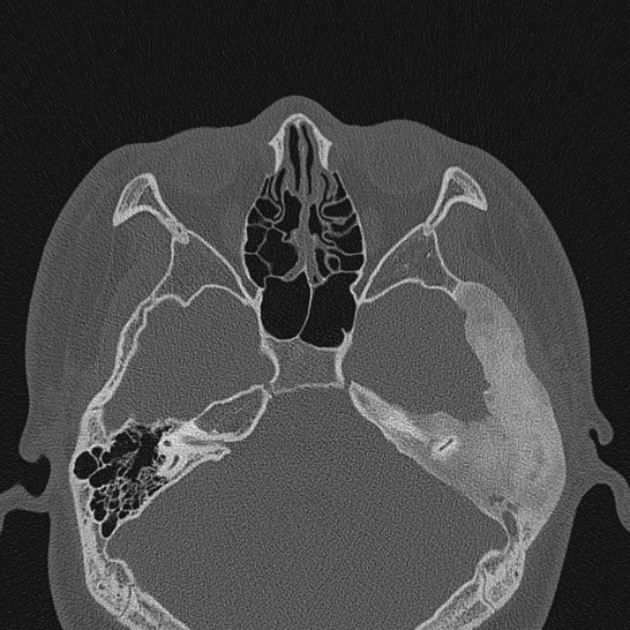
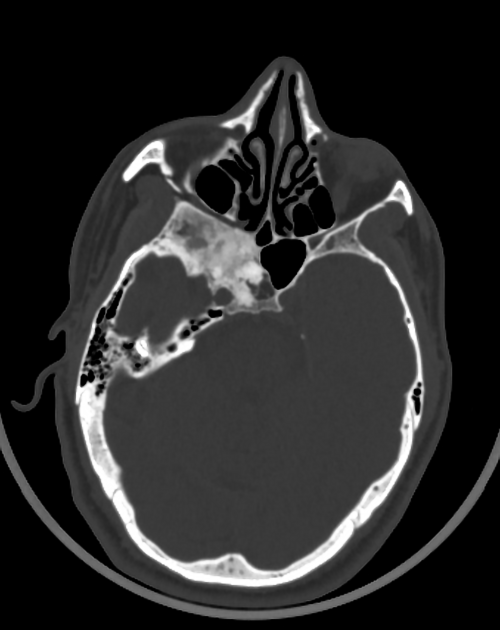
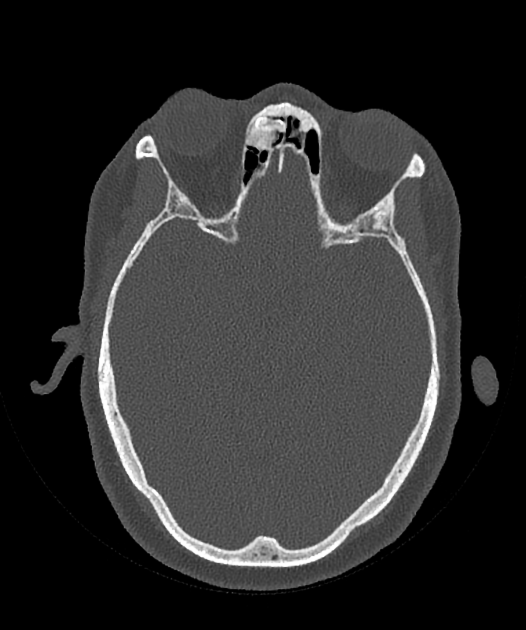
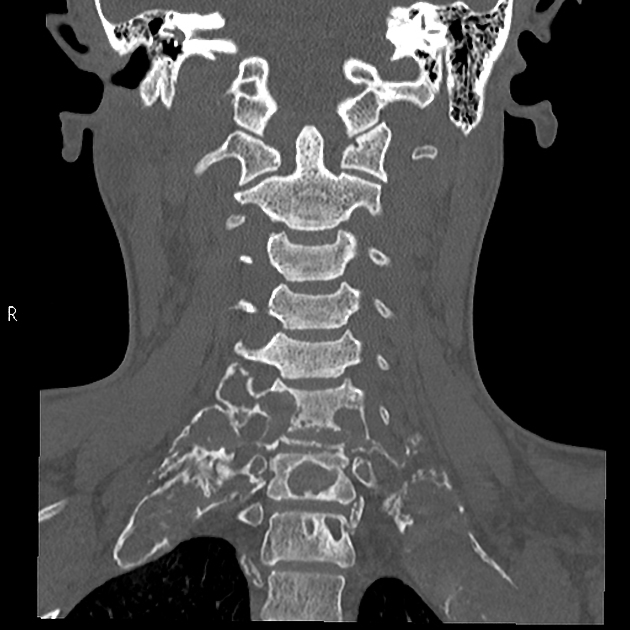
CT
CT better delineates morphological osseous changes of bone and is considered the modality of choice in the evaluation of fibrous dysplasia, especially in the setting of craniofacial lesions 5. CT imaging features include:
ground-glass opacities: 56% 9
homogeneously sclerotic: 23%
cystic: 21%
well-defined borders
expansion of the bone, with intact overlying bone
endosteal scalloping may be seen 7
The attenuation of lesions usually ranges from 60-140 HU and they usually enhance after the application of contrast media 5.
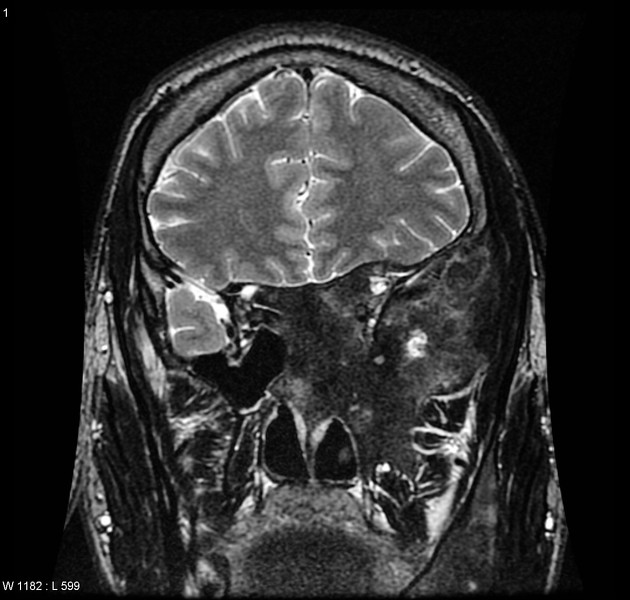
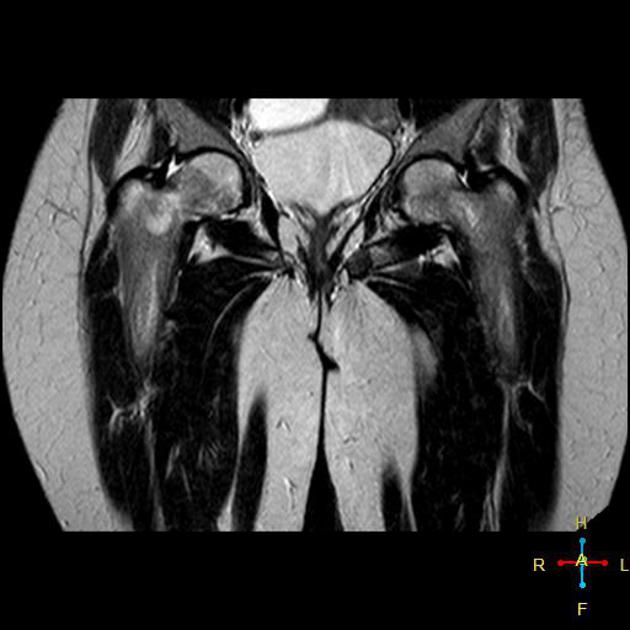
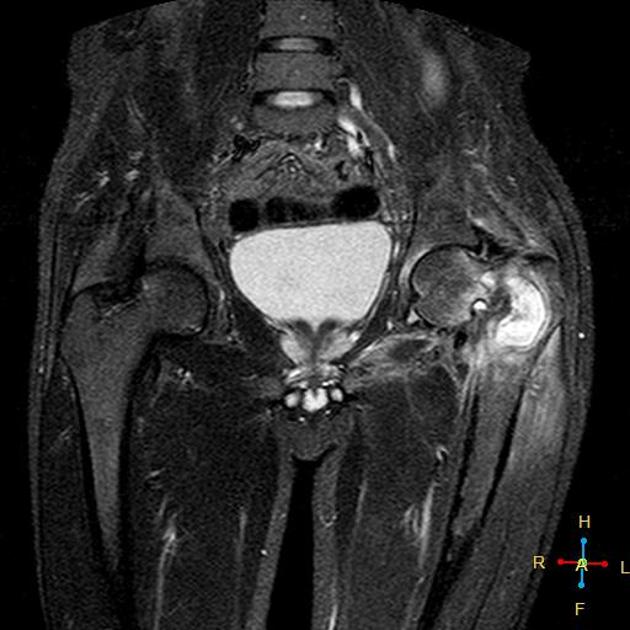
MRI
MRI is not particularly useful in differentiating fibrous dysplasia from other entities as there is marked variability in the appearance of the bone lesions, and they can often resemble a tumor or more aggressive lesions.
T1: usually intermediate to low heterogeneous signal 5
T2: variable signal 10
T1 C+ (Gd): heterogeneous moderate to avid contrast enhancement 9,10
Nuclear medicine
Demonstrates increased tracer uptake on Tc99 bone scans (lesions remain metabolically active into adulthood).
Radiology report
The radiological report should include a description of the following 5,6:
location and size
tumor margins and transition zone
-
signs of benign matrix transformation 5:
aneurysmal bone cyst-like changes
myxoid changes
-
concerning features suggestive of malignant matrix formation 5
cortical destruction
aggressive periosteal reaction
surrounding bone marrow edema
solid mass-like enhancement
soft tissue extension
-
additional associated findings 5:
If features are typical the lesion can be categorized as Bone-RADS 1 on CT or MRI 6.
Treatment and prognosis
Management aims to establish the extent of the disease and the maintenance of bone quality via dietary measures and exercise. The prognosis is excellent and usually, no other treatment is required 1.
However monostotic fibrous dysplasia can lead to deformities leg-length differences and impingement or nerve compression syndromes 1. If a mass effect is severe, then surgery excision may be considered 4,5.
Complications
Not surprisingly, bone affected by fibrous dysplasia is weaker than normal and thus susceptible to pathological fractures.
Sarcomatous dedifferentiation (most commonly osteosarcoma 12, fibrosarcoma, undifferentiated pleomorphic sarcoma, or rarely chondrosarcoma) is occasionally seen (<1%) and is more common in the polyostotic form. It should be noted that many reported cases may relate to previous treatment with radiation therapy 7.
History and etymology
Fibrous dysplasia was first described by the American bone pathologist Louis Lichtenstein in 1938 and the clinical, radiological and histological spectrum of findings were later characterized by him and his colleague Henry Louis Jaffe in 1942 13,14.
Differential diagnosis
Due to the variability of the appearance of fibrous dysplasia the potential differential is very long but will be significantly influenced by the dominant pattern.
-
mosaic pattern bone histologically
radiographically may be similar
different demographics
-
osseous lesions are rare
the vertebral column is the primary target
ribbon ribs
other features of the disease usually present
-
almost exclusively in the tibia with anterior bowing
the lesion begins in the cortex
usually seen in children <10 years
-
80% seen in the tibia
may appear indistinguishable
hemangioma 11


































 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.