Multiple biliary hamartomas (MBH) are a rare cause of multiple benign hepatic lesions. The condition is also known as von Meyenburg complexes, multiple bile duct hamartomas, or biliary microhamartomas. Multiple biliary hamartomas are asymptomatic and usually found incidentally. It is important to differentiate them from other causes of multiple liver lesions, particularly metastases.
On this page:
Epidemiology
The prevalence of multiple biliary hamartomas is ~3% at autopsy 1, however, prevalence on imaging is <1% as most hamartomas are <5 mm in size and often remain undetected. Multiple biliary hamartomas are reportedly three times more common in women than men 2.
Associations
Multiple biliary hamartomas are known to be associated with:
Several case reports have suggested possible malignant transformation of biliary hamartomas into cholangiocarcinoma 5 and hepatocellular carcinoma 6.
Pathology
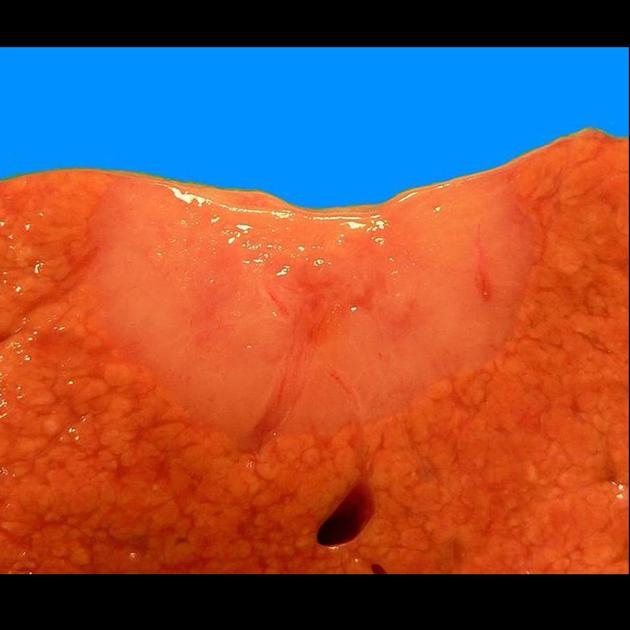
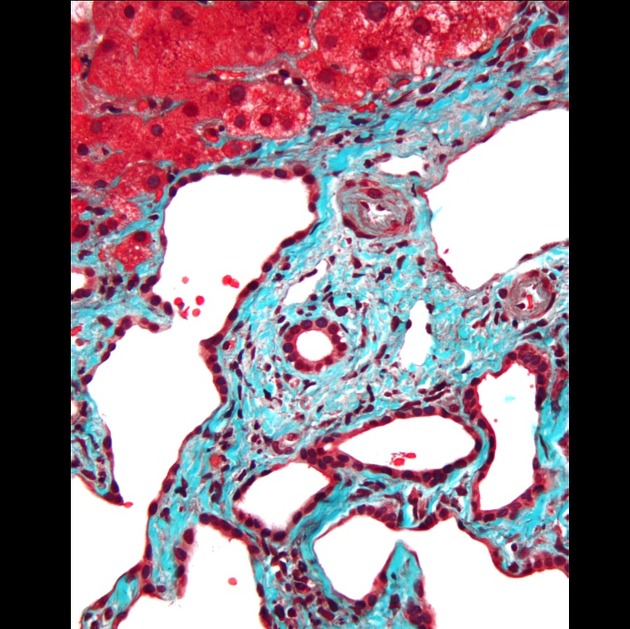
Biliary hamartomas are composed of small disorganized clusters of dilated cystic bile ducts lined by a single layer of cuboidal cells and surrounded by an abundant fibrocollagenous stroma 1,7,8. Although they may communicate with the biliary tree, they generally do not. They are thought to arise from embryonic bile duct remnants that have failed to involute.
Radiographic features
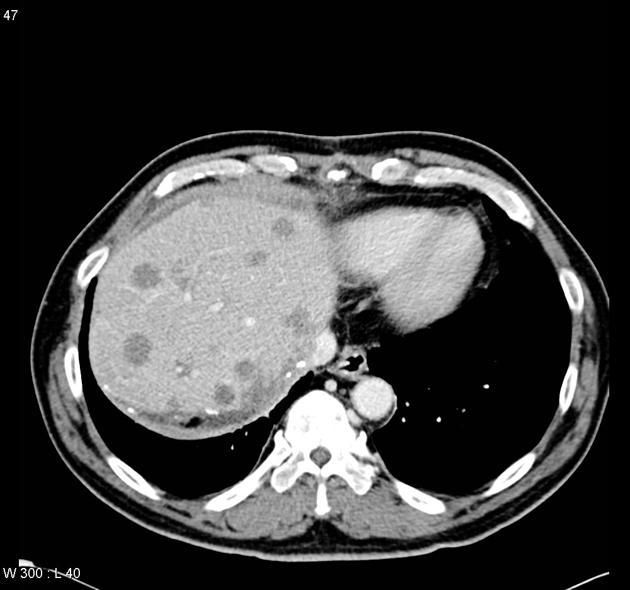
They appear as multiple small round or irregular lesions throughout the liver, with some predilection for subcapsular regions 1. They are usually 5-30 mm in size when detected by imaging (however most lesions are <5 mm when detected by pathologists). Radiographic findings can be non-specific and may be hard to differentiate from metastases and microabscesses.
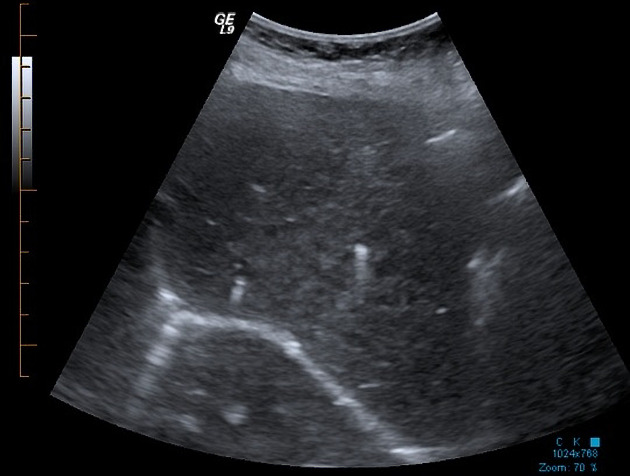
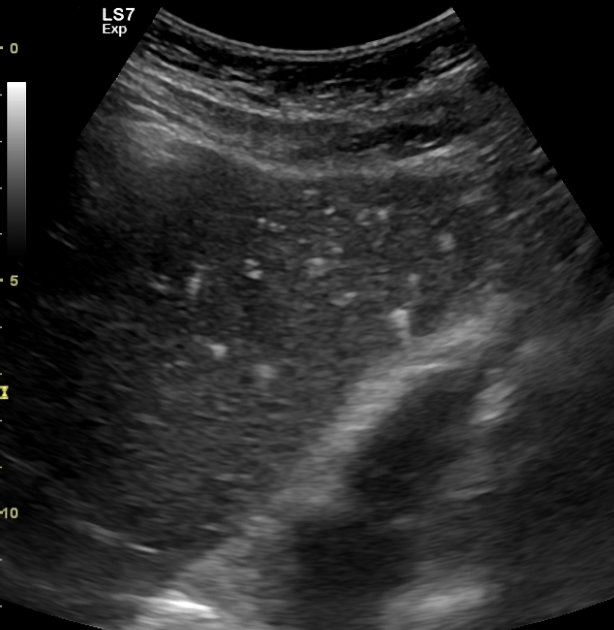
Ultrasound
Small hamartomas are usually echogenic if discretely seen. Often tiny individual hamartomas cannot be resolved and are instead interpreted as diffuse heterogeneous liver echotexture. Larger hamartomas (>10 mm) may appear hypoechoic or anechoic and comet-tail artifact may be seen 9. The appearances may mimic metastases (see ultrasound appearances of liver metastases).
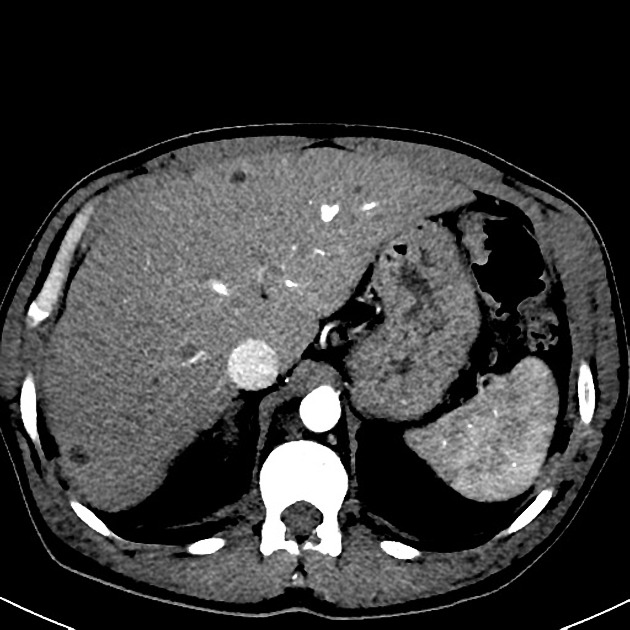
CT
Biliary hamartomas are hypoattenuating and often show no enhancement 7. Occasionally an enhancing nodule or rim may be identified in a small number of lesions.
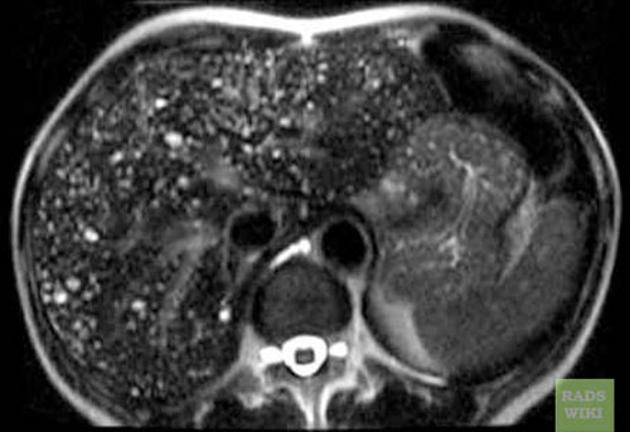
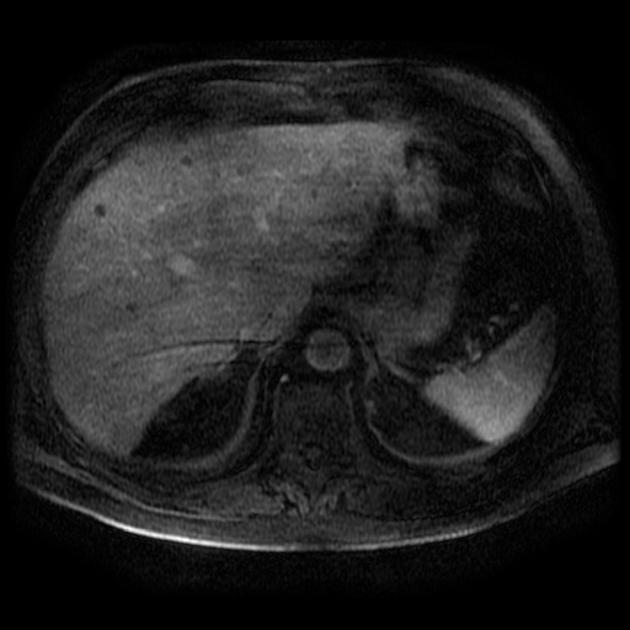
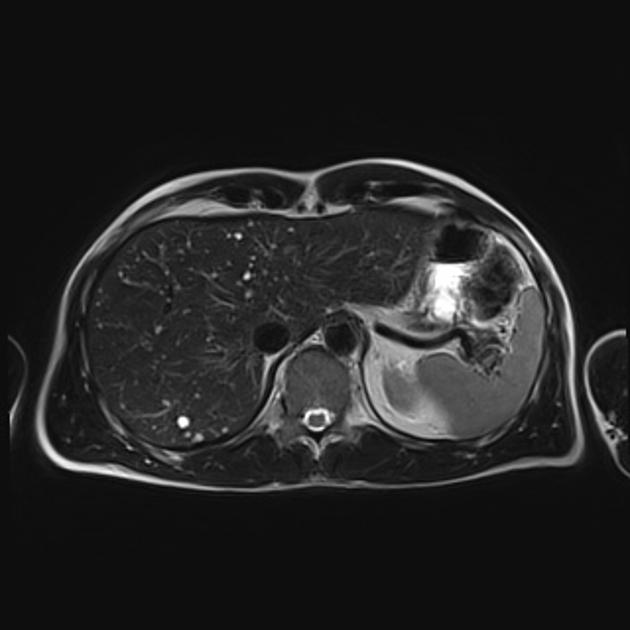
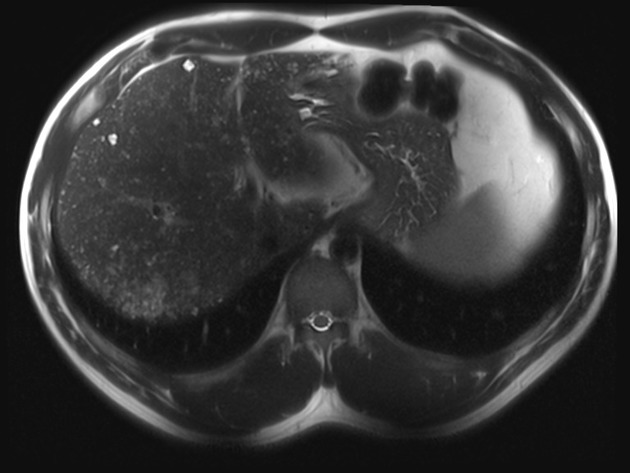
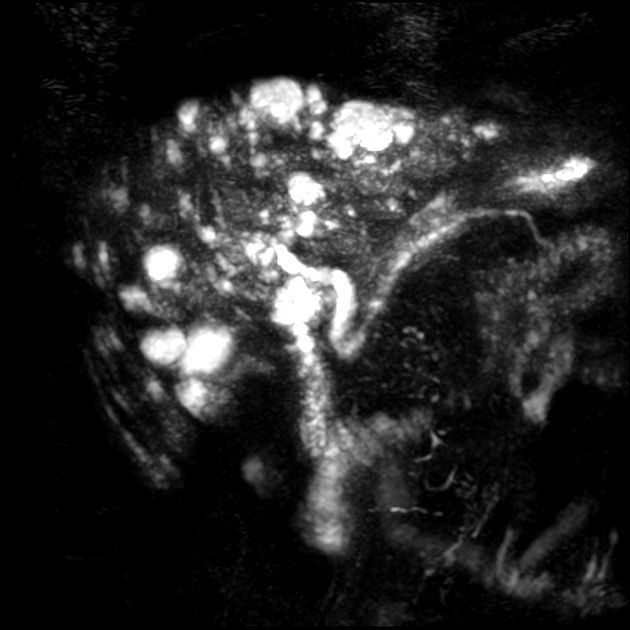
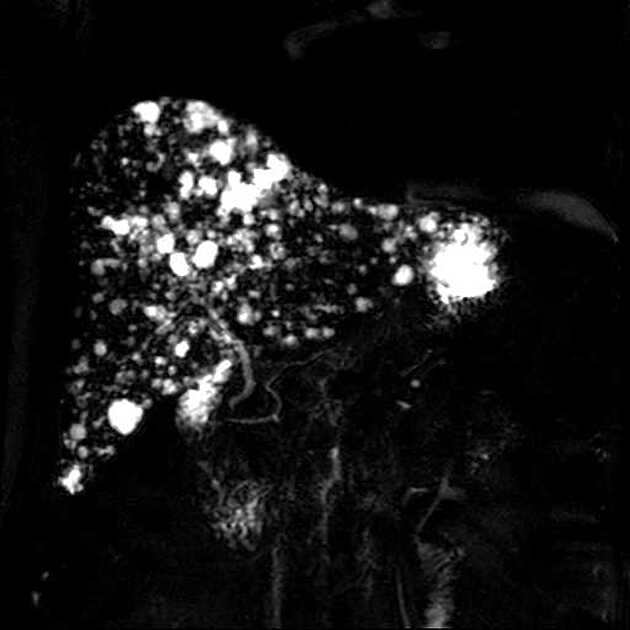
MRI
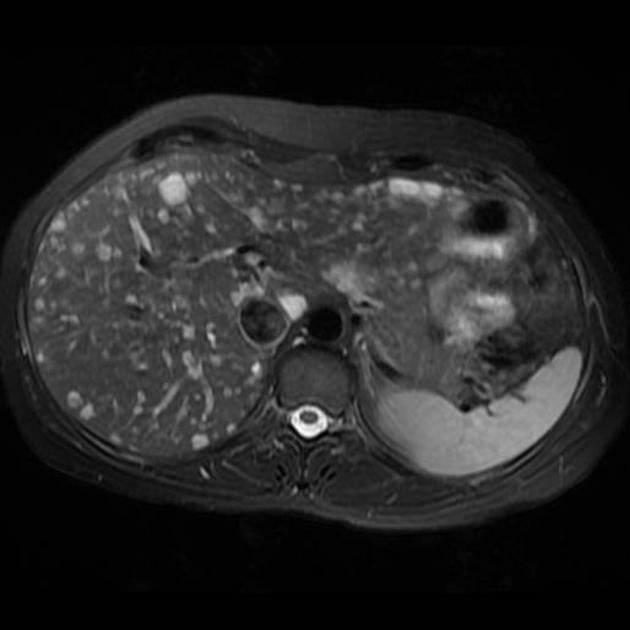
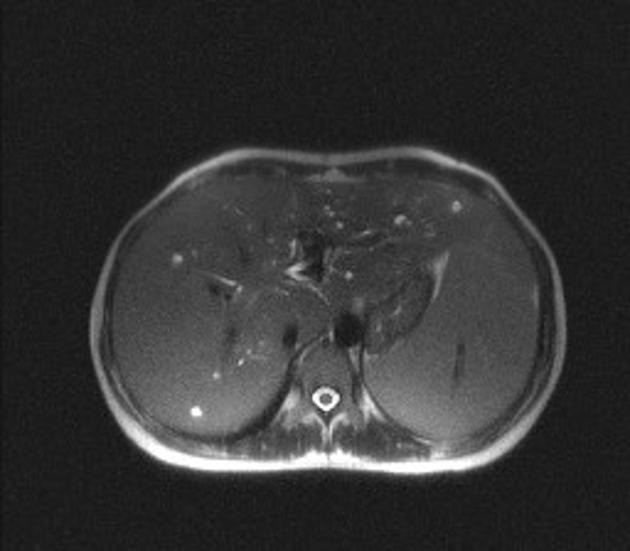
Most biliary hamartomas are:
T1: hypointense compared to liver parenchyma
-
T2
hyperintense
depending on TE, may approach CSF-signal intensity
-
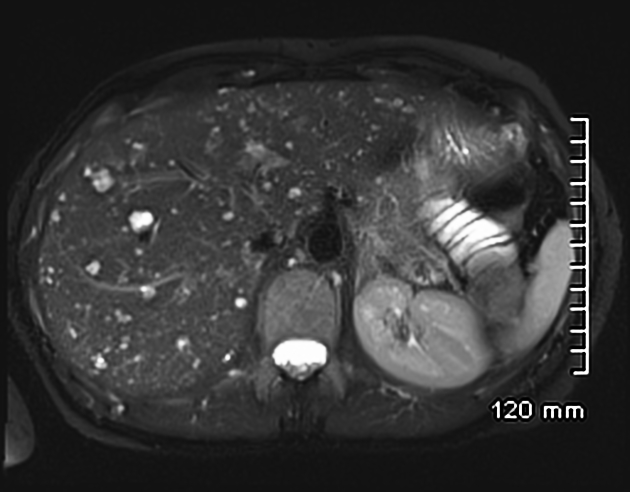
T1 C+ (Gd)
usually no enhancement
there may be thin peripheral rim enhancement that may represent compressed normal liver parenchyma 14,15
In ~90% of cases, an occasional hamartoma can be found containing a mural nodule (fibrocollagenous stroma) or rim (see above) that is T1 isointense and T2 intermediate, of which ~90% will enhance. Hamartomas show no diffusion restriction on DWI sequences 2,9,11.
Angiography (DSA)
Only a limited number of the many lesions that are actually present can be seen as grape-like clusters of abnormal vascularity with contrast persisting into the venous phase 10.
Nuclear medicine
Cholescintigraphy shows delayed uptake and delayed emptying of tracer within larger biliary hamartomas 12.
Treatment and prognosis
Aside from the possible risk of malignant transformation of cholangiocarcinoma or hepatocellular carcinoma, multiple biliary hamartomas are a benign asymptomatic condition with no long-term consequences, and no treatment is required.
History and etymology
Hans von Meyenburg (1887-1971) was a German-born Swiss pathologist who first described the pathology of biliary hamartomas in an article published in 1918 13,16.
Differential diagnosis
General imaging differential considerations include:
multiple liver metastases: more variable size and prominent enhancement
multiple liver microabscesses: clinical context is important, may have diffusion restriction on MRI
multiple small hepatic cysts
Caroli disease: demonstrates enhancing central dot sign of portal radicles









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.