Intracerebral haemorrhage (ICH), also known as intraparenchymal cerebral haemorrhage and often synonymously describing haemorrhagic stroke, is a subset of an intracranial haemorrhage as well as of stroke, defined by the acute accumulation of blood within the brain parenchyma.
This article concerns non-traumatic intracerebral haemorrhages; traumatic haemorrhagic cerebral contusions are discussed separately.
On this page:
Terminology
By convention, intracerebral haemorrhage refers to macroscopically visible, recent haemorrhages. In contrast, cerebral microhaemorrhages are discussed separately.
Clinical presentation
An intracerebral haemorrhage presents similarly to an ischaemic stroke and there are no reliable clinical differentiators between the two. There is typically a rapid onset of focal neurological deficit, which varies depending on the specific area of the brain that is involved. Compared to ischaemic stroke, there is more likely to be a decreased conscious state 11. Other common clinical features include 13:
headache
nausea and vomiting
seizure
Pathology
Intracerebral haemorrhages arise from rupture of a small blood vessel within the brain parenchyma or, less commonly, of a blood vessel adjacent to the parenchyma (e.g. jet haematoma).
Aetiology
Non-traumatic intracerebral haemorrhages were historically aetiologically divided according to whether or not they have an underlying structural lesion or bleeding diathesis.
-
spontaneous intracerebral haemorrhage presumed due to small vessel disease (formerly primary intracerebral haemorrhage 10)
-
secondary intracerebral haemorrhage: haemorrhage complicating some underlying structural lesion or bleeding diathesis
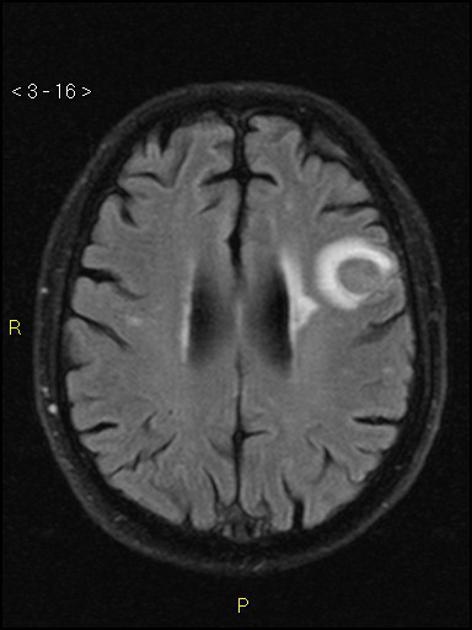
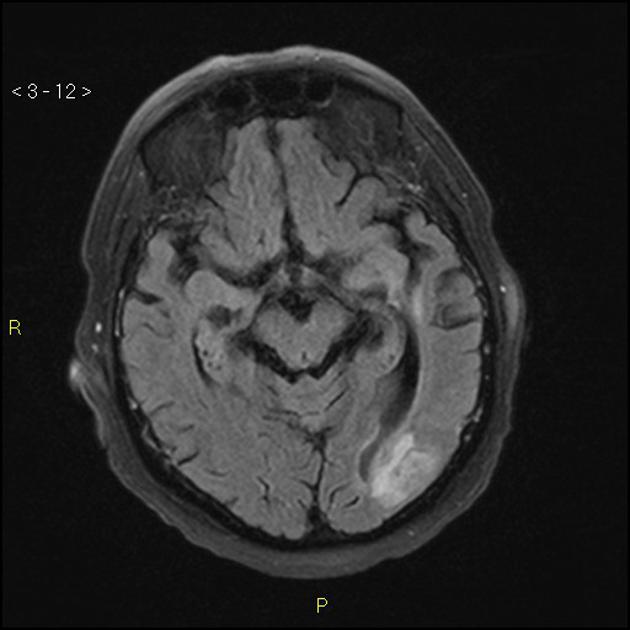
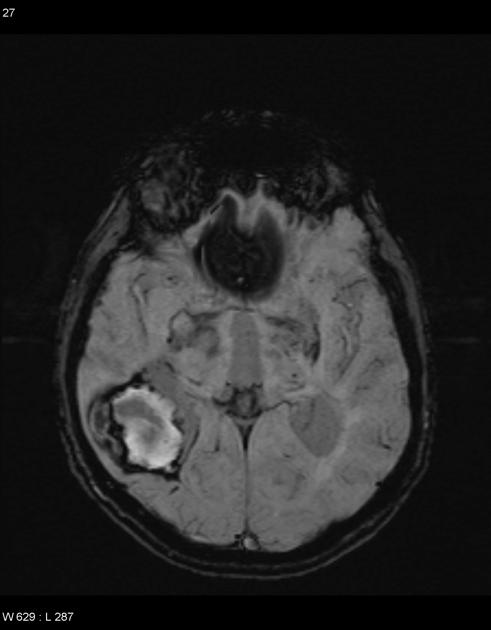
vascular malformation (e.g., brain arteriovenous malformation, cerebral cavernous malformation)
tumour (e.g., metastases, glioblastoma)
bleeding diathesis (e.g., anticoagulation therapy)
Aetiologies more commonly seen in the paediatric or young adult demographic are discussed separately: see stroke in children and young adults.
Location
Non-traumatic intracerebral haemorrhages are classified by location, which vary by aetiologic association 9.
lobar intracerebral haemorrhage: in any lobe(s) of the cerebral hemispheres in a cortical and/or subcortical location (excluding deep hemispheric and infratentorial regions)
-
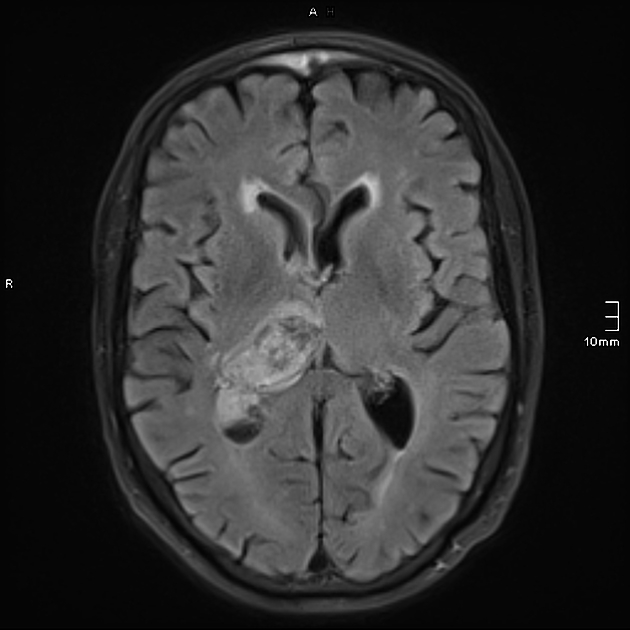
non-lobar intracerebral haemorrhage: in deep hemispheric or infratentorial location
deep hemispheric (basal ganglia, thalamus, internal capsule)
Radiographic features
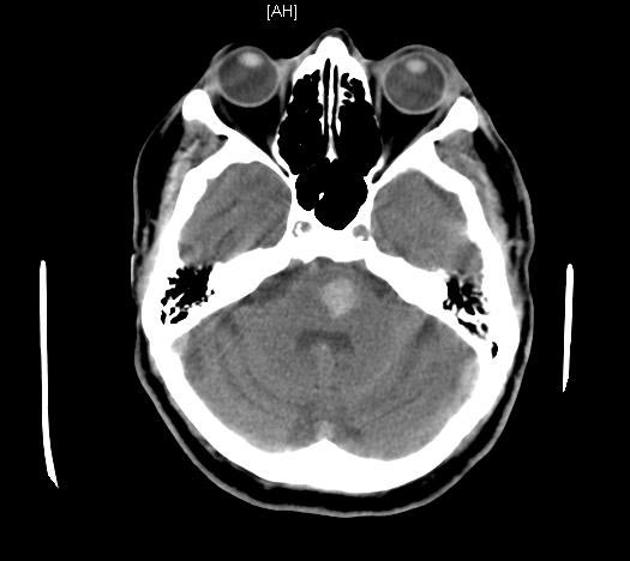
CT
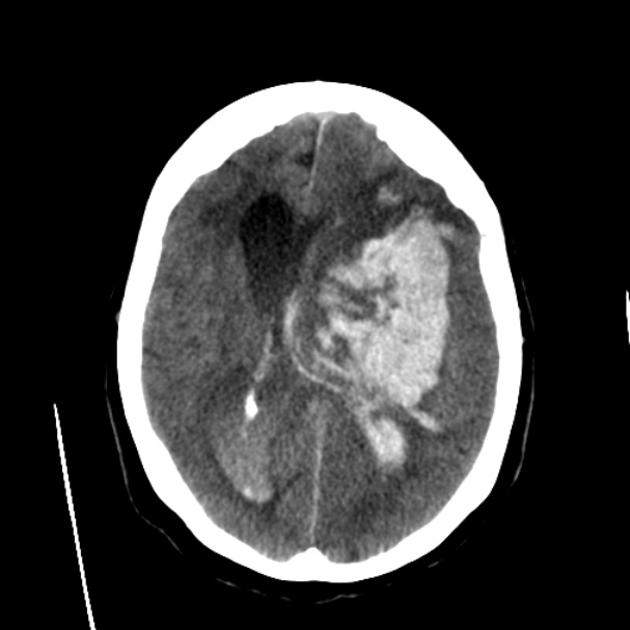
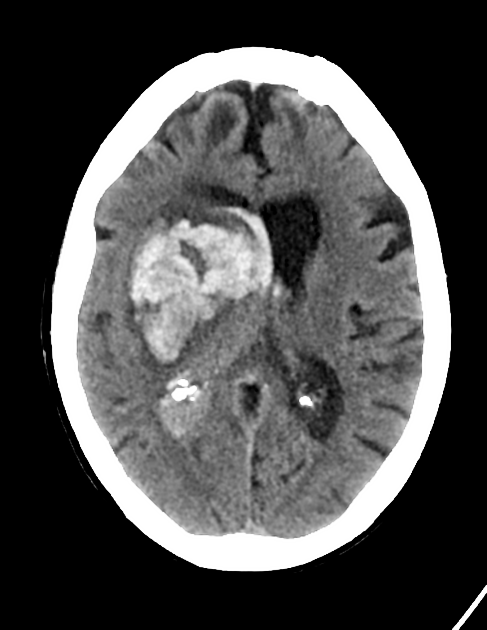
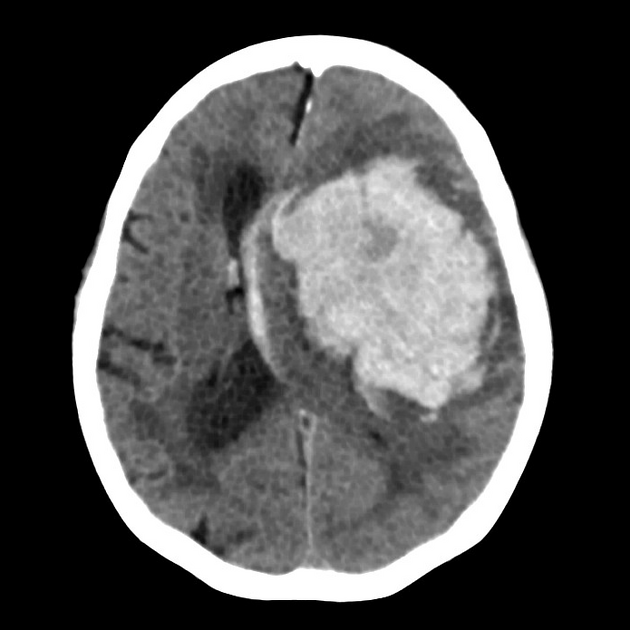
CT is usually the modality first obtained and demonstrates a hyperdense collection of blood, often with surrounding hypodense oedema. A number of complications may be present, such as extension of the haemorrhage into other intracranial compartments, hydrocephalus, herniation, etc.
A number of CT features can predict the likelihood of haemorrhage expansion and are therefore useful in decision-making and prognosis.
-
non-contrast CT
-
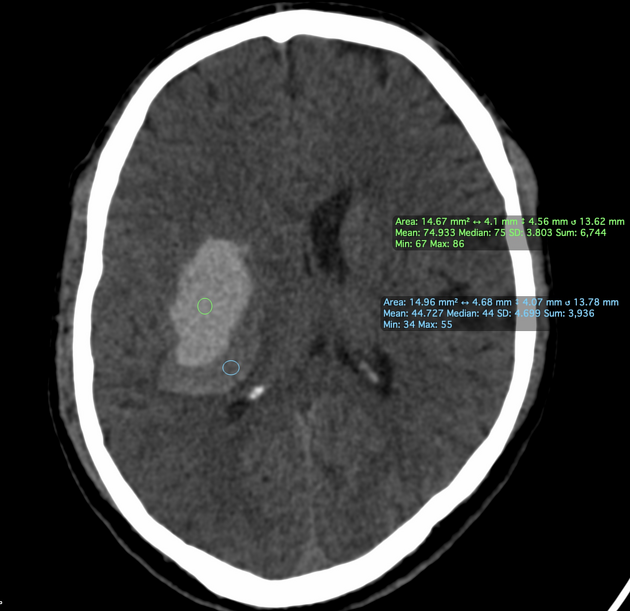
haemorrhage size
the volume of an intracerebral haemorrhage can be measured using ABC/2 formula or 3D volumetric software
haemorrhage size is considered to be the most reliable independent predictor of ICH expansion
haematoma expansion is measured as an increased growth >12.5 mL or volume >33% from the initial CT scan
haematomas with a volume of more than 30 mL are more prone to expansion
-
haemorrhage shape
intracerebral haemorrhage irregularity is thought to be due to multiple leaking vessels feeding the haematoma
haemorrhages with irregular shapes are more prone to expansion
-
haemorrhage density
the presence of hypodense or isodense regions within the hyperdense intracerebral haemorrhage represents active bleeding and is called swirl sign
when the swirl sign is encapsulated it is termed black hole sign
the presence of a relatively hypodense area adjacent to a hyperdense area is termed the blend sign
heterogeneous haemorrhage with hypodense foci is more prone to expansion
-
intraventricular haemorrhagic extension
intraventricular haemorrhagic extension occurs due to decompression of the haemorrhage into the low resistance ventricular system, thus; haematomas located in the thalamus, caudate nucleus or pons are more prone to intraventricular extension than lobar haematomas
a study has shown that lenticular and lobar haematomas with accompanying intraventricular extension displayed a higher proportion of haematoma expansion 5
-
-
contrast-enhanced CT
active contrast extravasation within haematoma predicts future haemorrhage expansion, this can be observed on CT angiography (CTA) as spot sign and pooling of contrast within the haematoma
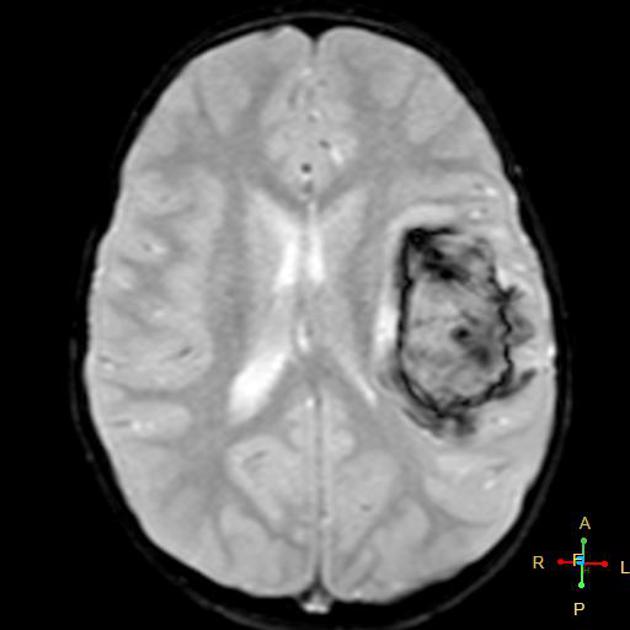
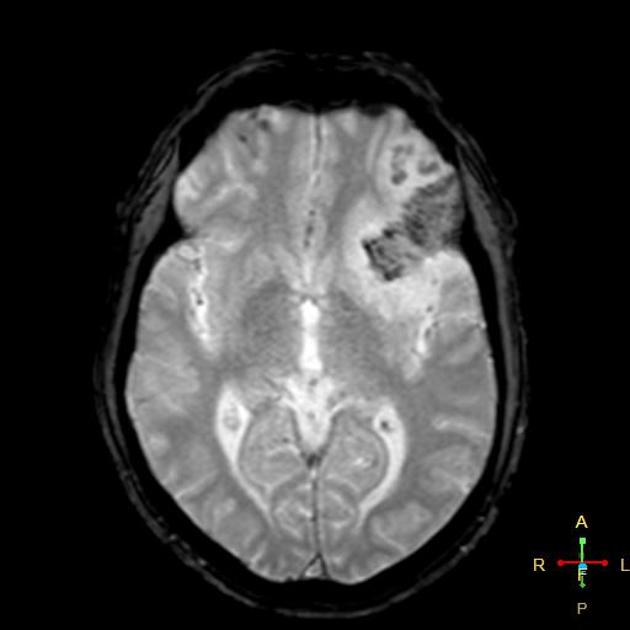
MRI
Findings depend on the size and age of the bleed (see ageing blood on MRI). MRI may also reveal clues to the aetiology, such as those of cerebral small vessel diseases (e.g. hypertensive microangiopathy, cerebral amyloid angiopathy).
Treatment and prognosis
Management is time-critical 14,15, with the principles of management including 12:
control of blood pressure, aiming for a systolic blood pressure of ~140 mmHg
-
reversal of any anticoagulation or coagulopathy
there is a paucity of evidence to support the effectiveness of routine use of haemostatic agents
-
management of raised intracranial pressure
e.g. external ventricular drain in the acute setting (especially if there is concurrent intraventricular haemorrhage), decompressive hemicraniectomy (weak evidence to support this in deep intracerebral haemorrhage 17)
-
neurosurgical haematoma evacuation can be considered on a case-by-case basis
evidence to support haematoma evacuation with or without extraventricular drain in cerebellar intracerebral haemorrhage 12, minimally invasive evacuation techniques in lobar intracerebral haemorrhage 16
-
management of seizures with antiseizure medications
there is a paucity of evidence to support the effectiveness of antiseizure medication prophylaxis for patients without seizures
Additionally, supportive care should be provided, including caring for patients in dedicated inpatient stroke units and attempting to prevent the numerous complications which are encountered by patients with neurological impairment from stroke.
Practical points
With any intracerebral haemorrhage the following points should be included in a report as they have prognostic implications 3:
location
-
size/volume
the ABC/2 formula is widely used, but there may be more accurate formulas (e.g. 2.5ABC/6, SH/2) and analyses available, some of which, however, may require the addition of specific software to the standard PACS tools
shape (irregular vs regular)
density (homogeneous vs heterogeneous)
presence/absence of substantial surrounding oedema that may indicate an underlying tumour
presence/absence of intraventricular haemorrhage
presence/absence of hydrocephalus
when CT angiography is performed, the presence/absence of the CTA spot sign or a vascular malformation










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.