Regenerative liver nodules are a form of non-neoplastic nodules that arise in a cirrhotic liver.
On this page:
Terminology
This may be slightly different from the term nodular regenerative hyperplasia, which are described histopathologically as regenerative nodules with little or no hepatic fibrosis and largely healthy hepatic architecture 1. When there is an accumulation of iron in the nodules, they are called siderotic nodules.
Pathology
Regenerative liver nodules form in the setting of necrosis or altered local vascularity and can be of three types 5:
micronodules <3 mm
macronodules >3 mm
giant regenerative nodules >5 cm (rare)
Radiographic features
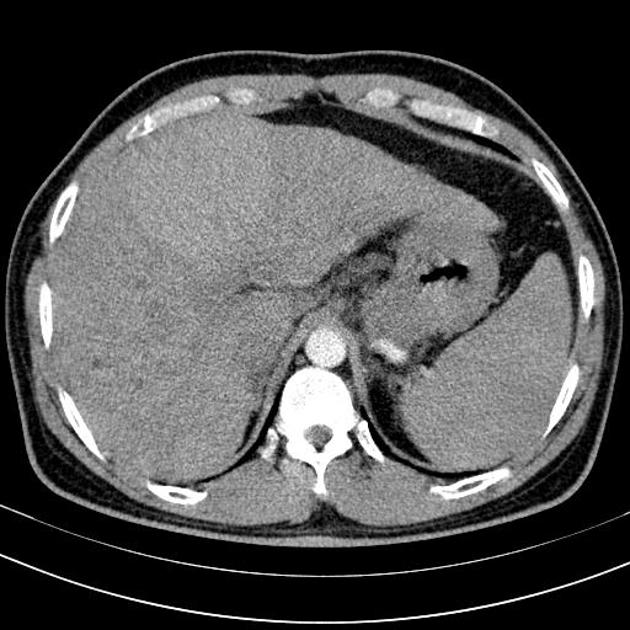
Regenerative nodules appear as round, well-defined nodules (usually in the thousands) present throughout the liver with surrounding fibrosis 5.
On post-contrast CT and MRI, regenerative nodules enhance similar to the normal liver parenchyma in both portal venous and hepatocellular/delayed phases, and thus may not be distinguishable in a cirrhotic liver. Arterial phase enhancement is generally absent or minimal, and will increase with the degree of dysplastic transformation and neo-vascularization.
CT
Regenerative nodules are rarely visible on non-contrast CT unless they are siderotic (i.e. containing iron). Siderotic regenerative nodules are hyperdense to liver on precontrast imaging and become isodense to liver on post contrast phases.
CT arterial portography
Contrast injection into the superior mesenteric artery (after arterial vascular access). Regenerative nodules are generally visualized as enhancing nodules surrounded by lower attenuation thin septa.
CT hepatic arteriography
Contrast injection into the common hepatic artery (after arterial vascular access). Regenerative nodules are generally visualized as non-enhancing nodules surrounded by enhancing fibrous septa.
CT hepatic arteriography is considered more sensitive than the former in depicting regenerative nodules 4.
MRI
Regenerative liver nodules are common in a cirrhotic liver 5:
T1: variable
T1 IP/OP: loss of signal on out-of-phase if fat-containing
T2: hypointense
T2*: hypointense
T1C+: usually do not enhance or enhance less than the liver parenchyma
Treatment and prognosis
Regenerative nodules may progress to dysplastic nodules or hepatocellular carcinoma 5.
Practical points
fat-containing regenerative nodules are usually multiple; a solitary fat-containing nodule is concerning for dysplasia/malignancy 5




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.