The stomach is a muscular organ that lies between the esophagus and duodenum in the upper abdomen. It lies on the left side of the abdominal cavity caudal to the diaphragm at the level of T10.
On this page:
Gross anatomy
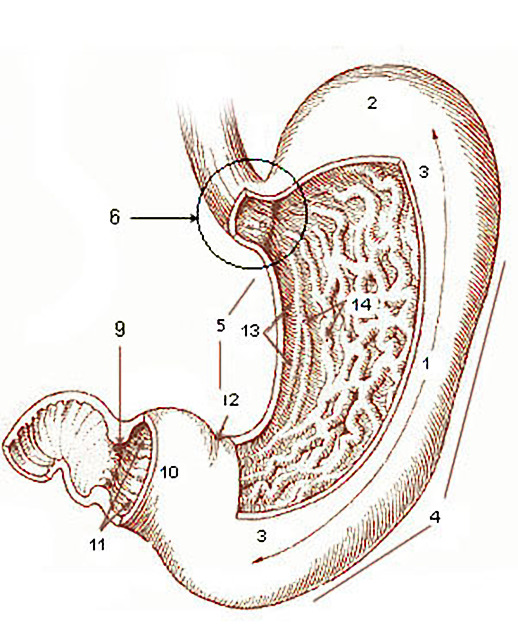
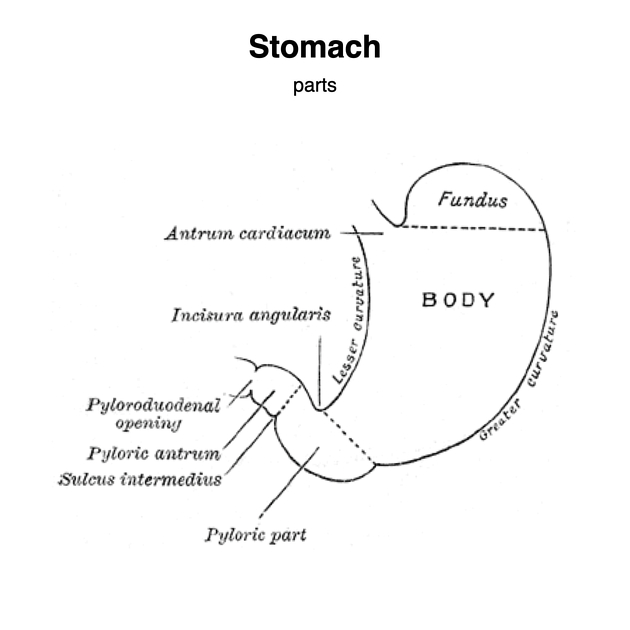
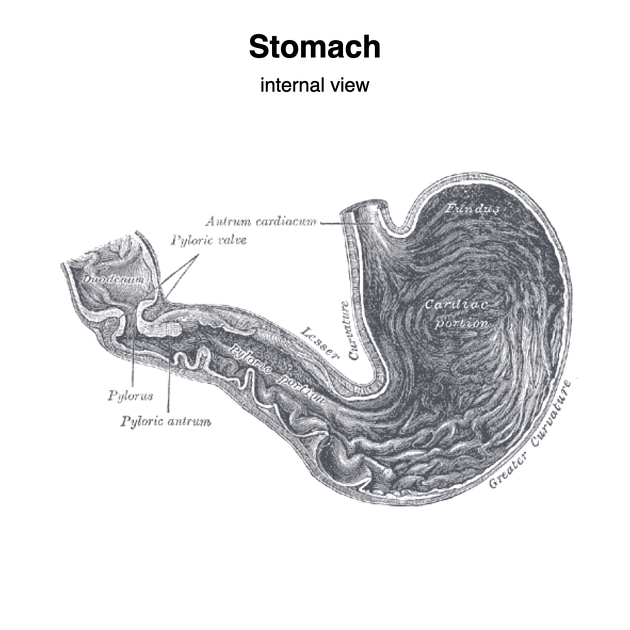
The stomach ("normal" empty volume 45 mL) is divided into distinct regions:
cardia: the area that receives the esophagus (gastro-esophageal junction)
fundus: formed by the upper curvature; portion of stomach above GEJ level 17
body (corpus): the main central region of the organ; central two-thirds portion from the cardia to the incisura angularis 17
pylorus (antrum): the lower section of the stomach that facilitates emptying into the small intestine, located on the right of the midline at the level of L1.
The lesser curvature forms the shorter concave border and the greater curvature forms the longer convex border of the stomach. The lesser omentum attaches the lesser curvature to the liver, while the greater omentum attaches to the greater curvature of the stomach 17.
There are two smooth muscle sphincters, esophageal and pyloric, that dictate entry into and exit from the stomach. These are under the control of several mechanisms including stimulant (parasympathetic) and inhibitory (orthosympathetic) control from the anterior gastric, posterior, superior and inferior celiac plexus and myenteric nerve plexuses.
The inner mucosal surface has many rugal folds that act to increase the surface area of the stomach lining and increase its efficiency.
Specific sites
incisura angularis: small anatomical notch on the stomach located on the lesser curvature of the stomach near the pyloric end, which marks the junction between the body and the antrum 17
fornix gastricus: refers to the arch-shaped superior margin of the fundus of the stomach
Relations
anteriorly: left lobe of liver, anterior abdominal wall, left hemidiaphragm
posteriorly: anterior wall of lesser sac, stomach bed
medially: abdominal aorta, celiac trunk, celiac lymph nodes
Arterial supply
lesser curvature: right gastric artery (inferiorly) and left gastric artery (superiorly)
cardia: left gastric artery
greater curvature: right gastroepiploic artery (inferiorly) and left gastroepiploic artery and short gastric arteries (superiorly)
fundus of the stomach: short gastric arteries
Venous drainage
left and right gastric veins drain to portal vein
short gastric vein and left gastroepiploic vein drain to splenic vein
right gastroepiploic vein drains to superior mesenteric vein 3
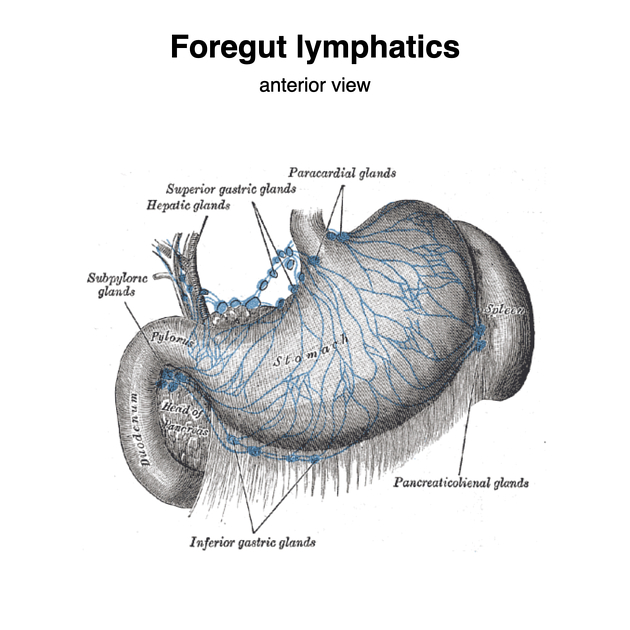
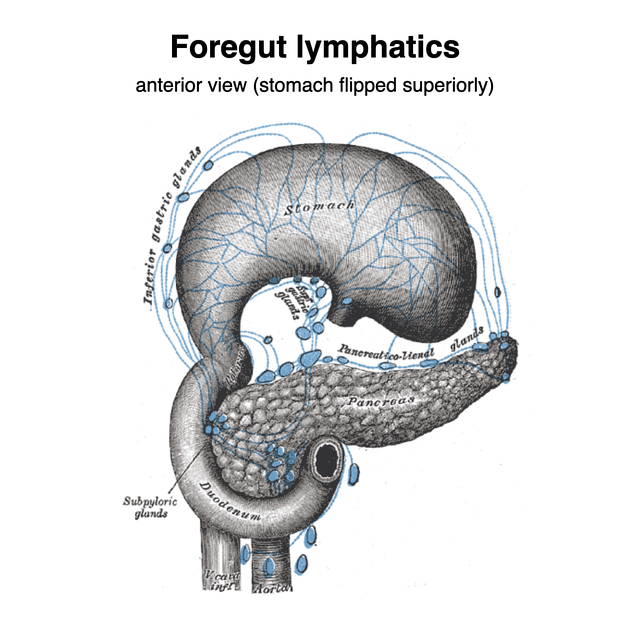
Lymphatic drainage
Stomach has its own lymph nodes stations. Routes of flow of lymph from perigastric nodes to para-aortic lymph nodes include 4-6:
directly to left paracardial lymph nodes
along lymph nodes accompanying the splenic artery
along lymph nodes accompanying the celiac artery
along lymph nodes accompanying the superior mesenteric artery
along lymph nodes on the posterior surface of the pancreatic head and nodes accompanying the common hepatic artery
It is suggested that the most likely route for para-aortic lymph node metastases is from the left gastric artery nodes accompanying the celiac artery 4.
Innervation
-
sympathetic innervation is from the T5 to T12 segments of the sympathetic chain via the greater and lesser splanchnic nerves which synapse in the celiac plexus.
sympathetic supply causes vasoconstriction, inhibition of gastric motility and pyloric constriction
afferents run with the sympathetic fibers (visceral pain sensation)
-
parasympathetic innervation is from the vagus nerves
the anterior vagal trunk supplies the anterior surface of the upper body and fundus, antrum, parts of the lesser curvature and the pylorus
the posterior vagal trunk supplies the cardiac orifice and posterior surface of the body and antrum
parasympathetic supply is secretomotor to the gastric mucosa, promotes gastric motility and relaxes the pyloric sphincter during gastric emptying
Histology
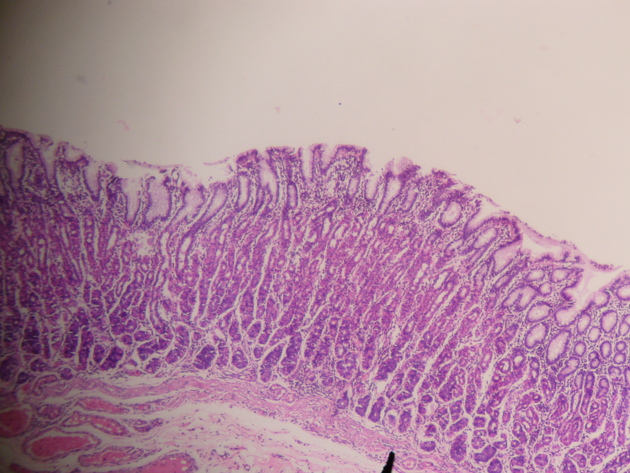
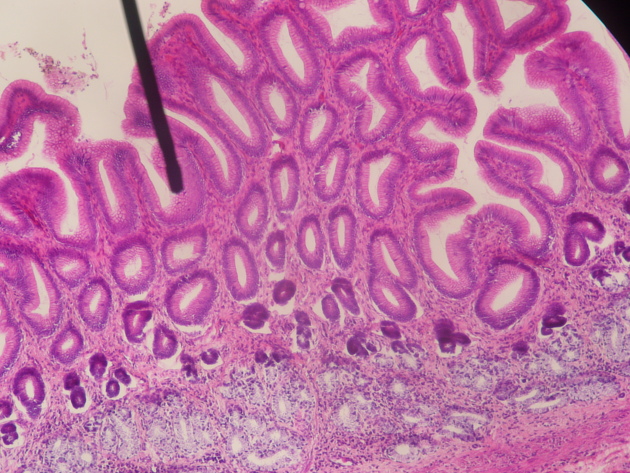
Akin to other areas of the gastrointestinal (GI) tract, the stomach walls are composed of the following layers:
mucosa: internal layer of epithelium, the lamina propria (loose connective tissue and gastric glandular tissue) and the muscularis mucosae
submucosa: a fibrous layer of connective tissue under the mucosa
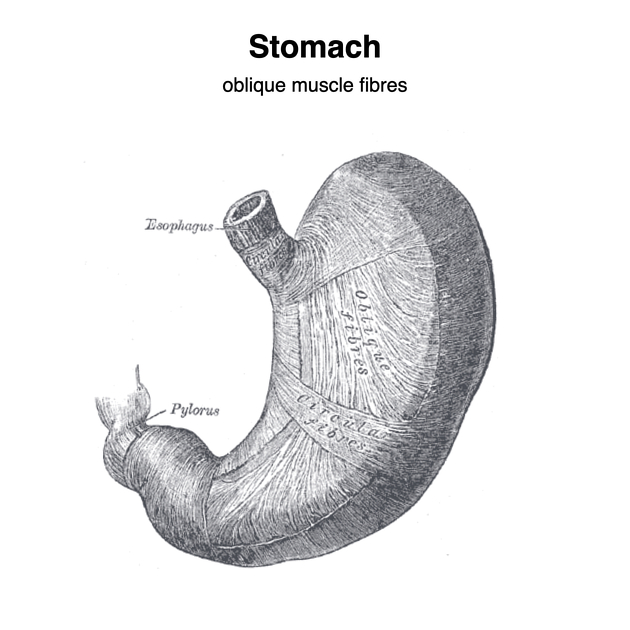
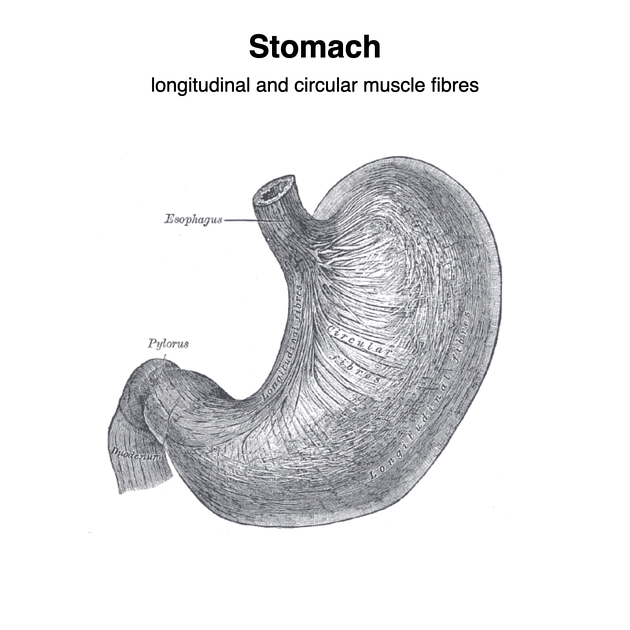
muscularis externa: this is the muscular layer of the stomach wall and is comprised of three layers (inner oblique, middle circular and outer longitudinal) unlike other GI organs which only have two layers
serosa: the outermost layer of the stomach wall consisting of connective tissue which is continuous with the peritoneum
Cell types
The stomach wall contains several different types of glandular tissue. The cardia, fundus and pylorus all have different types of glands and are composed of a variety of different cells:
mucous cells: secrete a mucus gel layer and are found throughout the stomach
parietal (oxyntic) cells: secrete gastric acid and intrinsic factor throughout the stomach
chief (zymogenic) cells: secrete pepsinogen and rennin in the fundus and body 17
enteroendocrine (APUD cells): secrete a variety of products and are found throughout the stomach
Physiology
Control of the stomach relates to the autonomic nervous system and various digestive system hormones:
gastrin: causes an increase in the secretion of hydrochloric acid (HCl), pepsinogen and intrinsic factor from parietal cells in the stomach; it also causes increased motility in the stomach; released by G-cells in the stomach to distension of the antrum, and digestive products; inhibited by a pH normally <4 (acidic), as well as the hormone somatostatin
cholecystokinin (CCK): greatest effect on the gallbladder, but it also decreases gastric emptying and increases release of pancreatic juice which is alkaline and neutralizes the chyme
secretin: has most effects on the pancreas, but will also diminish acid secretion in the stomach
gastric inhibitory peptide (GIP): decreases both gastric acid and motility
enteroglucagon: decreases both gastric acid and motility
glycogen: produced in the brain and stomach, affects the liver and level of glucose in the stomach
Radiographic features
Plain radiograph
The stomach is not usually well visualized on the plain film although a gastric bubble (gas outlining the fundus of the stomach) is often visible on an erect chest or abdominal x-ray.
Gastric rugae is readily identified on supine abdominal radiograph 20,21.
Ultrasound
Analogous to the abovementioned histological architecture, the gastric walls will consist of five concentric layers of alternating echogenicity when viewed with an appropriately high frequency transducer, characteristic of the sonographic gut signature 16.
Sonographic localization of the stomach is typically performed with epigastric transducer placement with the patient in a supine or right lateral decubitus position. The gastric antrum is commonly visualized just to the right of anatomic midline using the following sonographic landmarks; 11
-
lies cephalad and anterior to the gastric antrum 16
-
lies posteriorly to the gastric antrum
-
identified lying anteriorly to the abdominal aorta and superior mesenteric artery
parallels the course of the splenic vein, which demarcates its posterior extent 12
-
inferior to the gastric antrum
Visualization of the gastric body is often possible by sweeping leftward of the gastric antrum. Visualization of the gastric fundus may require using the spleen as a sonographic window, using a left intercostal probe position. The sonographic appearance of the stomach, most notably the gastric antrum, may differ based on the patient's prandial status as follows;
-
fasting patient
-
gastric antrum may appear as a flattened ovoid with absent to minimally appreciable luminal contents 11
targetoid or "bulls eye" appearance 12
may also appear round, with homogenous anechoic fluid filling the lumen
-
-
post-prandial patient
viscous fluid ingestion results in luminal contents appearing uniformly hyperechoic
-
recent solid food ingestion results in a heterogeneous appearance of luminal contents, with posterior acoustic shadowing
may be indicative of higher aspiration risk for patients under general anesthesia 10
CT
When well distended, the normal gastric wall will have a thickness of 5-7 mm in the antrum and 2-3 mm in the body 17.
Related pathology
-
neoplastic
-
inflammatory
-
infections
-
congenital gastric condition
-
other






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.