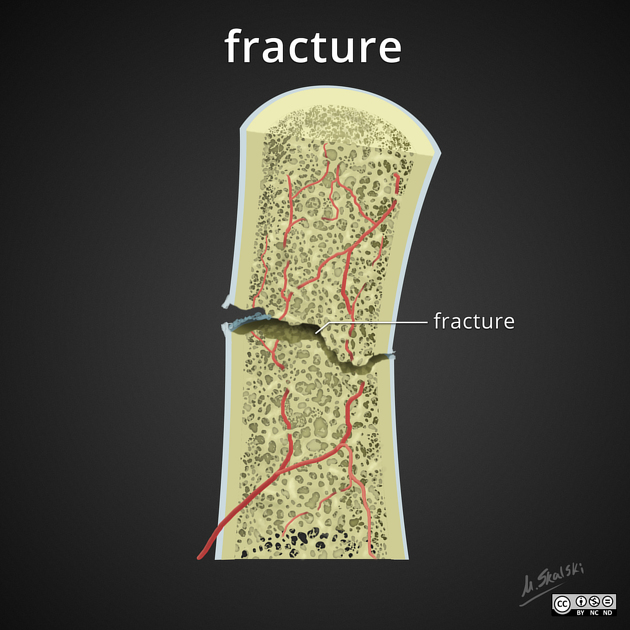
A fracture is a discontinuity in a bone (or cartilage) resulting from mechanical forces which exceed the bone's ability to withstand them.
On this page:
Terminology
A fracture is often written as # in medical shorthand, i.e. the hash symbol, although it is still pronounced as fracture, e.g. "neck of femur fracture", may be written as "#NOF".
Most commonly fractures occur in the setting of a normal bone with acute overwhelming force, usually in the setting of trauma. Fractures can also occur, however, in a variety of other settings.
Firstly, the entire skeleton may be weak due to metabolic (e.g. osteoporosis) or less frequently genetic abnormalities (e.g. osteogenesis imperfecta) and thus prone to fractures from forces that would be insufficient to cause fractures in normal bones. These are known as insufficiency fractures.
Secondly, the protracted chronic application of abnormal stresses (e.g. running) can result in the accumulation of microfractures faster than the body can heal, eventually resulting in macroscopic failure. These are termed fatigue fractures.
Together, insufficiency and fatigue fractures are often grouped together as stress fractures.
Thirdly, the bone may have a lesion that focally weakens it (e.g. metastasis, bone cyst, etc). These are known as pathological fractures.
Rarely the term 'fracture' is also used for non-osseous/chondral structures (e.g. penile fracture) although if unqualified it is assumed one is referring to a bony fracture.
Although many eponymous fractures exist and the relevant particulars of a fracture will depend on its specific location, generally fractures are described in a consistent manner:
Location
which bone is fractured
-
which part of the bone is affected
general: epiphysis, physis, metaphysis, diaphysis
specific features: e.g. tubercle, epicondyle, etc...
Type
Fractures usually fall within a set number of patterns.
-
complete fracture: extends all the way across the bone (most common)
transverse fracture: perpendicular to the axis of the bone
oblique fracture: oriented obliquely across the bone
spiral fracture: helical fracture path usually in the diaphysis of long bones
comminuted fracture: more than two parts
-
incomplete fracture: does not cross the bone completely (usually encountered in children)
buckle fracture: the cortex is buckled, often in the distal radius
greenstick fracture: the cortex is broken, but only on one side
Displacement
The relationship between fracture fragments can be described using the following terms.
-
fracture translation (a.k.a. translocation or displacement)
direction: usually of the distal part relative to the proximal part
amount: linear measurement or % width
-
direction: usually of the distal part relative to the proximal part
amount: in degrees
-
direction: terminology will depend on the location
amount: in degrees
-
direction: usually of the distal part relative to the proximal part
amount: linear measurement
distraction versus shortening (impaction or depression)
Complications
Many of the aforementioned fracture types can also go on to have additional complicating features, not to mention many associated soft tissue injuries beyond the scope of this article.
compound fracture: extending through the skin
-
joint involvement
intracapsular
articular
dislocation
Pathology
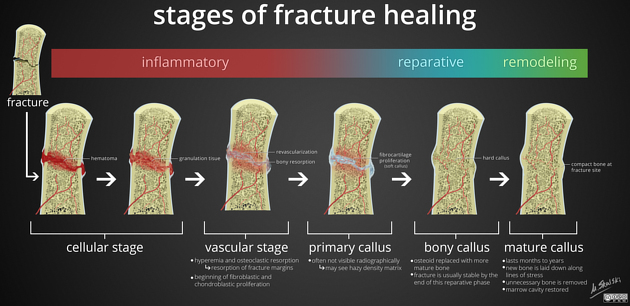
The pathophysiological sequence of events that occur following a fracture and eventually (hopefully) lead to complete fracture healing are fairly stereotyped and can be divided into three main phases:
inflammatory
reparative
remodeling
Inflammatory phase
Immediately at the time of fracture, the space between fracture ends is filled with blood forming a hematoma. Not only does this hematoma stop additional bleeding it also provides structural and biochemical support for the influx of inflammatory cells, fibroblasts, chondroblasts and the ingrowth of capillaries 1.
At the end of this process, which usually takes approximately a week, a primary callus (also known as soft-tissue callus, or procallus) is present which is non-mineralized and not readily visible on radiography 1.
Reparative phase
Over the ensuing few weeks this primary callus is transformed into a bony callus by the activation of osteoprogenitor cells. These cells lay down woven bone which stabilizes the fracture site 1.
Remodeling phase
The remodeling phase lasts many months, and even years, and represents the gradual formation of compact cortical bone with greater biomechanical properties and allows for the reduction of the width of the callus. In some instances, remodeling can result in almost perfect healing. In most instances, however, particularly if the alignment is not perfect, a residual deformity will remain.
Diagnosis
The diagnosis of a fracture is mainly based on typical radiographic criteria proving the bony discontinuity.
Radiographic features
Fractures are generally imaged using plain radiographs, however, there are a number of situations in which CT, MRI, bone scans or ultrasound are useful:
when 3D anatomy is complex (e.g. joints, wrists, feet, the base of skull, spine)
when plain films are insensitive to non-displaced fractures (e.g. base of skull, spine, sacrum, or proximal neck of femur)
when a pathological fracture is suspected
Both plain radiographs and CT rely on the identification of discontinuity of bone at the fracture site. In contrast, MRI relies primarily on visualizing soft tissue and bone marrow changes, whereas nuclear medicine (e.g. bone scans) visualizes bone metabolic changes.
Historically ultrasound was not considered to be the first-line modality to diagnose fractures and has been more commonly used for children. However, there is now renewed interest in its use as a POCUS tool in the emergency setting 2.
Plain radiograph
The radiographic positions should be optimal for the evaluation on plain radiograph to be valid. Radiographic features include 3:
discontinuity of the cortical and trabecular bone
step off in cortical and trabecular bone
displacement of osseous fragments
presence of abnormal fat pad or elevation of fat pad
Impaction lines or sclerotic bands
CT
CT is useful in detecting occult fractures. Several advantages of CT includes: short acquisition time, ability to acquire volumetric image of the bone, with good spatial resolution. CT is also useful in excluding bone marrow edema, space-occupying lesions such as malignancy, and osteomyelitis. Some features of fractures include 3:
discontinuity of the cortical and trabecular bone
depressed/depressed articular surfaces
increased medullary density
endosteal sclerosis
sclerotic lines in trabecular bone
periosteal thickening
Treatment and prognosis
The fundamentals of fracture healing rely on alignment and immobilization. Alignment may or may not be necessary depending on the degree of displacement, the importance of correct alignment (e.g. index finger vs rib) and the particulars of the patient (e.g. professional athlete vs debilitated elderly).
Immobilization can be achieved in a variety of ways depending on the location and morphology of the fracture.
none (e.g. most rib fractures)
sling (e.g. many clavicular fractures)
cast (e.g. many forearm fractures)
internal fixation (e.g. most hip fractures): open vs closed reduction




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.