A pancreas transplant is a major surgical procedure in which a donor pancreas is transplanted into a recipient. The donor pancreas is typically cadaveric, but may rarely be a segment from a living donor 1. The transplant is meant to establish normoglycemia in patients with diabetes mellitus, typically type 1, though similar outcomes may be achieved with patients with type 2 diabetes mellitus 2.
On this page:
Indications
Transplants are typically performed in patients with diabetic complications or hyperlabile diabetes. To be a candidate for transplant, the risks and complications from the patient's diabetes must outweigh the risk from surgical complications and post procedure immunosuppression, which must be continued for life 4.
Pancreas transplants may be performed for both type 1 and type 2 diabetes, although it is more commonly performed for type 1. Patients with type 1 diabetes often have absent or minimal serum levels of C-peptide (<1 mg/ml), and are considered better surgical candidates 5.
Indications for pancreas transplants and simultaneous pancreas and kidney transplants are continually evolving. The American Diabetes Association 2006 indications for pancreas transplant are 4:
hyperlabile diabetes defined by frequent acute severe metabolic complications (hypoglycemia, marked hyperglycemia, and ketoacidosis) requiring medical attention
clinical and emotional problems with insulin therapy that are incapacitating
consistent failure of insulin based management to prevent complications
presence of (two or more) diabetic complications that are progressive and unresponsive to intensive insulin therapy
early diabetic nephropathy
proliferative retinopathy
symptomatic peripheral or autonomic neuropathy
vasculopathy with accelerated atherosclerosis
The indications for a pancreas and kidney transplant are:
CKD stages 4 or 5 (creatinine clearance <30 ml/min) with type 1 diabetes and with other diabetic complications
prior renal transplant which is failing in a type 1 diabetic
Types of pancreas transplantation
The most common types of pancreas transplants are 3:
SPK: simultaneous pancreas and kidney transplant (~78% of cases)
PAK: pancreas after kidney transplant (~16% of cases)
PTA: pancreas transplant alone (~7% of cases)
Procedure
Technique
The pancreas is procured from the donor in a variety of ways, depending on the operative needs. The second portion of the duodenum (containing the ampulla of Vater) is recovered with the pancreas.
The technique generally consists of 3:
incision and exposure: intraperitoneal or retroperitoneal approaches possible
donor portal vein mobilization: to confluence of splenic vein and superior mesenteric vein
-
arterial reconstruction, involving either:
-
donor Y-graft:
donor internal iliac artery is anastomosed end-to-end with the recipient external iliac artery
the other ends of the donor internal iliac artery bifurcation are anastomosed end-to-end with the donor pancreas superior mesenteric artery (SMA) and splenic artery
systemic venous drainage
-
direct splenic artery to SMA
donor SMA is anastomosed to recipient external iliac artery
donor splenic artery is anastomosed end-to-side with the donor SMA
portal venous drainage
-
end-to-side or side-to-side anastomosis of the donor duodenal segment with recipient jejunum
Radiographic features
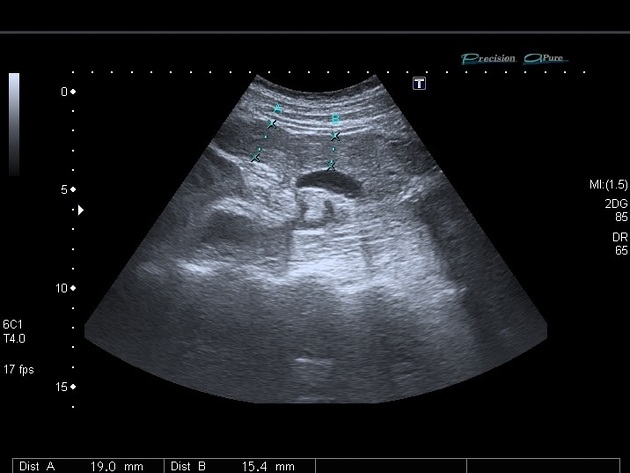
Ultrasound
Ultrasound is considered the first-line modality in evaluating the transplanted pancreas and vasculature 3, demonstrating the following features:
-
grayscale:
transplant is hypoechoic relative to mesenteric fat
useful to evaluate for peripancreatic fluid collections
-
color Doppler / power Doppler:
evaluate flow to all parts of the transplant parenchyma
evaluation of patency of arterial and venous anastomoses
-
spectral Doppler
arterial waveforms: sharp upstroke with continuous diastolic flow
venous waveforms: monophasic
Ultrasound may be limited by the presence of overlying bowel gas, which is common due to the frequent anastomosis to the small bowel.
One of the primary roles of ultrasound is to exclude thrombosis. Ultrasound has limited ability to diagnose rejection. Rejection and pancreatitis may appear similarly.
CT
CT is superior to ultrasound in cases of suspected abdominal infections, bowel complications, graft rejection, or pancreatitis 3. It is typically performed with oral contrast.
MRI
Given the common presence of contraindications to IV contrast material in donor recipients, MR is superior to CT in assessing vascular complications 3.
Complications
Vascular complications of a pancreas transplant are conceptually similar to a renal transplant, and include 3
graft rejection
anastomotic breakdown and hemorrhage
stenosis or thrombosis of the arterial inflow or venous outflow
Bowel complications may also occur 3:
-
usually from adhesions, but internal hernia may occur
anastomotic exocrine leak
colitis, specifically pseudomembranous and cytomegalovirus colitis
Other complications include 3:
fluid collections, especially peripancreatic fluid collection
post-transplant lymphoproliferative/lymphoproliferation disorder (PTLD)
Post-grafting pancreatitis is also possible.
Prognosis
Unadjusted patient survival rates 6:
-
SPK:
1 year: 95-98%
3 years: 91-93%
5 years: 87%
10 years: 70%
-
PAK:
1 year: 95-98%
3 years: 91-93%
5 years: 84%
10 years: 65%
-
PTA:
1 year: 95-98%
3 years: 91-93%
5 years: 89%
10 years: 73%
SPK patients demonstrate the best pancreas graft survival rates.
Practical points
the donor duodenum sometimes may not fill well with oral contrast and can simulate a perianastomotic fluid collection





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.