Hepatic metastases are 18-40 times more common than primary liver tumors 6. Ultrasound, CT, and MRI are helpful in detecting hepatic metastases and evaluation across multiple post-contrast CT series, or MRI pulse sequences are necessary.
On this page:
Epidemiology
The demographics of patients with liver metastases will mirror that of the underlying primaries. Incidence, therefore, increases with age.
Clinical presentation
Liver metastases are usually asymptomatic and found during the workup of a malignancy. If the hepatic metastatic burden is large, then the presentation or symptoms related to the liver disease may include:
localized pain and tenderness due to capsular stretching
disordered liver metabolic function
low-grade fever 2
Pathology
The most common sites of primary malignancy that metastasize to the liver are 2:
-
gastrointestinal tract (via portal circulation)
colorectal carcinoma (termed colorectal liver metastases, CRLMs)
-
genitourinary system
essentially all metastatic solid malignancies
Radiographic features
One of the main difficulties in liver imaging for metastatic disease is the high prevalence of benign liver lesions that can be misinterpreted as evidence of metastatic disease, thus dramatically changing a patient's stage, and therefore treatment options. Liver hemangiomas, and to a lesser degree focal nodular hyperplasia (FNH), are the main sources of confusion 3. Additionally, pseudolesions (e.g. transient hepatic attenuation differences (THADs), focal fatty sparing / focal fatty change) may further muddy the waters. Therefore, an understanding of the various appearances of metastatic disease is crucial.
Ultrasound
Routine greyscale ultrasound, contrast-enhanced ultrasound, and intra-operative ultrasound all have roles to play.
Unfortunately, not only do metastases have a wide range of appearances, but background echogenicity changes of the liver due to fatty change make absolute statements difficult to make. In general, however, metastases may appear as 3:
rounded and well-defined
positive mass effect with distortion of adjacent vessels
hypoechoic: most common ~65% and is a concerning feature 8
hypoechoic halo due to compressed and fat-spared liver
cystic, calcified, infiltrative and echogenic appearances are all possible: see liver metastases ultrasound appearances
Contrast-enhanced ultrasound has similar characteristics to CT, able to distinguish between hypovascular liver lesions, and hypervascular liver lesions.
See also: ultrasound appearance of hepatic metastases.
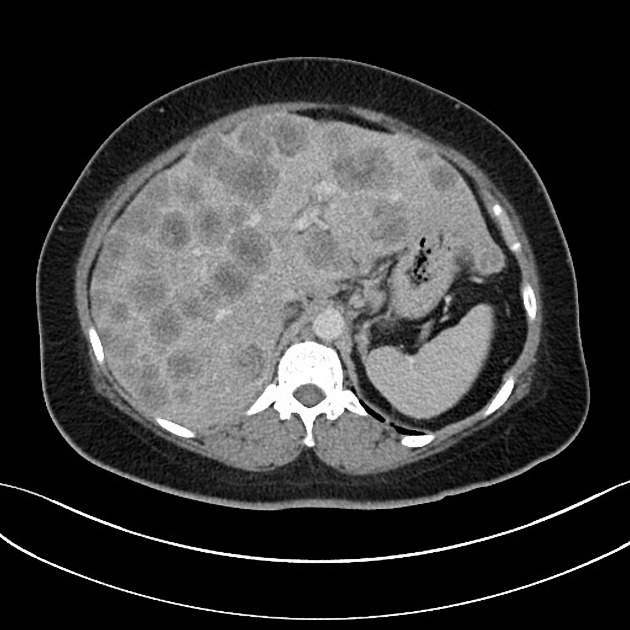
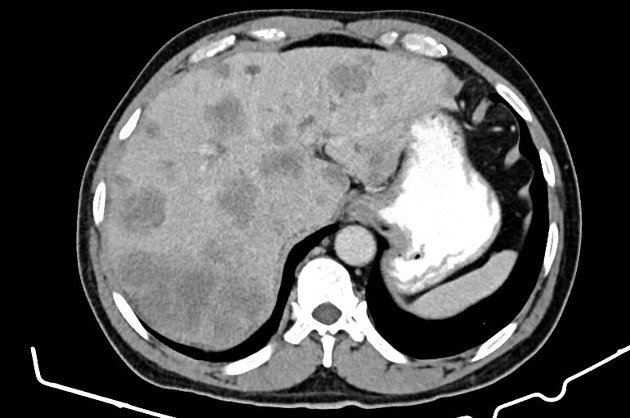
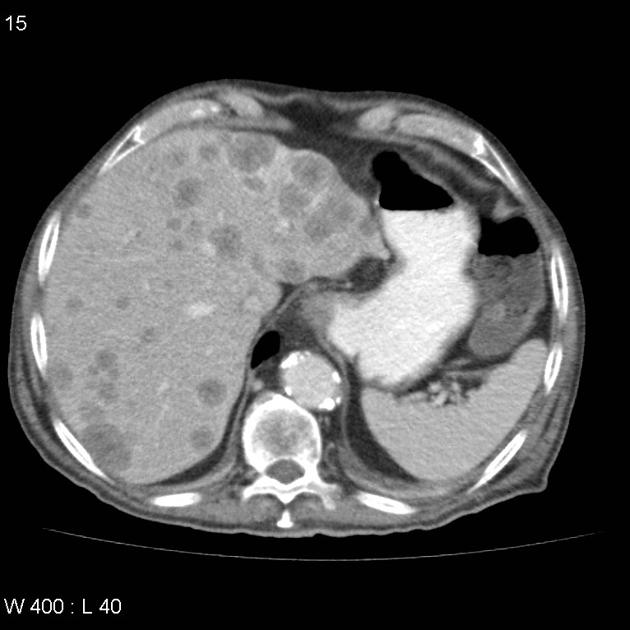
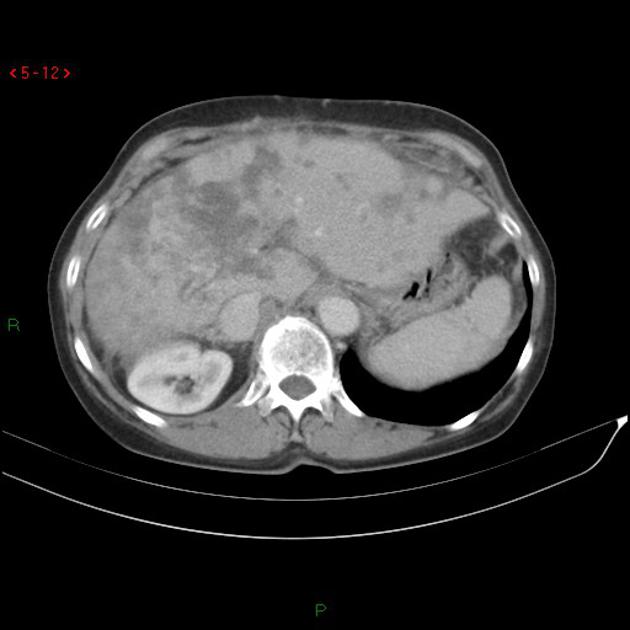
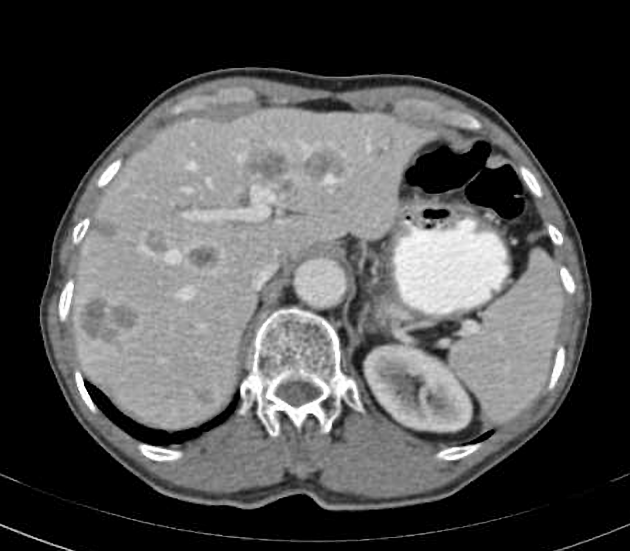
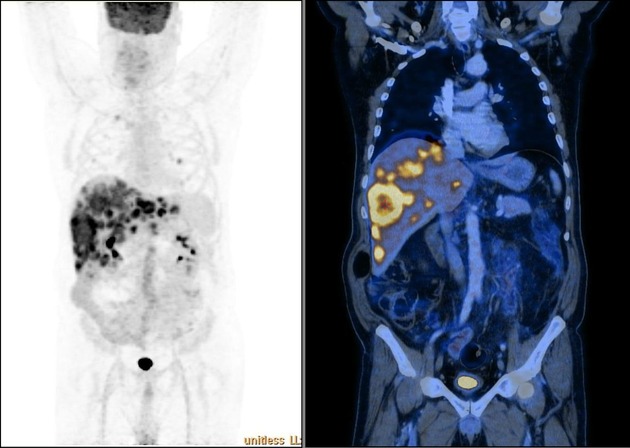
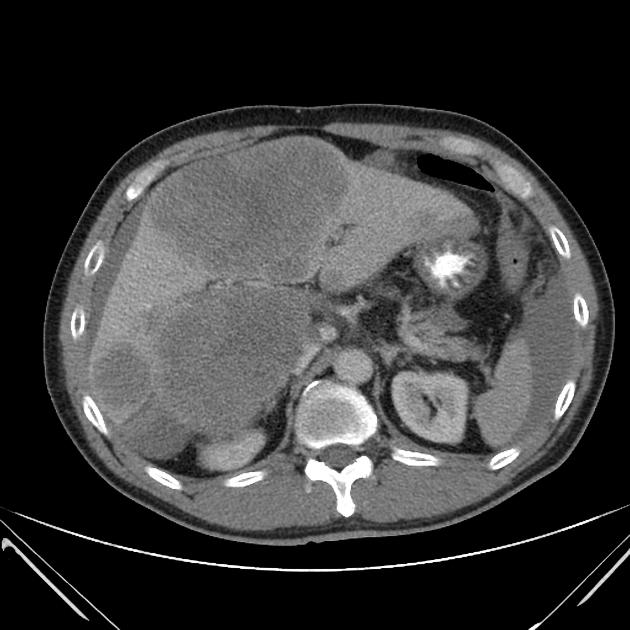
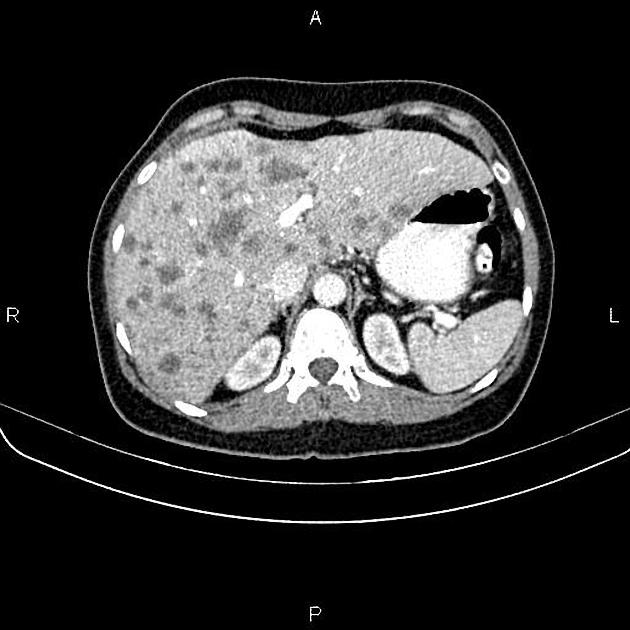
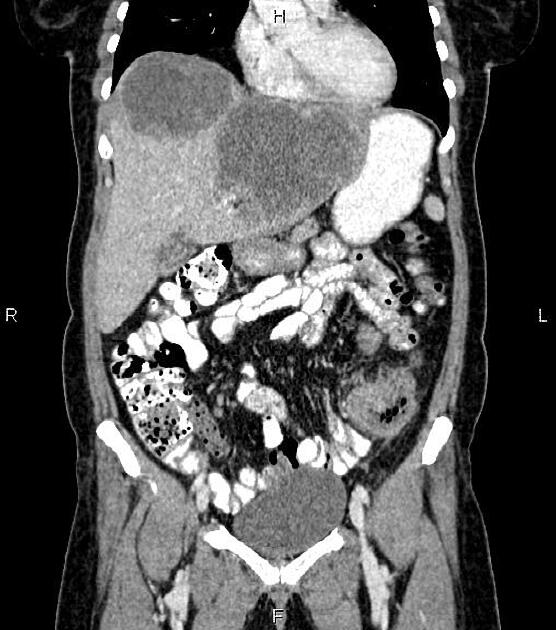
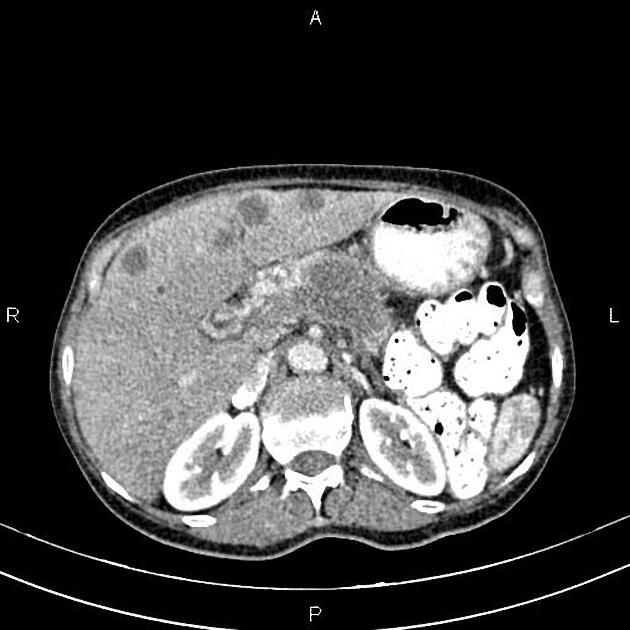
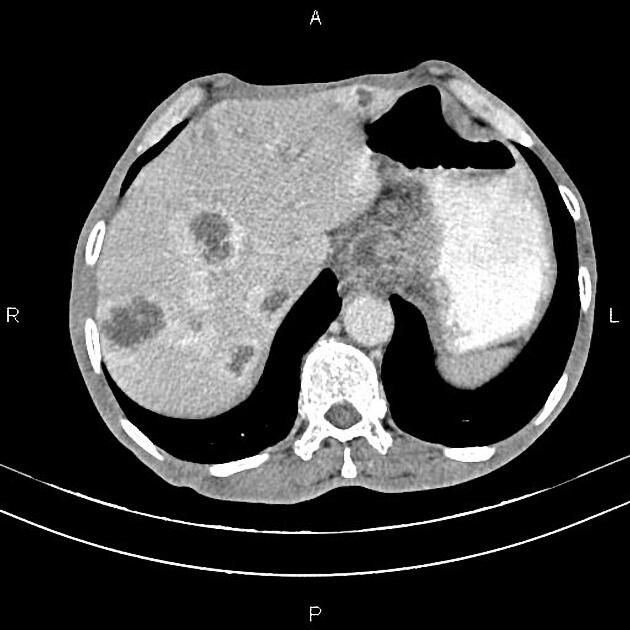
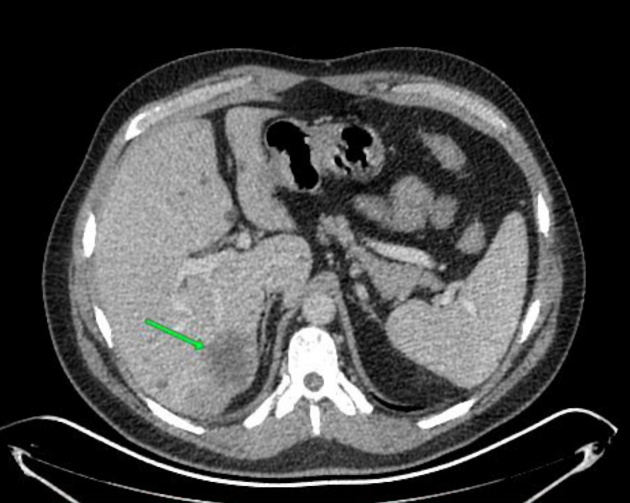
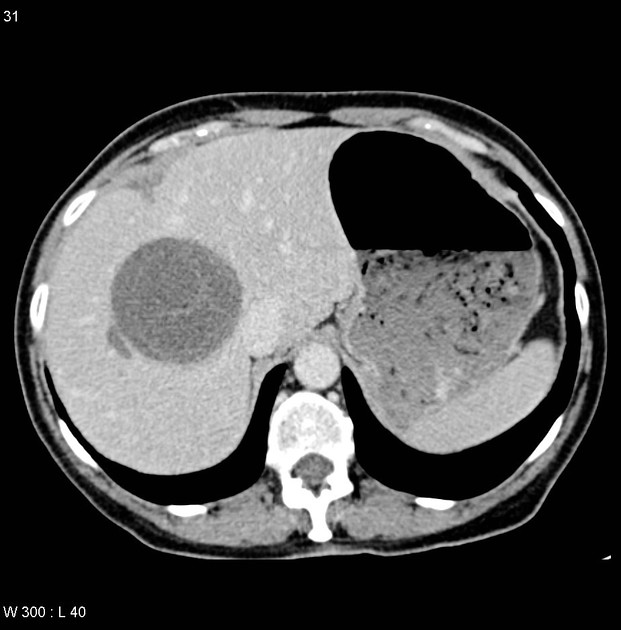
CT
Liver metastases are typically hypoattenuating on unenhanced CT, enhancing less than surrounding liver following contrast 1. If there is concomitant hepatic steatosis, then the lesions may be iso- or even slightly hyperattenuating. Enhancement is typically peripheral, and although there may be central filling in on portal venous phase, the delayed phase will show washout; helpful in distinguishing a metastasis from a hemangioma 1.
Some primaries have a tendency to produce hyper-enhancing metastases, including renal cell carcinoma, thyroid carcinoma, neuroendocrine tumors, etc. (see hypervascular liver lesions).
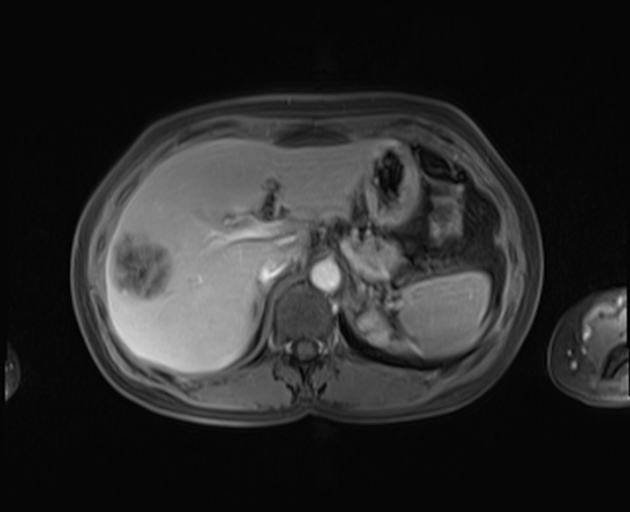
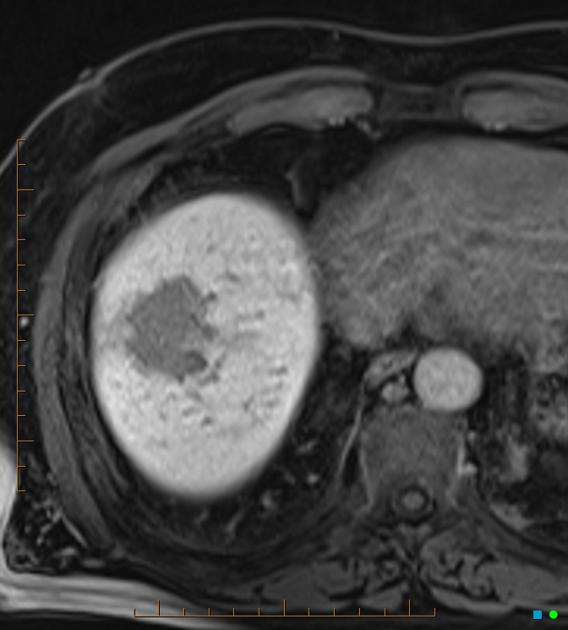
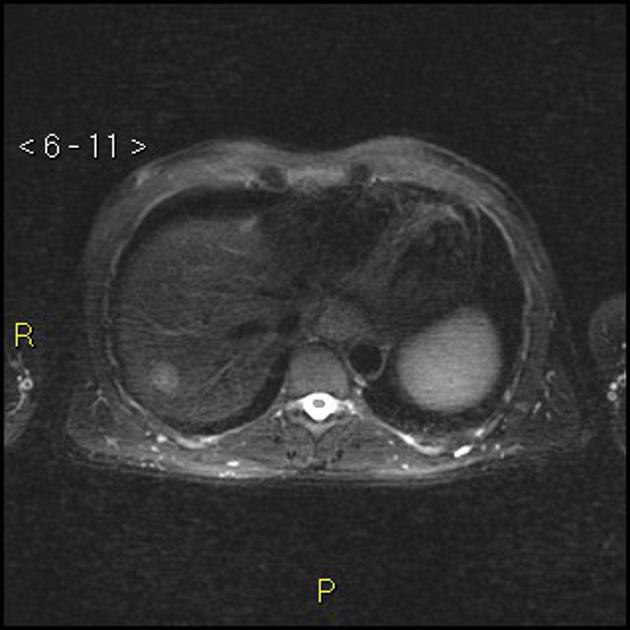
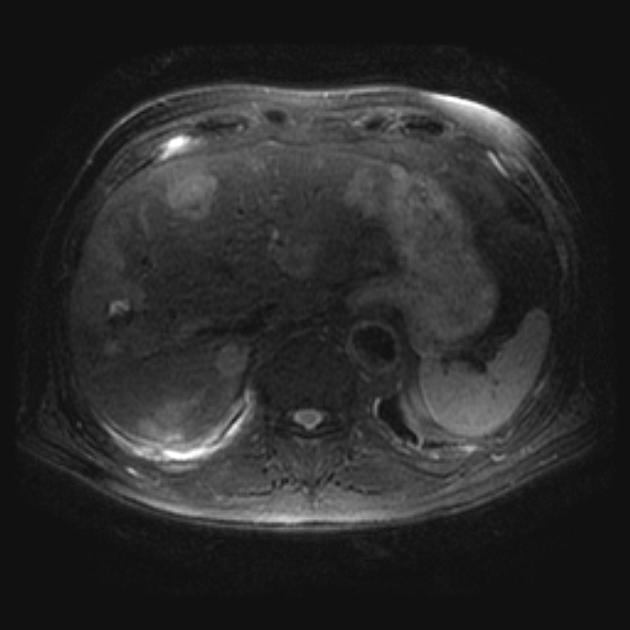
MRI
The appearance of liver metastases on MRI is also variable, but MRI is more sensitive than CT for the detection of liver metastases 5. MRI examination of the liver may involve numerous sequences (see liver MRI protocol), and choice of the gadolinium contrast agent (extracellular contrast agent or Eovist) is an important consideration.
The most frequent appearances are 5:
T1: moderately hypointense
T2: mildly to moderately hyperintense
-
T1 C+ (Gd): enhancement may be lesional or perilesional (enhancement outside the confines of the T1 delineated lesion) 7
small lesions (<1.5 cm) tend to uniformly enhance
larger lesions (>1.5 cm) tend to show transient rim enhancement (i.e. with washout); helpful feature in distinguishing a metastasis from a liver hemangioma
perilesional enhancement is most commonly seen in colorectal and pancreatic adenocarcinoma metastases 5
-
T1 C+ (Eovist/Primovist):
Eovist/Primovist is often useful for detection and confirmation of metastatic disease
on the delayed phase, metastatic lesions do not retain any Eovist/Primovist and essentially appear as "holes" in the liver
DWI/ADC b600-800: restricted diffusion with ADC values lower than those of the surrounding parenchyma18
Fluid-fluid levels are considered a specific finding for neuroendocrine tumor metastases 9.
Radiology report
The following should be included in the radiology report 17:
number, size and location (using the Couinaud classification) of tumor(s)
relationship to the main portal pedicles and hepatic veins
portal vein patency
radiological signs of portal hypertension
extrahepatic metastatic disease
Treatment and prognosis
Hepatic metastases from colorectal adenocarcinoma can potentially be treated with hepatic metastasectomy, since they may be the only site of metastatic disease. Up to 20% of patients undergoing metastasectomy for this indication remain disease-free 10. Multiple staging systems for disease-free survival after metastasectomy have been proposed and are being refined. One of the more frequently used systems (e.g. "Fong" score) includes variables such as 11:
node-negative primary
single hepatic metastasis
hepatic metastasis size <5 cm
CEA <200 ng/mL
disease-free interval >1 year
These variables suggest a better metastasectomy disease-free survival.
Transarterial chemotherapy and radioembolization are other options for the treatment of hepatic metastases. MRI-guided adaptive radiation therapy is a new and unique method of liver tumor treatment for both primary and metastatic disease 16.
Differential diagnosis
General differential imaging considerations include:
hepatic hemangioma: usually hyperechoic, geographic, no mass effect, discontinuous peripheral nodular enhancement and 'filling in' 1
multiple hepatic cysts: no enhancement or mural nodules; can be hyper-dense/intense due to blood or infection
hepatocellular carcinoma (HCC): hypervascular, more often solitary, possible hypoechoic US halo, cirrhotic liver, vascular invasion
-
focal nodular hyperplasia (FNH)
often younger patients
central scar, with persistent delayed enhancement
transient hepatic attenuation differences (THAD): often in cirrhosis
multifocal fatty infiltration/focal fatty sparing: periligamentous, perivascular distribution; MRI in-out phase signal changes, vessels course through "lesions"; no mass effect
cholangiocarcinoma: delayed enhancement, capsular retraction
multiple liver abscesses: possible CT cluster sign and right pleural effusion
primary non-Hodgkin lymphoma 12
















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.