The accessory nerve, also called the spinal accessory nerve, or historically, the nerve of Willis, is the eleventh cranial nerve (CN XI) and is composed of two parts, the cranial part and the spinal part (TA: nervus accessorius or nervus cranialis XI).
On this page:
Connections and course
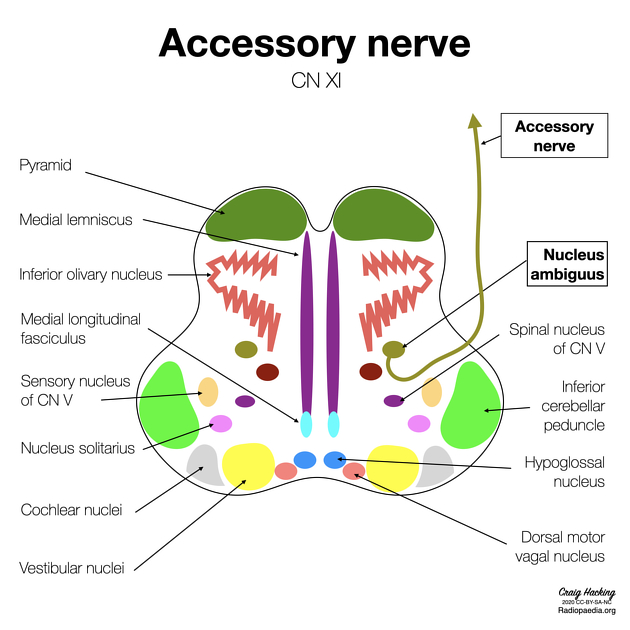
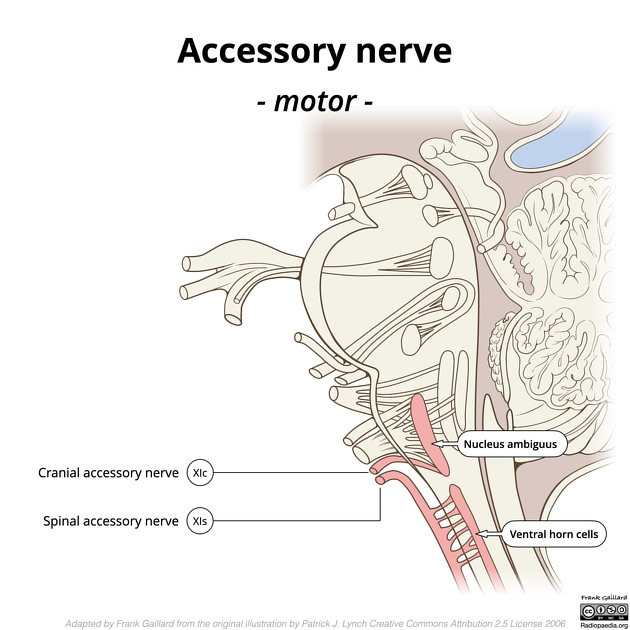
The cranial part (accessory portion) is the smaller of the two. Its fibers arise from the cells of the nucleus ambiguus and emerge as four or five delicate rootlets from the side of the medulla oblongata, below the roots of the vagus nerve. It runs laterally to the jugular foramen, where it interchanges fibers with the spinal portion or becomes united to it for a short distance; here it is also connected by one or two filaments with the jugular ganglion of the vagus. It then passes through the jugular foramen, separates from the spinal portion and continues over the surface of the ganglion nodosum of the vagus, to the surface of which it is adherent, and is distributed principally to the pharyngeal and superior laryngeal branches of the vagus. Through the pharyngeal branch, it probably supplies the musculus uvulae and levator veli palatini. Some filaments from it continue into the trunk of the vagus below the ganglion, to be distributed with the recurrent nerve and probably also with the cardiac nerves.
The spinal part (spinal portion) is firm in texture. Its fibers arise from the ventral horn cells in the cord between C1 and C5 of the cervical plexus. The fibers emerge from the cord laterally between the anterior and posterior spinal nerve roots to form a single trunk, which ascends into the skull through the foramen magnum. It then exits the skull through the jugular foramen, through which it passes, lying in the same sheath of dura mater as the vagus but separated from it by a fold of the arachnoid mater.
- in the jugular foramen, it receives one or two filaments from the cranial part of the nerve, or else joins it for a short distance and then separates from it again
- as it exits from the jugular foramen, it runs backwards then descends obliquely behind the digastric and stylohyoid muscles to the upper part of the sternocleidomastoid muscle; it pierces this muscle and courses obliquely across the posterior triangle of the neck, to end in the deep surface of the trapezius muscle
- as it traverses the sternocleidomastoid muscle, it gives several filaments to the muscle and joins with branches from the second cervical nerve
- in the posterior triangle, it unites with the second and third cervical nerves, while beneath the trapezius it forms a plexus with the third and fourth cervical nerves, and from this plexus fibers are distributed to the muscle
- most consider the cranial part of the eleventh cranial nerve to be functional part of the vagus nerve
Functions
The accessory nerve is responsible for the motor innervation of the sternocleidomastoid and trapezius muscles.
- the sternocleidomastoid muscle acts in elevation of the thoracic cage and shoulder girdle, or, with fixation of the limb, will act in lateral flexion of the head to the shoulder on the same side and rotate the head to direct the chin upward to the opposite side. Therefore, injury of the a spinal accessory nerve will cause deficit in the movements of the head to the contralateral side 4
- the trapezius muscle is one of several muscles that elevate the shoulder girdle and retract the girdle dorsally
Related pathology
Injury to the accessory nerve presents clinically as:
- inability to shrug one's shoulders, due to the paralysis of the trapezius muscle
- inability of head rotation due to paralysis of the sternocleidomastoid muscle
Clinical landmarks
- the spinal accessory nerve can be identified entering the deep surface of the sternocleidomastoid muscle 4 cm or more below the mastoid process
- it can be located at Erb's point just superior to where the greater auricular nerve surfaces from the deep neck
- the spinal accessory nerve can also be located readily in the lateral neck at the point where it disappears under the deep surface of the trapezius muscle, roughly two fingerbreadths superior to the clavicle, at the anterior margin of the trapezius muscle









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.