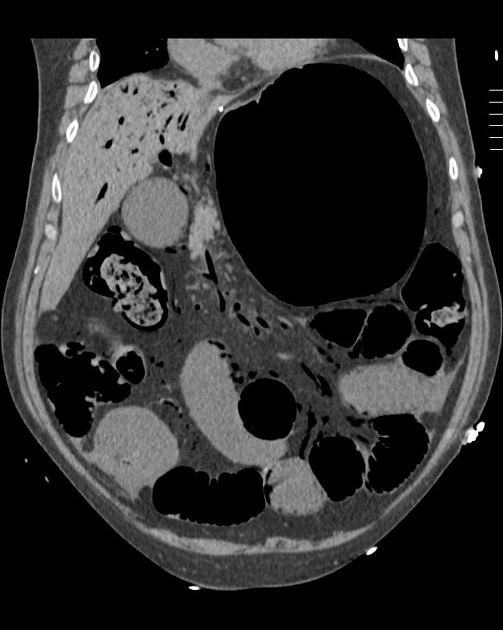
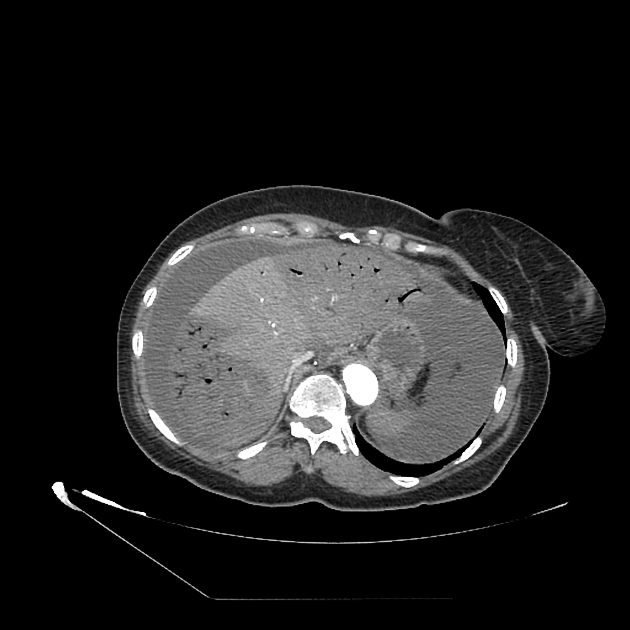
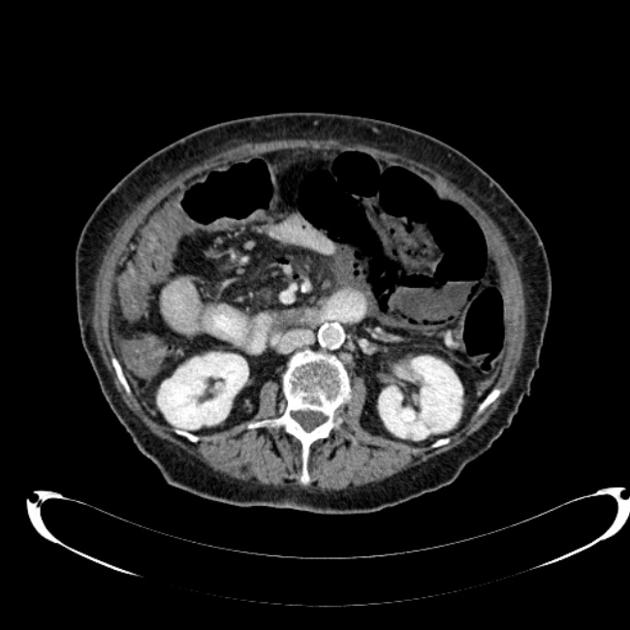
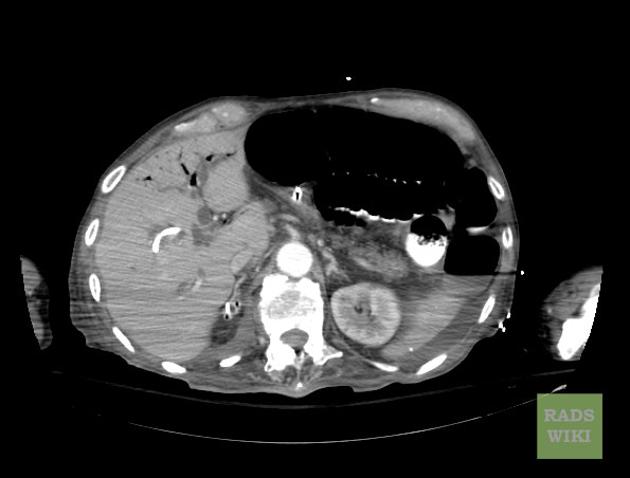
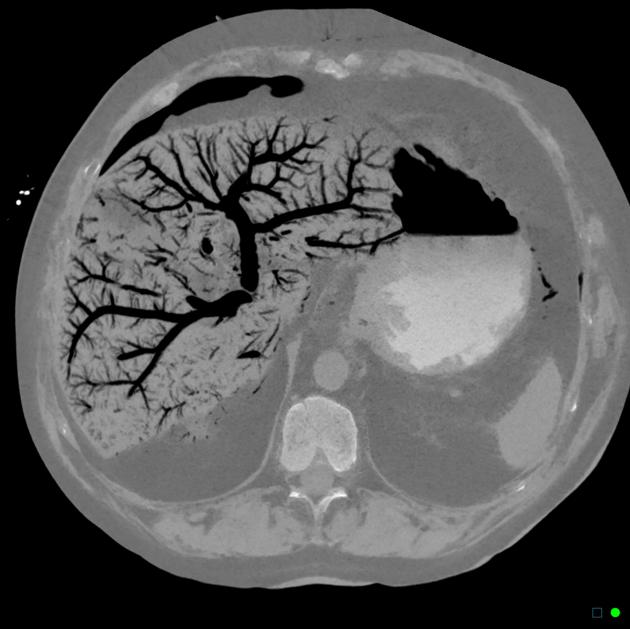
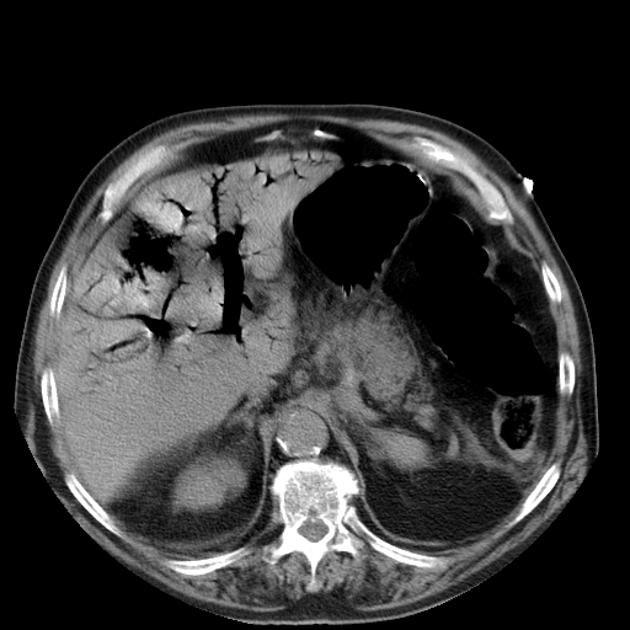
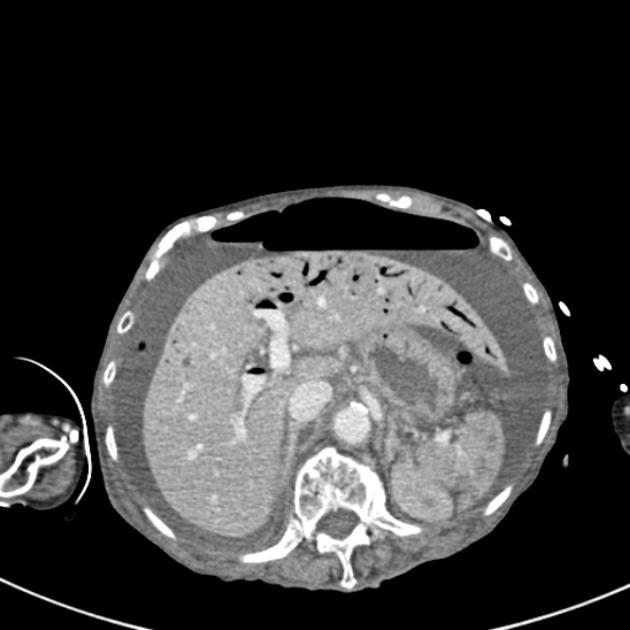
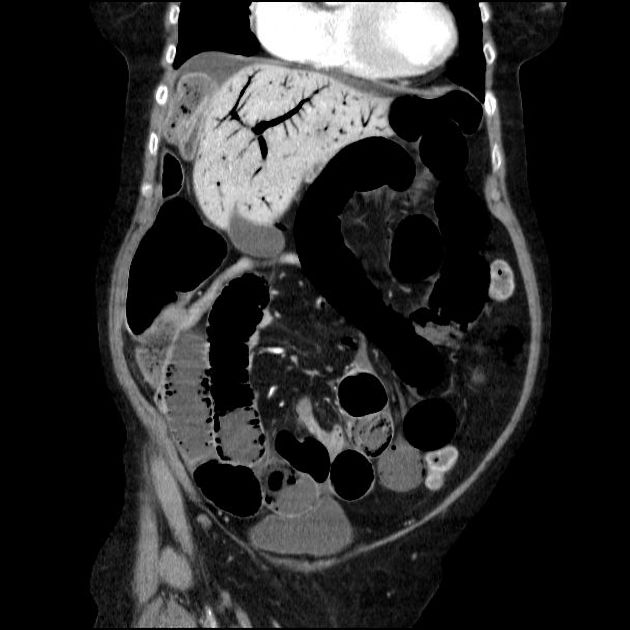
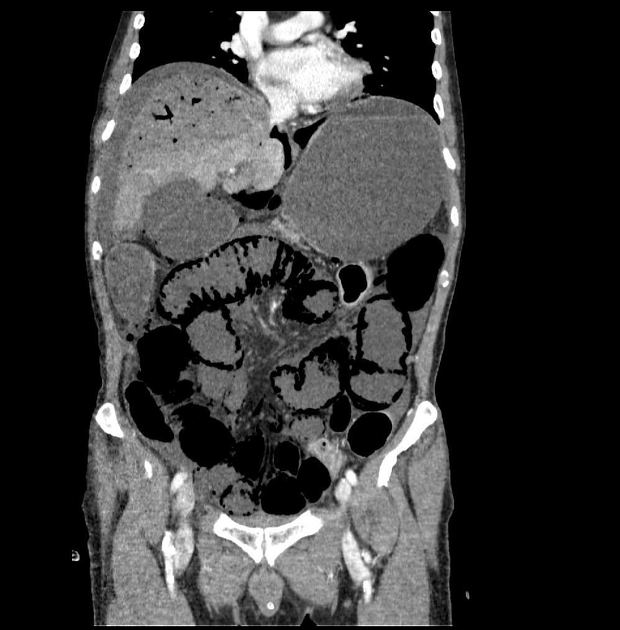
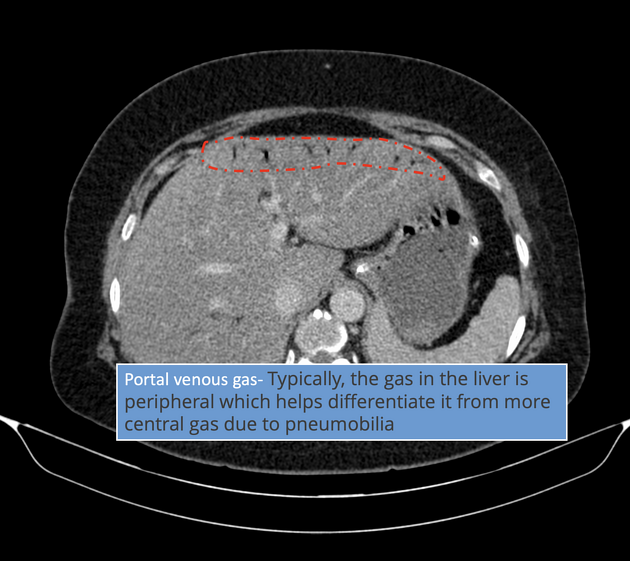
Portal venous gas, also known as pneumatosis portalis, is the accumulation of gas in the portal vein and its branches. It needs to be distinguished from pneumobilia, although this is usually not too problematic when associated findings are taken into account along with the pattern of gas (i.e. peripheral in portal venous gas, central in pneumobilia).
On this page:
Pathology
Etiology
Although traditionally considered a harbinger of death, portal venous gas is increasingly recognized in a variety of conditions, many of which do not carry as high mortality or morbidity risks.
Causes of portal venous gas are best divided according to the age of the patient:
-
child
postoperative finding in corrective bowel surgery
-
adult
-
alterations of the bowel wall
ischemic bowel (usually mural gas as well as mesenteric gas: mortality of 75-90%, but gas is not an independent predictor)
necrotic/ulcerated colorectal carcinoma (CRC)
perforated peptic ulcer
-
bowel luminal distention
iatrogenic gastric and bowel dilatation (e.g. upper and lower endoscopic procedures, enemas)
paralytic ileus or mechanical bowel obstruction
barotrauma
-
intra-abdominal sepsis
-
unknown mechanism
corticosteroid usage
diarrhea 1
cardiopulmonary resuscitation 8
-
Radiographic features
Plain radiograph
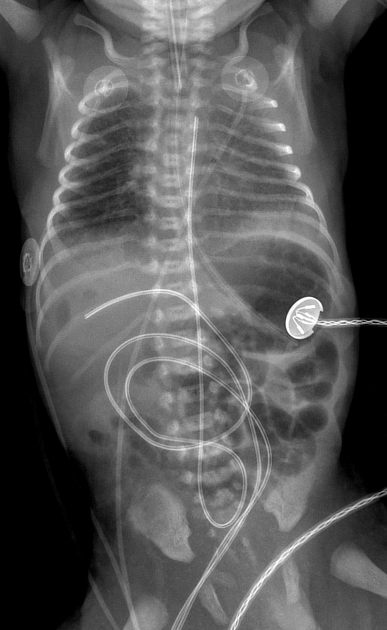
Branching lucencies projected in the liver or vessels coursing towards the liver.
Ultrasound
Gas in the portal veins usually manifests as echogenic mobile foci in the lumen of the portal vein. Doppler ultrasound will demonstrate sharp spikes on both sides of the basal line on the Doppler spectral display 7.
CT
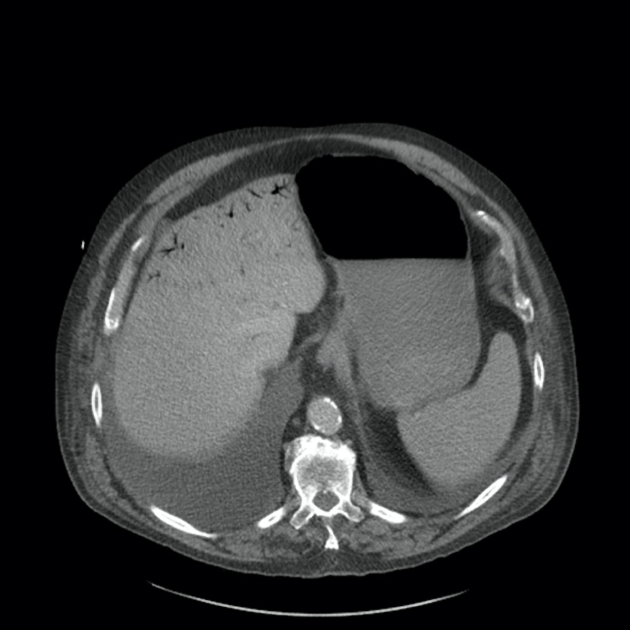
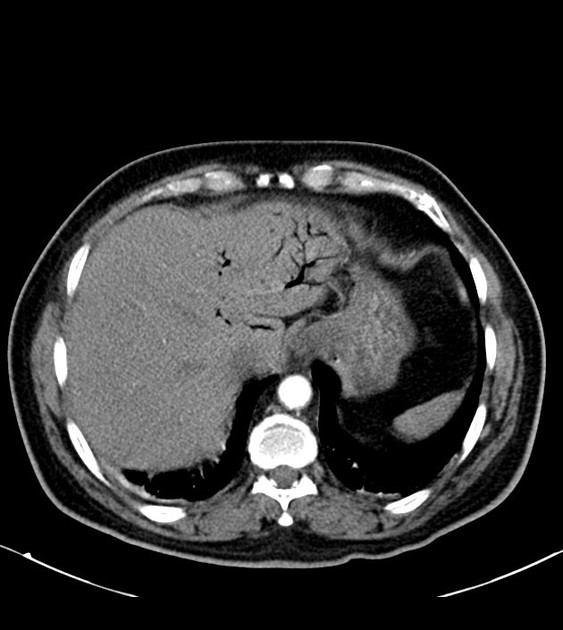
Similar to x-ray features, portal venous gas manifests on CT as branching gaseous foci of low density in the liver, portal vein and its tributaries. The vessel-gas interface may cause streak artifact. Typically, the gas in the liver is peripheral which helps differentiate it from more central gas due to pneumobilia.
History and etymology
The first description of hepatic portal venous gas as a radiological observation was in 1955 by Wolfe and Evens 9.









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.