Respiratory bronchiolitis interstitial lung disease (RB-ILD) is a clinical diagnosis. The CT features are indistinguishable from respiratory bronchiolitis (RB) and should be reported as such.
On this page:
Epidemiology
In almost all cases, respiratory bronchiolitis-interstitial lung disease is associated with heavy tobacco smoking (usually 30 pack-years or more) and is often seen in 30-40 years age group.
Clinical presentation
Chronic cough and progressive dyspnea 4 differentiate RB-ILD from RB. Inspiratory crackles are heard in up to half of patients. Clubbing is rare 1. RB-ILD is a clinical diagnosis.
Pathology
On lung biopsy of respiratory bronchiolitis-interstitial lung disease, pigment-laden macrophages are found within alveoli, and peribronchial inflammation noted. Unlike simple respiratory bronchiolitis, fibrosis extends beyond the tissues immediately adjacent to respiratory bronchioles and extends into alveolar septae.
Histologically respiratory bronchiolitis-interstitial lung disease is very similar to desquamative interstitial pneumonia (DIP) and many authors feel that the two conditions are closely related, or even variants of the same condition 3. It has even been suggested that DIP should be abolished altogether, and simply thought of as end-stage/severe RB-ILD 5.
Radiographic features
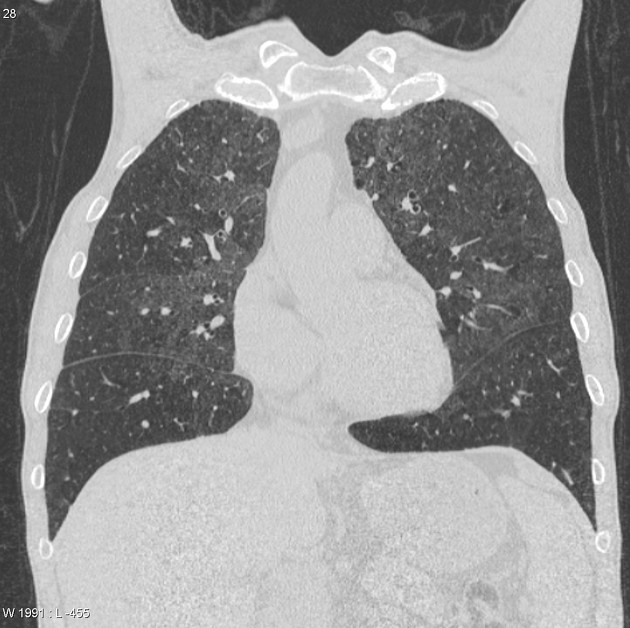
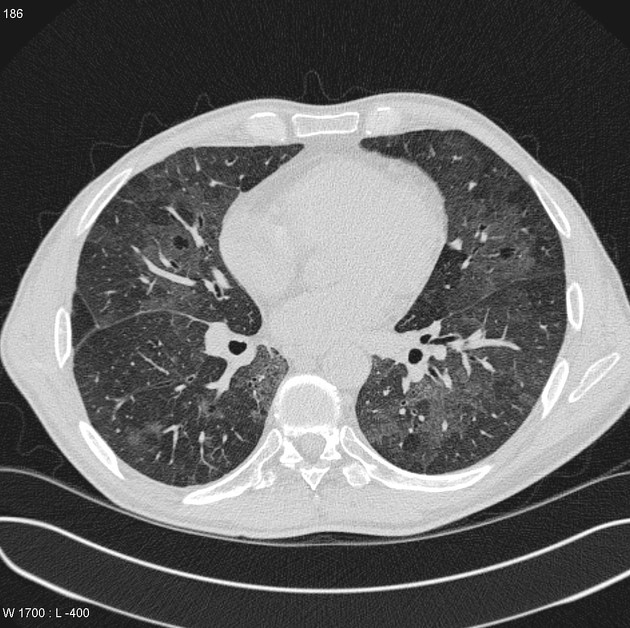
CT
ground glass opacities: may have a slight upper zone predilection 9
poorly defined centrilobular nodules
no particular distribution with both upper and lower zones potentially affected
if advanced, fibrosis may be evident typically affecting the subpleural regions and more so in the lower lung zones
patchy areas of hypoattenuation (~40%) with a lower lung predominance 10
-
other changes related to smoking
bronchial wall thickening: can be central +/- peripheral
Treatment and prognosis
Usually, no treatment is required for respiratory bronchiolitis-interstitial lung disease other than giving up smoking.
History and etymology
It was first described in 1974 by the American pulmonologist Dennis E Niewoehner (1940-2020) 15 and colleagues 11,13.
Differential diagnosis
With typical HRCT chest appearances consider:
-
non-specific interstitial pneumonitis (NSIP)
changes of fibrosis: lung volume loss, reticular opacities, and traction bronchiectasis
ground glass opacities have a random distribution
-
non-fibrotic or fibrotic hypersensitivity pneumonitis (HP)
More profuse centrilobular ground glass nodules favors HP over RB-ILD
RB-ILD more likely to have centrilobular emphysematous changes due to relationship with smoking




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.