Pulmonary hamartomas (alternative plural: hamartomata) are benign neoplasms composed of cartilage, connective tissue, muscle, fat, and bone. It is one of the most common benign lung tumors, accounting for ~8% of all lung neoplasms and 6% of solitary pulmonary nodules.
On this page:
Terminology
Pulmonary chondroma has been used interchangeably with pulmonary hamartoma in the past, but due to their histological differences, they should be considered separate entities 14.
Epidemiology
Patients usually present in the 4th and 5th decades of life, which is very uncommon in children. There is a recognized male predilection (M:F = 2.5:1). Most lesions are diagnosed incidentally.
Clinical presentation
Pulmonary hamartomas are usually asymptomatic and found incidentally when imaging the chest for other reasons. It can occasionally present with hemoptysis, bronchial obstruction, and cough (especially endobronchial types) 6.
Pathology
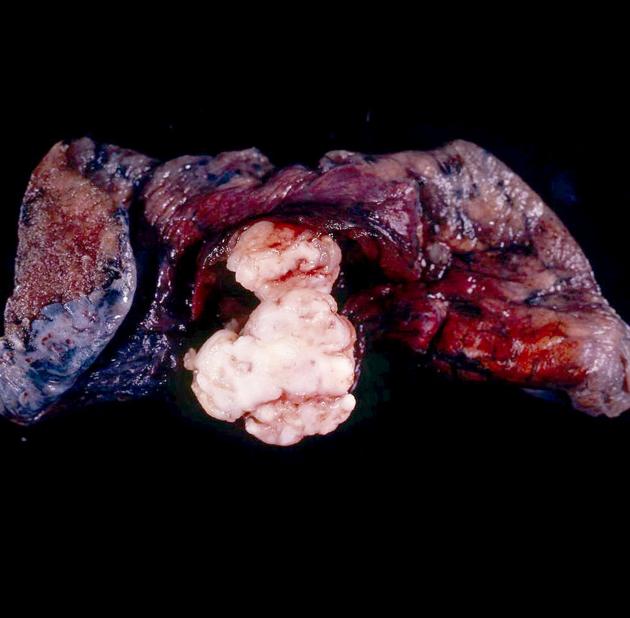
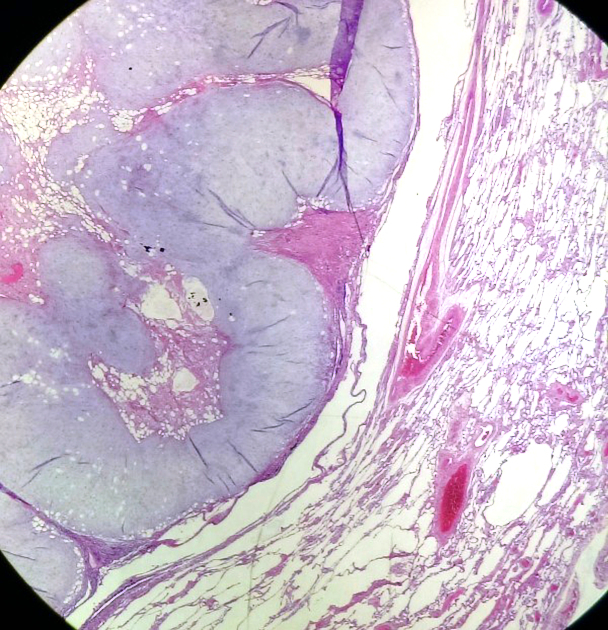
Hamartomas may be chondromatous (more common), leiomyomatous, or a mixture. They contain at least two mesenchymal elements. They are unencapsulated, lobulated tumors with connective tissue septa.
As with any hamartoma, it comprises tissues that normally constitute the lung and bronchi. The tissue elements, although mature, are disorganized. On rare occasions, they contain principally fatty tissue called lipomatous hamartomas or endobronchial lipomas.
Location
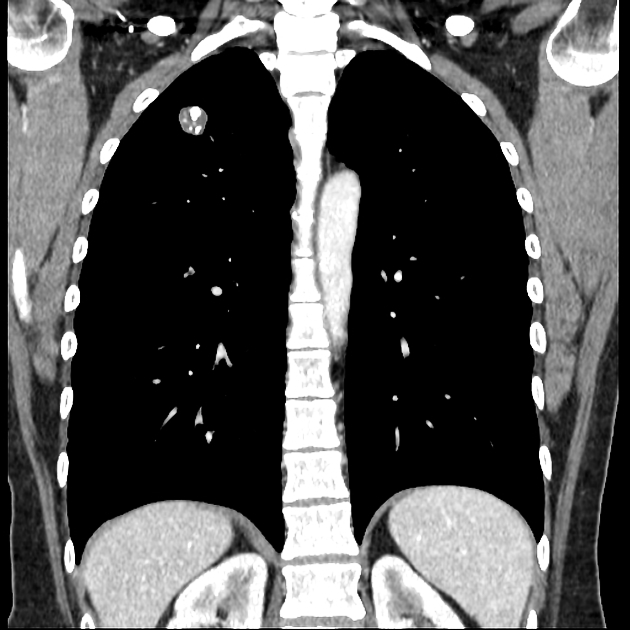
The vast majority of pulmonary hamartomas are located peripherally within the lungs (>90%), with endobronchial hamartomas representing only ~5% (range 1.4-10%) of such lesions 10-11.
Typically, hamartomas manifest incidentally as solitary nodules in the periphery of the lung.
Variants
Radiographic features
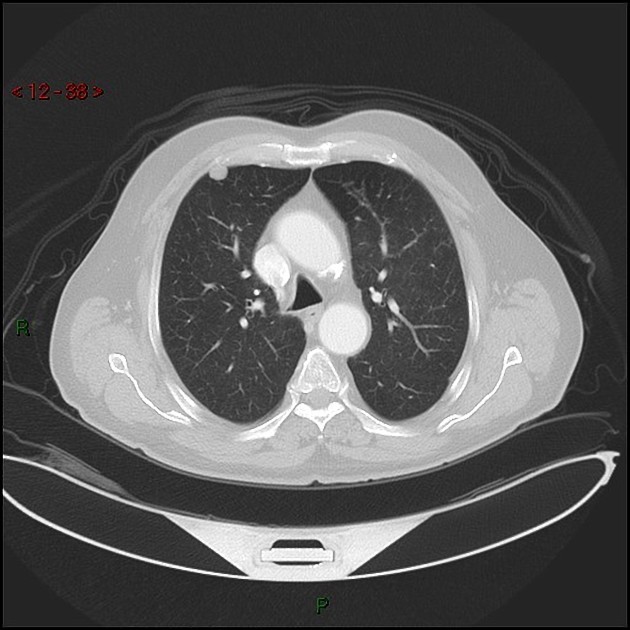
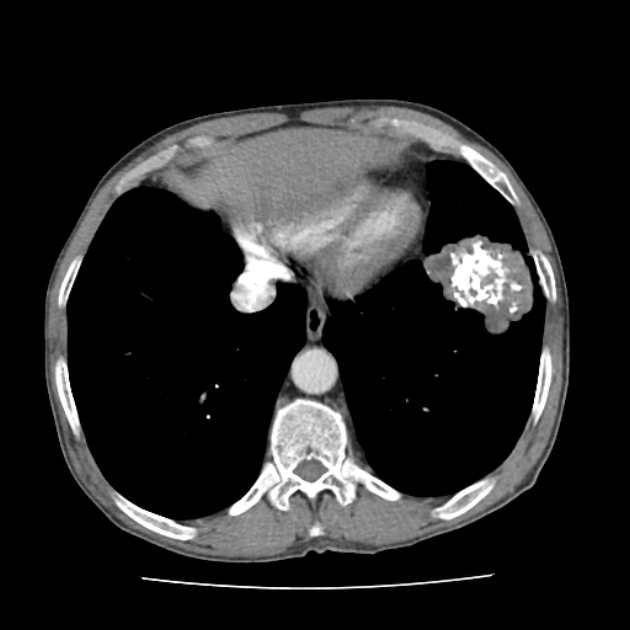
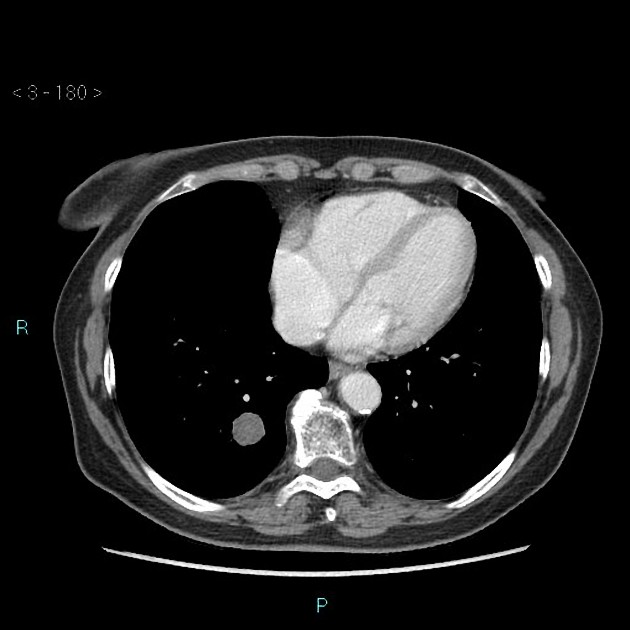
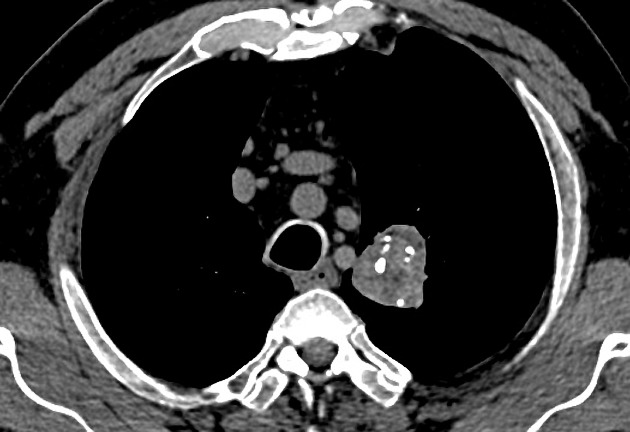
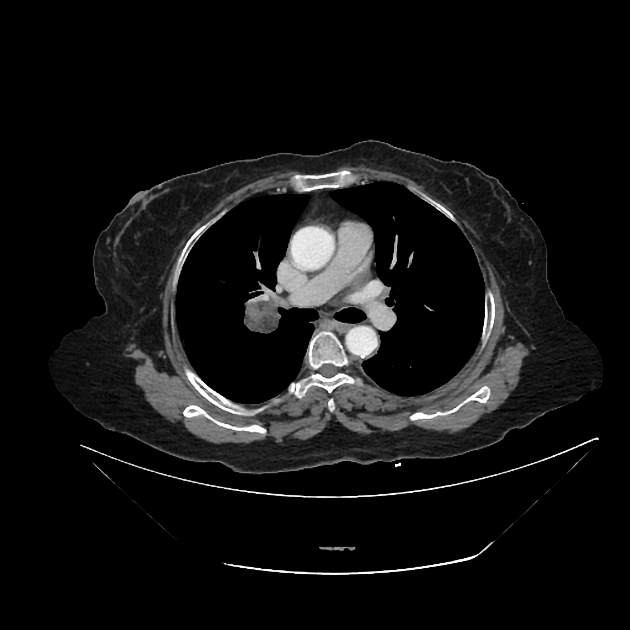
Often discovered incidentally, they are typically well-circumscribed nodules or masses (usually small) with either smooth or lobulated margins. Approximately 60% have fat 7, and approximately 20-30% have calcification/ossification (popcorn-like) 3. Cavitation is not seen.
Size is variable: they can be large (>10 cm), but in most cases, they are <2.5-4 cm in diameter 10,13.
Growth occurs but is very slow, with a typical volume doubling time of over 400 days 9.
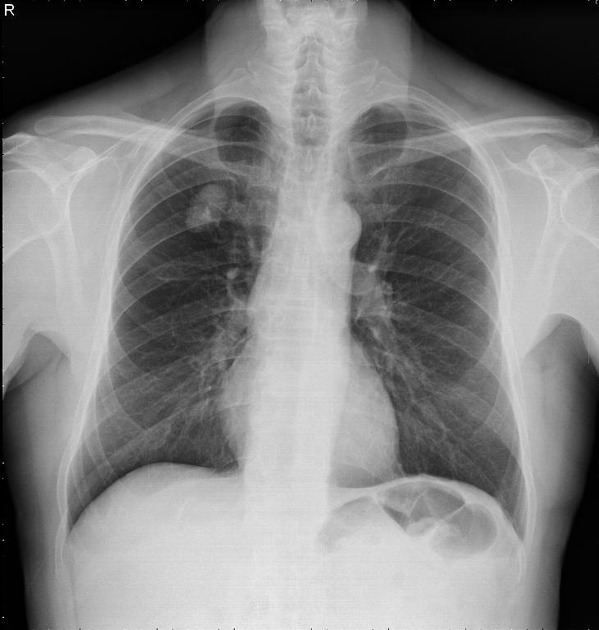
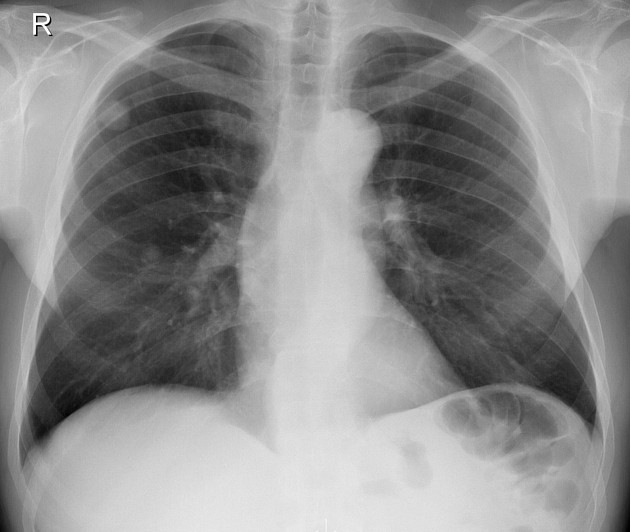
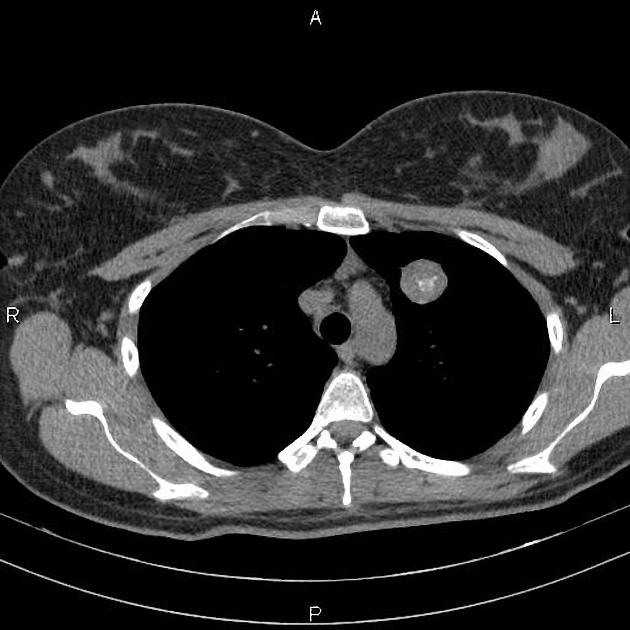
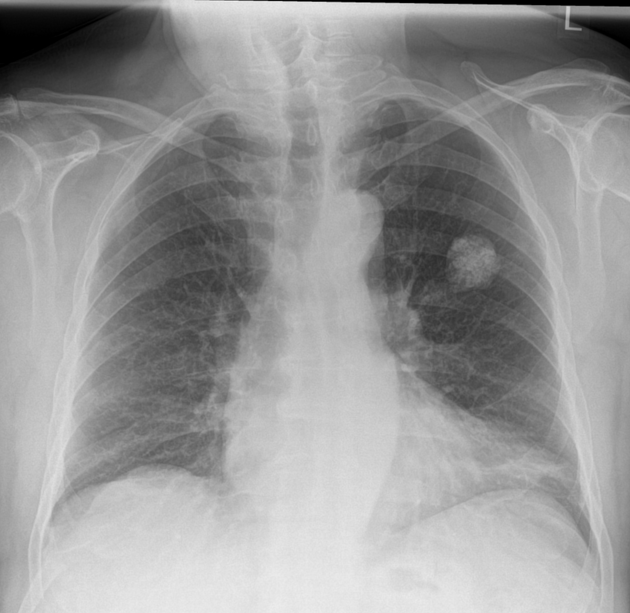
Plain radiograph
Chest radiography is non-specific, demonstrating a soft tissue attenuation, well-circumscribed mass with either smooth or lobulated margins. Calcification (classically popcorn type) may be seen, which can suggest the diagnosis. Fat is difficult to identify with certainty, although the lesion is typically of low density for its size.
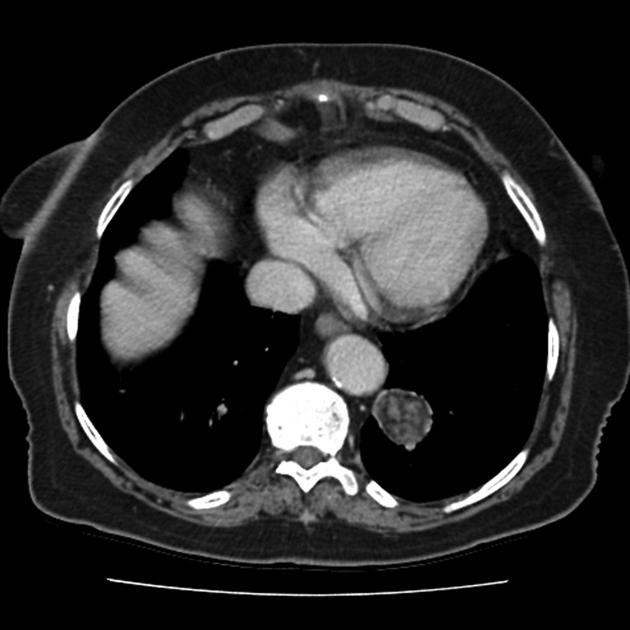
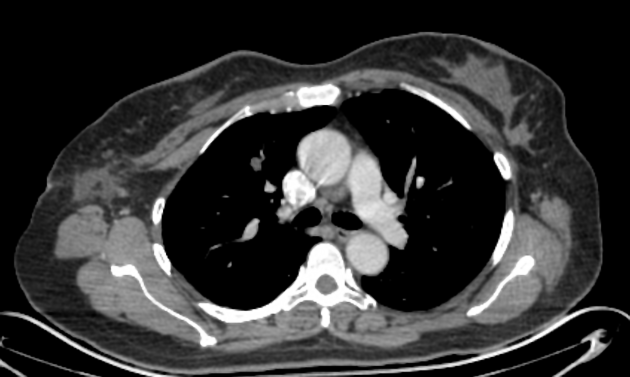
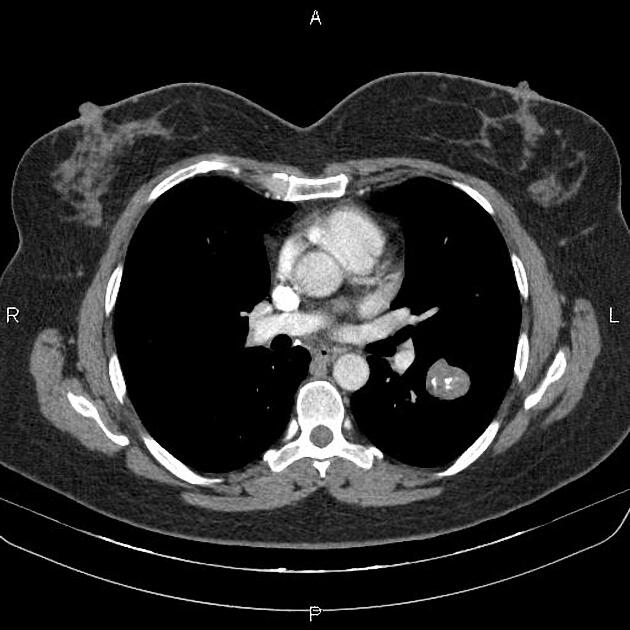
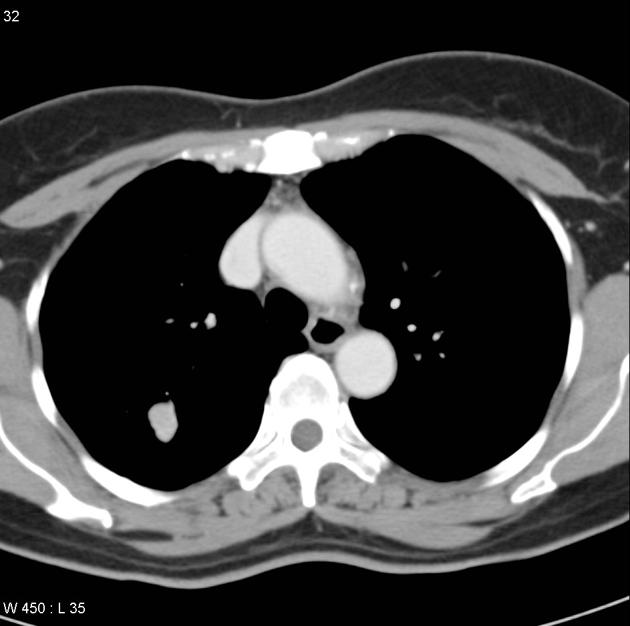
CT
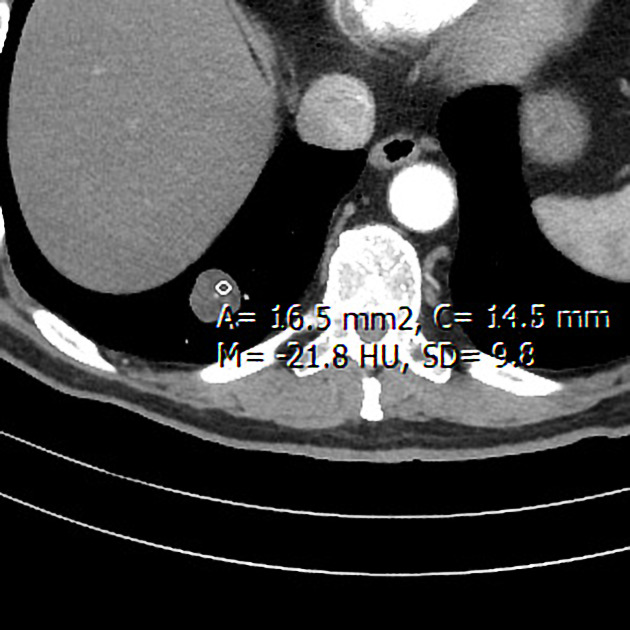
CT is far superior in detecting intralesional fat and calcification. The reported prevalence of calcification in hamartomas on CT varies from 5 to 50%, while fat may be identified in up to 60% of hamartomas at CT. The fat components may be localized or generalized within the nodule.
Fat can be recognized by comparing it to subcutaneous fat and will typically have a Hounsfield measurement of -40 to -120 HU 10. The presence of fat in a well-circumscribed solitary pulmonary nodule that does not demonstrate significant growth is essentially pathognomonic of a pulmonary hamartoma, and no further investigations are required. 7. Unfortunately, fat can only be identified in 60% of lesions. Thin section CT is, therefore, essential to avoid missing small foci of fat.
Calcification is typically dispersed through multiple clumps throughout the lesion in a popcorn configuration 3.
MRI
-
T1: heterogeneous signal
mainly intermediate signal 8
foci of high signal represent fat
low signal regions representing fibrous or calcific material
-
T2:
high signal due to fat and cartilaginous components
low signal regions representing fibrous or calcific material
T1 C+ (Gd): heterogeneous enhancement is seen
Nuclear medicine
PET-CT
Although uncommon, increased avidity may be seen on FDG-PET 7. Thus, further investigation with PET-CT of slow-growing, fat-containing masses is unwarranted, confusing, and contributes to patient radiation dose.
Treatment and prognosis
Malignant transformation is exceedingly rare, and a peripheral small hamartoma with no atypical features can be safely left alone, with infrequent follow-up to exclude growth.
Surgical resection is curative in atypical cases or endobronchial hamartomas causing distal complications. Rigid transbronchial resection is most frequently employed in the latter 12.
Differential diagnosis
On CT consider
-
peripheral pulmonary carcinoid 15
-
can be difficult to differentiate at times, but many carcinoids may have
higher attenuation
more lobulation
more distal nodularity
distal hyperlucency
atelectasis
more bronchial extension and involvement
marked homogenous contrast enhancement
-
The broader differential somewhat depends on whether fat or calcification is identifiable within the lesion.
If fat is visualized, the differential is narrow, with almost all cases representing pulmonary hamartoma. See differential of fat-containing solitary pulmonary nodule.
Calcification also significantly narrows the differential but to a lesser degree. See the differential of a solitary pulmonary nodule with calcification.
If neither fat nor calcification is present, the differential is significantly broader than that of a solitary pulmonary nodule. See the differential of a solitary pulmonary nodule.









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.