Diagnostic HRCT criteria for usual interstitial pneumonia (UIP) pattern - Fleischner society guideline (2018)
In 2018, the Fleischner Society provided updated diagnostic HRCT criteria for usual interstitial pneumonia (UIP) pattern based on literature review and the expert opinion of members. As a part of this white paper, diagnostic HRCT criteria for usual interstitial pneumonia (UIP) pattern were updated.
The 2018 revised diagnostic HRCT criteria for usual interstitial pneumonia (UIP) pattern published by the American Thoracic Society, the European Respiratory Society, the Japanese Respiratory Society, and the Latin American Thoracic Association has converged to a similar categorization of the HRCT findings into four groups.
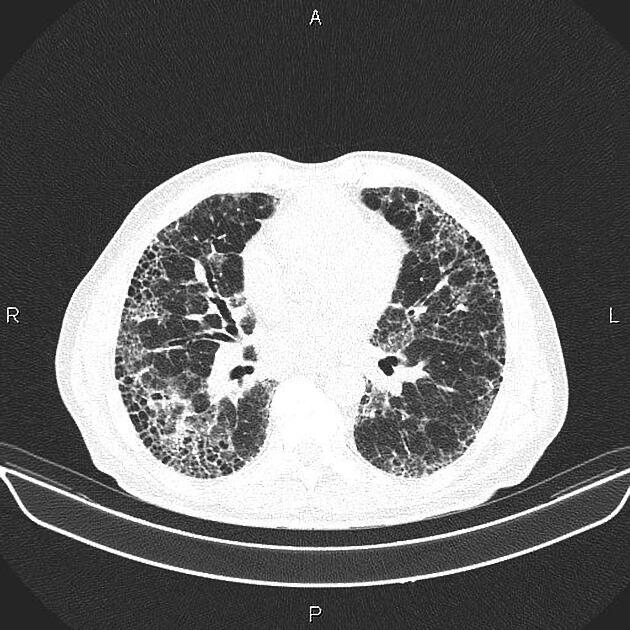
Typical UIP CT pattern
-
distribution
basal predominant (occasionally diffuse)
subpleural predominant
often heterogeneous
-
features
reticulation with peripheral bronchiectasis or bronchiolectasis
absence of features suggesting an alternative diagnosis
the presence of this pattern, in the correct clinical setting, permits a confident diagnosis of IPF (idiopathic pulmonary fibrosis)
if the clinical setting is equivocal for IPF, lung biopsy and further review in a multidisciplinary meeting are recommended
Probable UIP CT pattern
-
distribution
heterogenous basal
subpleural predominance
-
features
reticulation with peripheral bronchiectasis or bronchiolectasis
absence of features suggesting an alternative diagnosis
honeycombing is absent
the presence of this pattern, in the correct clinical setting, permits a confident diagnosis of IPF (idiopathic pulmonary fibrosis)
if the clinical setting is equivocal for IPF, lung biopsy and further review in a multidisciplinary meeting are recommended
CT pattern indeterminate for UIP
-
distribution
variable or diffuse
-
features
evidence of fibrosis with some inconspicuous features suggestive of a non-UIP pattern
diagnosis of IPF cannot be reached and lung biopsy and further review in a multidisciplinary meeting are recommended
CT features most consistent with non-IPF diagnosis
-
distribution
upper or mid lung predominant fibrosis
peribronchovascular predominance with subpleural sparing
-
features, any of the following:
predominant consolidation
predominant ground glass opacity without acute exacerbation
extensive mosaic attention with extensive sharply defined lobular air trapping on expiration
nodules
cysts
diagnosis of IPF cannot be reached and lung biopsy and further review in a multidisciplinary meeting are recommended
The paper also states that all patients with an IPF diagnosis should have it reviewed at periodic intervals.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.