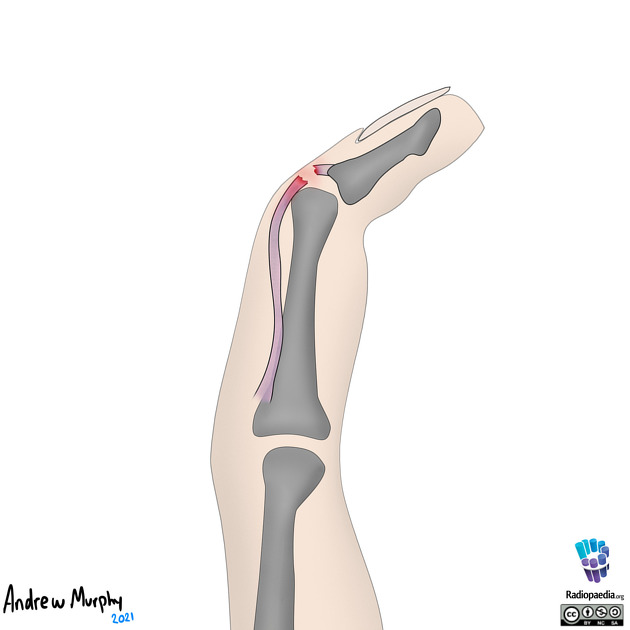
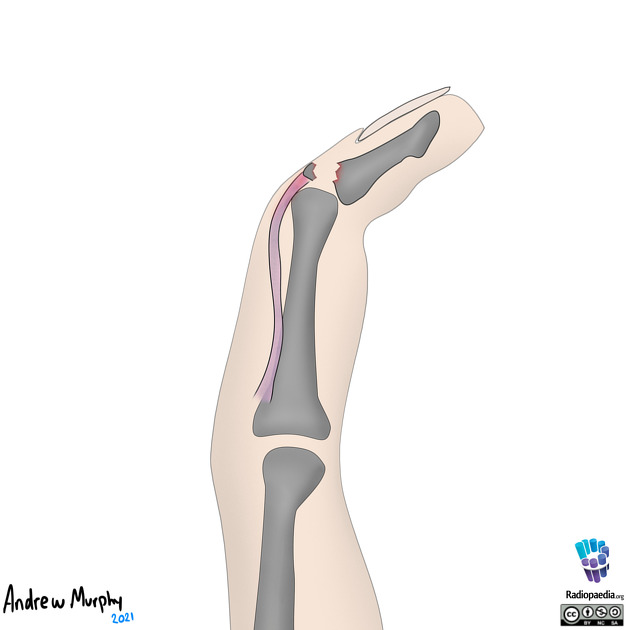
Mallet finger is an injury of the extensor mechanism of the finger at the level of the distal interphalangeal (DIP) joint. It is the most prevalent finger tendon injury in sport. It may represent an isolated tendinous injury or occur in combination with an avulsion fracture of the dorsal base of the distal phalanx.
On this page:
Clinical presentation
It is characterized by an inability to extend the finger at the distal interphalangeal (DIP) joint. There is slight flexion at this joint, which is where the term "mallet" comes from - the finger position resembles a mallet (for example, a piano key mallet).
The injury classically occurs while playing sports where the DIP joint undergoes sudden flexion (extended finger is struck at the tip by an object, e.g. baseball, basketball), or a crush injury (slamming a door towards the distal interphalangeal joint) in the extensor direction.
Pathology
The DIP joint is extended by combined pulling force of the terminal (lateral bands) of the extensor tendon, functioning together with the oblique retinacular ligament 7. Injury to these structures commonly results from direct axial or flexion loading of the DIP joint, as can occur by direct blow from a ball.
The terminal extensor tendon inserts on the DIP joint capsule, and so injurious force may also result in an intra-articular avulsion fracture of the base of the distal phalanx. This may represent an epiphyseal injury in skeletally-immature children 7.
Radiographic features
Plain radiograph
If there is a bony avulsion, a plain film will classically show a triangular avulsion fragment at the insertion of the common extensor tendon on the dorsal aspect of the distal phalanx at the DIP joint.
A high proportion of mallet finger injuries will present as isolated tendon injuries without any associated avulsions fractures known as a "mallet fracture" 5.
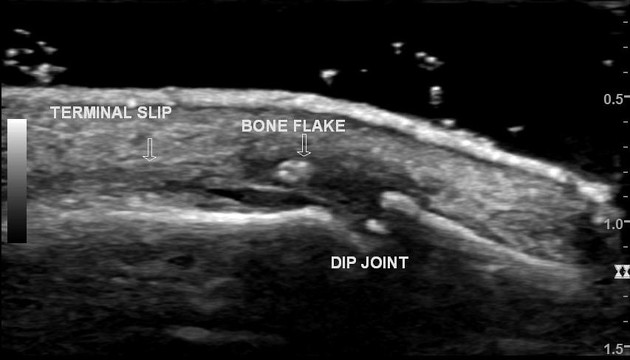
Ultrasound
The findings on ultrasound include 6:
loss of real-time movement of the tendon
complete or partial extensor tendon tears
fluid in the region of the extensor tendon insertion
avulsion fracture
Treatment and prognosis
The preferred treatment for closed mallet injuries is non operative treatment, using a splint to maintain the DIP joint in extension or slight hyperextension; the proximal interphalangeal (PIP) joint is kept mobile. This positioning causes approximation of the injured tendon ends, which usually heals by scarring over time and restores extension 7. Non-operative treatment would usually involve 6 weeks of full time splinting followed by 6 weeks of night splinting 8. It is also important to note that the DIP joint should be kept in full extension for the entire first 6 week period including times of hygiene.
It is uncommon for closed mallet finger injuries to require surgical intervention 5. Surgery is considered for avulsion fracture where the fragment is larger than 1/3 of the joint surface and there is more than 2 mm displacement, or there is volar subluxation of the distal phalanx which is not reducible in a splint.
The fragment may be pinned with a Kirschner wire (either percutaneously or following open reduction) or indirectly reduced by "door stop" technique with the DIP joint flexed and a stabilizing Kirschner wire placed through the middle phalanx 7. Post-operative complications, e.g. infection or need for further surgery, are common. The alternative is for fixation with a screw or hook plate if the fragment size will accommodate.
Open injuries are generally surgically explored to evaluate for additional tendinous injury.
Complications
the most common complication in mallet finger injuries are dorsal skin complications (including dorsal ulceration, nail deformities, and maceration of the skin), which are prevalent in both operative and non-operative cases 8
extensor lag
untreated mallet finger or incomplete healing may progress to a swan neck deformity that will require surgical intervention 3,4,7
development of secondary osteoarthritic changes 4






























 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.